Official Journals By StatPerson Publication
|
Table of Content - Volume 10 Issue 1 -April 2019
A study of phrenic nerve paralysis after vertical infraclavicular brachial plexus block
Kiran Sonawane1, Hemant Patil2*
1Assistant Professor, Department of Anaesthesiology, Government Medical College, Jalgaon, Maharashtra, INDIA. 2Private Practitioner, Jalgaon, Maharashtra, INDIA. Email: drkiran6669@gmail.com
Abstract Background: Peripheral nerve blocks are gaining widespread popularity for perioperative management because of their distinct advantages over general and central neuraxial anaesthesia. Infraclavicular brachial plexus block (ICPB) was introduced in early 20th century as an alternative to axillary and supraclavicular approaches. The vertical infraclavicular brachial plexus block (VIB) has become well known. In performing this block, the needle is inserted anteroposteriorly, immediately caudal to the middle of the clavicle. Phrenic nerve palsy may occur in this approach with varying incidence depending upon site of block. Aims and Objectives: To study the diaphragmatic paralysis due to phrenic nerve paralysis after vertical infraclavicular brachial plexus block. Materials and Method: In the present study total 50 ASA physical status grade I and II Patients were included. Recording of detailed history, physical examination and routine laboratory tests were performed in all the selected patients. Patient was explained the procedure and informed consent was taken. End- Inspiratory X-ray chest film was obtained preoperatively and the same was reported by hospital radiologist. Standard protocol and procedure was used for inducing the vertical infraclavicular brachial plexus block. Diaphragmatic movement was observed after deep inspiration on fluoroscopic C–ARM machine to note whether there was restricted, paradoxical or absent movement of diaphragm. The pre procedure movement of diaphragm after deep inspiration on right side and left side was noted. Results: Majority of the study patients in the present study were in age group of 19-30 years of age (56%) followed by 31-50 years of age (32%). Majority of the study subjects were male (70%) with male: female ratio of 2.33:1. It was seen that 80% patients were of ASA grade I and 20% were of ASA grade II. Preoperative and postoperative fluoroscopy was performed in all the cases and it was seen that normal movement of diaphragm on right and left sides was present in the all patients. Restricted, paradoxical, or absent movement of diaphragm was seen in none of the patient. It was observed that on right side mean preoperative and post operative Diaphragmatic movement was 2.486 cm and 2.462 cm respectively and the difference observed was not statistically significant. Similarly the mean preoperative and post operative Diaphragmatic movement on left side was 2.080cm and 2.068cm respectively and the difference was not significant. Comparison of both X –ray showed no evidence of elevated diaphragm in any patients after vertical brachial plexus block approach. Preoperative and post operative Diaphragmatic movement was measured on x ray and compared. The X-ray chest showed normal position and contour of diaphragm preoperatively and postoperatively. Conclusion: Thus with reference to above results and discussion we ruled out diaphragmatic involvement due to phrenic nerve paralysis after VIB Plexus block approach. Thus VIB is a newer but useful technique of giving blocks to upper limb surgeries with less complication like phrenic nerve paralysis. Key Word: vertical infraclavicular brachial plexus block, phrenic nerve paralysis.
INTRODUCTION Peripheral nerve blocks are gaining widespread popularity for perioperative management because of their distinct advantages over general and central neuraxial anaesthesia. Infraclavicular brachial plexus block (ICPB) was introduced in early 20th century as an alternative to axillary and supraclavicular approaches. However, this approach was not utilised despite its advantages of less complications and more consistent block until Raj et al. introduced this in 1973.1 But Raj’s technique could also not gain widespread use probably due to unreliable results2 and lack of precision in needle placement.3 Since then several variations on the technique of ICPB have been described with various surface landmarks, site of needle insertion and recommendations for needle direction.4-6 The vertical infraclavicular brachial plexus block (VIB) has become well known.4,7,8 In performing this block, the needle is inserted anteroposteriorly, immediately caudal to the middle of the clavicle. The plexus is expected to be found at a depth of 3–4 cm, and the pleura is expected to be found at levels deeper than 6 cm.7 Although the first rib may serve as a backstop for the needle approaching the lung4, the risk of pneumothorax 8-10 and puncture of the subclavian vessels has been questioned. Finally, when performing VIB, we occasionally have found difficulty in palpating the ventral acromial process one of two landmarks for defining the needle insertion point. Brachial plexus is formed by anterior primi rami of C5, C6, C7, C8 and T1. It may be prefixed (C4) or postfixed (T2) as variant. Brachial plexus involves roots, trunk, divisions, cords and further peripheral nerves. So it can be blocked at various levels such as interscalanae, supraclavicular, infraclavicular, and axillary or different peripheral nerve blocks. Phrenic nerve palsy may occur in these approaches with varying incidence depending upon site of block. Prior studies showed less incidence of phrenic nerve palsy with infraclavicular block than interscalanae or supraclavicular block. With this background we have decided to study incidence of phrenic nerve paralysis with vertical infraclavicular brachial plexus block to further elaborate it.
