|
Table of Content - Volume 20 Issue 2 - November 2021
Anatomical variations of Poupart’s ligament in relation to deep fascia of anterior abdomen wall and its clinical implications - A cadaveric study
Kosuri Kalyan Chakravarthi
Professor, Department of Anatomy, Varun Arjun Medical College and Rohilkhand Hospital, Banthra-Shahjahanpur, Uttar Pradesh, INDIA. Email: kalyankosuric@gmail.com
Abstract Background: Poupart’s ligament also called as inguinal ligament which extends from the anterior superior iliac spine to the pubic tubercle and is formed by the thickening of the lower boarder of the aponeurosis of external oblique muscle of abdomen. It is an important landmark in surgery for diagnosis and while performing inguinal surgery. Deep fascia is said to be absent in the anterior abdomen wall, because it is formed by collagenous fibrous membrane which is non-elastic and might prevent bulging of anterior abdomen wall. Aim: Accordingly, the aim of this study was designed to evaluate the prevalence of unusual anatomical variations of Poupart’s ligament in relation to the occurrence of deep fascia in the anterior abdominal wall. Methods and Materials: This study was carried out on routine human cadaveric dissection of abdomen conducted (Between 2009-2021) for medical undergraduates. Dissections were performed on a body that had been donated for the purpose of medical education and research to the laboratory of anatomy in accordance with the institutional ethical standards and Indian anatomy act. Unusual formation of Poupart’s ligament in relation to the deep fascia of abdomen were observed and photographs were taken. Results: Out of 62 human cadavers (male-35 and female-27), in 3 middle aged male cadavers following variations were observed- 1. Presence of well-defined thick deep fascia in the anterior abdomen wall and its bilateral formation of inguinal ligament with bilateral complete indirect inguinal hernia; 2. Presence of bilateral superficial inguinal ring in the deep fascia above the pubic crest; 3. Bilateral conjoined fleshy muscle origin of inguinal part of internal oblique and transverse abdominis from lateral two thirds of deep fascia’s inguinal ligament; 4. Bilateral intermingling of lower boarder of external oblique aponeurosis with the fleshy fibers of inguinal part of internal oblique muscle were observed. Conclusion: A rare and unusual bilateral anomalous formation of Poupart’s ligament with bilateral inguinal hernia noted in this study, have not been presented in the modern medical literature. Awareness and anatomical knowledge of these variations is essential not only to anatomists, but also to the radiologists, embryologists, and to the surgeons operating on groin hernias can increase the success of diagnostic evaluation and surgical approaches to the region. Key words: Deep fascia, indirect complete inguinal hernia, myofascial syndromes, Poupart’s ligament and processus vaginalis.
INTRODUCTION The anterior abdomen wall is musculo-fibrous and is formed by eight layers from before backwards skin, superficial fascia, external oblique muscle its aponeurosis, internal oblique muscle its aponeurosis, transversus abdominus muscle its aponeurosis, facia transversalis, extra-peritoneal tissue, and parietal peritoneum. Superficial fascia of the anterior abdomen wall consists of single layer above the line joining the two anterior superior iliac spines, below the line it splits into Camper’s facia (superficial layer) and scarpa’s facia (deep membranous layer). Deep fascia is absent in the anterior abdomen wall, because it is formed by collagenous fibrous membrane which is non-elastic and might prevent bulging of anterior abdomen wall. The most superficial muscle of anterior abdomen is external oblique muscle arises from eight fleshy slips from the outer surfaces and lower boarders of lower eight ribs. Most of its fleshy posterior fibers inserted on to the outer lip of the anterior two-third of the iliac crest and remaining fibers end in a broad aponeurosis. The upper boarder of aponeurosis is overlapped by the pectoralis major muscle, and its lower boarder thickened to form a Poupart’s ligament. Above the pubic crest the aponeurosis presents a tringle gap known as the superficial inguinal ring. Poupart’s ligament also called as inguinal ligament which extends from the anterior superior iliac spine to the pubic tubercle. Inguinal ligament was discovered by Gabrielle Falloppio in 1562 and further described by French anatomist Francois Poupart.1 The superior surface of the inguinal ligament is grooved and forms the floor of the inguinal canal and contains the ilioinguinal nerve and the spermatic cord in males and round ligament in females. Grooved upper surface of lateral two thirds of inguinal ligament give origin to internal oblique, lateral one third to the transverse abdominis. The ligament forms the base of the femoral triangle and bridges the neurovascular and muscular structures that pass from the deep pelvis to the thigh. Inguinal ligament is an important landmark in surgery for diagnosis and while performing inguinal surgery. Accordingly, the aim of this study was designed to evaluate the prevalence of unusual anatomical variations of Poupart’s ligament in relation to the occurrence of deep fascia in the anterior abdominal wall.