MATERIALS AND METHOD: The present study was conducted to study the diaphragmatic paralysis due to phrenic nerve paralysis after vertical infraclavicular brachial plexus block. For the purpose of study following inclusion and exclusion criteria was used to select the study subjects. Inclusion Criteria:
Exclusion Criteria:
With respect to the above mentioned inclusion and exclusion criteria total 50 patients were included in our study. Study Procedure: Recording of detailed history, physical examination and routine laboratory tests were performed in all the selected patients. Patient was explained the procedure and informed consent was taken. End- Inspiratory X-ray chest film was obtained preoperatively and the same was reported by hospital radiologist. The study procedure was performed with patients in supine position. Standard monitors like manual BP, Cardioscope, and Pulse oximeter were attached and readings noted. Intravenous line was secured on the opposite arm. Further diaphragmatic movement after deep inspiration was observed on fluoroscopy with C- arm Machine (Siemens’). Since we were judging phrenic nerve paralysis by diaphragmatic levels, we monitored diaphragmatic movement after deep inspiration with C-arm machine preprocedure and postprocedure. Patients were sedated with inj Midazolam 0.05 mg/kg, analgesia with inj Fentanyl 2mg/kg intravenously. Patient lying supine head turned to the opposite side with the arm to be anesthetized kept by the side of the body. The clavicular area cleaned and draped with all aseptic precautions. Standard protocol and procedure was used for inducing the vertical infraclavicular brachial plexus block. Block performed time was noted. Extent of block was assessed periodically. After 20 mins the extent of sensory and motor blocks was documented and surgical preparation was commenced. Diaphragmatic movement was observed after deep inspiration on fluoroscopic C-ARM machine to note whether there was restricted, paradoxical or absent movement of diaphragm. The pre procedure movement of diaphragm after deep inspiration on right side and left side was noted. Also the post procedure movement of diaphragm after deep inspiration on right side and left side was noted. Intraoperatovely Pulse, BP, Saturation, Respiration and ECG were monitored and all were within normal limit. Patient was enquired about intraoperative and postoperative difficulty in breathing. Postoperatively end Inspiratory X-ray chest film was obtained and reported by hospital radiologist. Comparison of preoperative and postoperative X-ray chest was done to look for elevated ipsilateral diaphragm to rule out phrenic nerve paralysis due to VIB. Data Collected and statistical analysis done with IBM SPSS statistical software.
RESULTS The present study was conducted in the department of anesthesia of the study institute. The study included total 50 patients of ASA grade I and II physical status and above 18 years of age undergoing elective and emergency upper limb surgery. Table 1: Demographic distribution of patients:
It was seen that majority of the study patients in the present study were in age group of 19-30 years of age (56%) followed by 31-50 years of age (32%). Majority of the study subjects were male (70%) with male: female ratio of 2.33:1. It was seen that 80% patients were of ASA grade I and 20% were of ASA grade II.
Table 2: Preoperative and postoperative fluoroscopy
Preoperative and postoperative fluoroscopy was performed in all the cases and it was seen that normal movement of diaphragm on right and left sides was present in the all patients. Restricted, paradoxical, or absent movement of diaphragm was seen in none of the patient
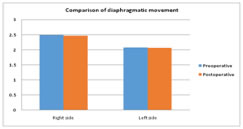
Table 3: Comparison of diaphragmatic movement after VIB plexus block on right and left side
It was observed that on right side mean preoperative and post operative Diaphragmatic movement was 2.486 cm and 2.462 cm respectively and the difference observed was not statistically significant. Similarly the mean preoperative and post operative Diaphragmatic movement on left side was 2.080cm and 2.068cm respectively and the difference was not significant. Table 4: Comparison of diaphragmatic movement by X-ray chest preoperatively and postoperatively
Comparison of both X–ray showed no evidence of elevated diaphragm in any patients after vertical brachial plexus block approach. Preoperative and post operative Diaphragmatic movement was measured on x ray and compared. The X-ray chest showed normal position and contour of diaphragm preoperatively and postoperatively.