METHODS AND MATERIALS This study (Between year 2009-2021) was carried out on 62 human cadavers (male-35 and female-27), donated for the purpose of medical education and research to the laboratory of anatomy in accordance with the institutional ethical standards and Indian anatomy act. This study was reviewed and approved by the appropriate institutional review board (reference number: IRB AN Feb 017). While doing human cadaveric dissection of abdomen, anterior abdominal wall was observed carefully for anatomical variations of Poupart’s ligament in relation to deep fascia. Anatomical variations were noted and photographs were taken for proper documentation.
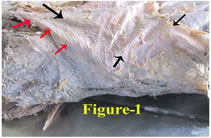
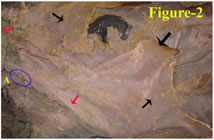
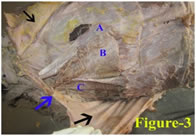
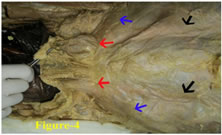
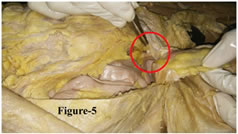
Out of 62 human cadavers (male-35 and female-27), in 3 middle aged male cadavers the following variations were observed. Bilaterally a well-defined thick deep fascia of anterior abdomen wall deep to the superficial fascia and superficial to the external oblique muscle was observed (Figure-1). Surprisingly the lower boarder of the deep fascia of anterior abdomen wall formed the Poupart’s ligament bilaterally, which extended from the anterior superior iliac spine to the pubic tubercle (Figure-2). The lower border of the external oblique aponeurosis intermingled with the fleshy fibers of inguinal part of internal oblique muscle (Figure-3). Deep facia of abdomen forming the upper grooved surface of inguinal ligament was given a conjoined muscle origin (inguinal part of internal obliqueand transverse abdominis) from its lateral two thirds. Lack of cremasteric muscle origin from the middle third of inguinal ligament was noted. Above the pubic crest the deep facia of abdomen presented bilaterally a triangular gap knows as the superficial inguinal ring (Figure-4 and Figure-5). Medially the deep fascia is continued with the opposite one in the midline, laterally with thoraco lumbar fascia, above with the pectoral fascia and below with the fascia lata (Figure-1 and Figure-2). Bilateral complete indirect inguinal hernia was observed. In which protrusion of small gut with peritoneal sac was extended from deep inguinal canal to the scrotum and prominent bulging was observed at the superficial inguinal ring (in the deep fascia of anterior abdominal wall) (Figure-4 and Figure-5).
DISCUSSION Deep fascia is a dense fibrous connective tissue that interpenetrates and surrounds the muscles, bones, nerves, and blood vessels of the body. Anatomically deep layer of pectoral fascia (deep fascia) above adherent to clavicular periosteum, whereas its superficial layer continues with the superficial lamina of investing layer of deep cervical fascia, which surrounds the sternocleidomastoid and the trapezius muscles. Medially the deep layer inserts into the sternal periosteum, while its superficial layer crosses the sternum in the midline and continues with the similar layer of opposite side. Distally the pectoral fascia is reinforced by some fibrous expansions originating from the rectus abdominis sheath and by the fascia of the contralateral external oblique muscles. Anatomically deep fascia is said to be absent in the anterior abdomen wall, a well-defined thick bilateral deep fascia in the anterior abdomen wall noted in this study might be due to abnormal downward continuation of the pectoral fascia during the embryonic development. Such unusual and rare presence of deep fascia in the anterior abdominal wall may prevents or interfere bulging of abdomen, which may lead to elevated intraabdominal pressure (Intraabdominal hypertension). Elevated intra-abdominal pressure is a common phenomenon, which occurs in various clinical conditions, like blunt or penetrating trauma, haemorrhage, abdominal aortic aneurysm rupture, intestinal obstruction, retroperitoneal hematoma, pregnancy, ascites, liver cirrhosis, ileus, burns, intra-abdominal sepsis, and large-volume fluid replacement.2-6 Deep fascia was originally considered to be essentially avascular, however recent investigations confirmed a rich presence of thin blood vessels. Figure 1 Figure 2
Figure 3 Figure 4 Figure 5 Figure 1: Showing well-defined thick deep fascia in the anterior abdominal wall; Figure-2: Showing well-defined thick bilateral deep fascia and its inguinal ligament in the anterior abdominal wall; Figure 3: Showing muscles of anterior abdominal in relation to wall well-defined thick deep fascia; Figure 4: Showing bilateral indirect complete inguinal hernia.; Figure 5: Showing indirect complete inguinal hernia at deep inguinal ring. Black arrows- Deep fascia; Blue and Red arrows- Deep fascia’s Inguinal ligament; A- External oblique muscle; B- Internal oblique muscle; C- Transversus abdominus muscle; Red arrows (Figure-4)- bilateral indirect complete inguinal hernia; Blue circle (A)-Superficial Inguinal Ring; Red circle- loops of small intestine along with peritoneum protruding in to the inguinal canal through deep inguinal canal.