DISCUSSION Infraclavicular brachial plexus blocks are gaining widespread popularity due to less incidence of phrenic nerve paralysis than interscalene and supraclavicular brachial plexus blocks. The present study was conducted to evaluate the phrenic nerve paralysis after VIB plexus block approach. For this purpose total 50 patients were enrolled out of which 80% were ASA physical status grade I and 20% patients were of grade II. Majority of the patients were in age group of 19-30 years of age (56%) followed by 31-50 years of age (32%) and out of which 70% were male and 30% were female patients. Preoperative and postoperative fluoroscopy showed normal movement of diaphragm on both sides of chest. Restricted, paradoxical, or absent movement of diaphragm was seen in none of the patient. In most patients the diaphragm lied at the level of 5thand 6th intercostal space. In Lennon F A et al11study, in most patients the diaphragm in the mid lung field lies at the level of 5th or 6th interspaces. On right side it was in 5th intercostal space and on left side it was on 6th intercostal space. The preoperative average movement of diaphragm on right side was 2.486 cm and left side was 2.080 cm. The postoperative average movement of diaphragm on right side was 2.462 cm and left side was 2.068 cm. The difference observed in diaphragm movement preoperatively and postoperatively on right and left side was not significant statistically by application of paired t test. The diaphragm moves in vertical plane and in quiet respiration is responsible for the major part of tidal exchanges. The exact extent to which it moves has been studied radiographically. Wade et al12 gives it a range of about 1.5 cm upwards or downwards during quite respiration, but the distance may be extended to 6-10 cm with deep breathing. In most people, the right hemidiaphragm is 1.5-2.5cm higher than the left, but the two hemidiaphragm are at the same level in some 9% of the population. In a few normal individuals the left hemidiphragm is upto 1 cm higher than right. The normal excursion of diaphragm is usually between 1.5 cm and 2.5 cm through greater degree of movement is not uncommon observed by Lemon et al11. Postoperative end Inspiratory X-ray chest compared with preoperative X-ray chest showed normal position and contour of diaphragm. There was no elevation of diaphragm on the side of block performed in any patient. Unequal excursion of the two hemidiaphragm occurs in approximately 80% of normal people. According to Alexander et al13, the left side is usually dominant, while Simson et al14, stated that the right side usually exhibits the greater excursion. In either event, this inequality of diaphragm excursion is less than 10mm in most people. While normal young adults can move the diaphragm over at least 30mm, this range is greatly reduced in the elderly. The etiology of phrenic nerve block following brachial plexus anaesthesia carried out above the clavicle is twofold. It may result from diffusion of local anaesthetic cephalad to involve the more proximal cervical roots (C3, C4, C5) or may also be consequences of an improperly performed block with local anaesthetic deposited outside the brachial plexus sheath anterior to the anterior scalene muscle. Both etiologies result in decreased mobility of the hemidiphragm ipsilateral to the side in which the regional block was performed. The single chest X-ray taken following inspiration may demonstrate a raised left or right hemidiaphragm but, unlike the double-exposure technique, does not indicate diaphragmatic movement between inspiration and expiration. Two single chest X-ray one taken following inspiration and one following expiration, can also demonstrate phrenic nerve block, but difficult to compare because of differences in technique and degree of respiratory variation between the two films. Sebastien Robux et al15 reports a case of permanent phrenic nerve paralysis with hemidiaphragmatic palsy after interscalene brachial plexus block. Bashein et al16 reported a case of hemidiaphragmatic paralysis after interscalene block performed using a paraesthesia technique as described by Winnie et al17. These authors suggested that phrenic nerve paralysis was related to a direct needle trauma. Accidental, temporary blockade of the phrenic nerve occurs in 36% of patients having interscalene brachial plexus block, but long-lasting injury to the phrenic nerve has not been reported. He describes a phrenic nerve paresis that has persisted more than 3 yrs. following an interscalene brachial plexus block. Wilson et al5 described in 1998 an infraclavicular coracoid approach that has since then adopted in our community hospital. Thus in our study, there was no case of diaphragmatic paralysis due to phrenic nerve involvement after VIB approach by all above criteria.
CONCLUSION Thus with reference to above results and discussion we ruled out diaphragmatic involvement due to phrenic nerve paralysis after VIB Plexus block approach. Thus VIB is a newer but useful technique of giving blocks to upper limb surgeries with less complication like phrenic nerve paralysis.
REFERENCES
|
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
 Home
Home