Deep fascia is potential source of pain in different pathologies and various pain syndromes as it is richly innervated by sensory receptors which contribute proprioception, nociception and may be responsive to manual pressure, temperature and vibration. With overuse or injury or irritation to the deep fascia may get tighten and contract creating undue pressure on underlying muscles and may results in musculoskeletal pain or myofascial syndrome. Awareness of deep fascia in the anterior abdominal wall observed in this study can help the clinician in diagnosis and treating in different myofascial syndromes. Vital structures of the human musculoskeletal system are bones, cartilage, ligaments and tendons. Bones and cartilage provide structural framework for the body while ligaments and tendons perform the important function of supporting the bones which help us to move and carry out various physical activities. Anatomically inguinal ligament is formed by the inward folding of lower boarder of the aponeurosis of external oblique muscle of abdomen. In this study the lower boarder of the deep facia of anterior abdomen formed the inguinal ligament bilaterally, and the lower border of the external oblique aponeurosis intermingled with the fleshy fibers of internal oblique muscle. Such unusual inguinal ligament formed by the deep fascia may disturb the flexibility of the hip region which can leads to compression of femoral vessels, lateral femoral cutaneous nerve and femoral nerve or may interfere the action of external oblique muscle. Such unusual and rare anatomical variations of inguinal ligament have not been cited in modern literature. Awareness and anatomical knowledge of these variations can help the clinician in quick diagnostic evaluation and surgical approaches to the region. External oblique muscle of abdomen forms the anterior wall of inguinal canal, in increased intraabdominal pressure it approaches close to the posterior wall of inguinal canal and obliterates the inguinal canal like a flap-valve and prevents inguinal hernia. Presence of deep facia and its inguinal ligament superficial to the external oblique muscle observed in this study may interfere the biomechanics of external oblique muscle and may increase susceptible to inguinal hernia. Acquiring such detailed knowledge of inguinal ligament is essential for surgeons operating on groin hernias. Cremaster is a paired striated muscle of the pelvis and perineum that is fully developed only in the male external genitalia. Anatomically, it originates from the internal oblique and grooved upper surface of middle of the inguinal ligament. This muscle surrounds the spermatic cord and runs from the deep inguinal ring to the testicle. It lowers and raises the testis closer to the body in order to control its temperature and protects the testes and sperm cells from the negative environmental factors. In increased intraabdominal pressure contraction of cremasteric muscle pulls the testis up toward the superficial inguinal ring, closes the outlet of inguinal canal like a plug (ball-valve action) and prevents the inguinal hernia. Origin of cremasteric muscle from the middle third of inguinal ligament noted as absent in this study may weakens the functions of cremasteric muscle and may leads to inguinal hernia. Hernia generally means weakness or defect of the body wall muscle fibers that provide a space for protrusion of internal organs. The lifetime risk of groin hernia the inguinal or femoral canal is 27 to 43%in men and 3 to 6% in women.7,8 According to the previous studies, prevalence of the inguinal hernia is nearly 5% worldwide. 9 Inguinal hernia is divided into two categories, indirect and direct which include 24 and 50 percent of all types of hernia, respectively. 10 Indirect inguinal hernia is caused by a birth defect in the abdominal wall that is congenital and direct inguinal hernia develops by a weakness in the abdominal muscles over time in adult life due to straining or heavy weight lifting. At about seventh week of intra-uterine life testis begins to develop from the genital ridge. During the 4th month of foetal life, the testis appears in the iliac fossa, and reaches the deep inguinal ring at about the 7th month. During the 7th and 8th months they rapidly traverse the inguinal canal, and at or shortly after birth it finally reaches the scrotum. Gubernaculum a fibromuscular band also called as caudal genital ligament which stretches from the lower pole of testis to the scrotum and plays an important role in the descent of testis.11,12The processus vaginalis is the peritoneum invagination into the space created by the gubernaculum through which the testes migrate from the retroperitoneum towards the scrotum during embryological development. Proximal part of Processus vaginalis becomes obliterated in a superior-to-inferior direction around the time of birth and disappears. In females, the processus normally leaves no remnant in the adult. In males, normally only the scrotal portion of the processus remains to form the tunica vaginalis testis.13Bilateral complete indirect inguinal hernia observed in this study may be due complete patent processus vaginalis or due to presence of thick deep facia in the abdomen or due to weakness and dilatation of larger deep inguinal canal, as per review of literature such multiple and bilateral anatomical variation were not cited in the modern medical literature.
CONCLUSION Well-defined thick deep fascia in the anterior abdominal and its inguinal ligament formation with bilateral indirect complete inguinal hernia observed in this study are very important clinically. As per literature survey such anatomical variations have not been presented in the modern medical literature. Such detailed anatomical variations knowledge is essential not only to anatomists, but also to radiologists, embryologists, and to the surgeons operating on groin hernias can increase the success of diagnostic evaluation and surgical approaches to the region.
REFERENCES
Policy for Articles with Open Access
|
|
 Home
Home