Official Journals By StatPerson Publication
|
Table of Content - Volume 10 Issue 1 -April 2019
Dexamethasone as an adjuvant to ropivacaine in supraclavicular brachial plexus block
Shailendra Patil1*, Kashinath Jadhav2, Vaishali Bapat3, Rajesh Pawar4
1Assistant Professor, 2Associate Professor, 3Hod & Professor, 4Senior Resident, Department of Anaesthesia, BKL Walawalkar Rural Medical College, Sawarde, Chiplun, Maharashtra, INDIA. Email:drsbp26@gmail.com
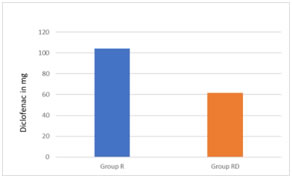
Abstract Background: Different adjuvants have been added to local anesthetic to augment the duration of supraclavicular brachial plexus block. This study was done to study the adjuvant effect of dexamethasone when added with 0.5% Ropivacaine in supraclavicular brachial plexus block. Objective: The objective of the study was to evaluate onset of sensory and motor blockade, duration of analgesia and motor blockade with dexamethasone as an adjuvant to ropivacaine in patients undergoing upper limb surgeries by supraclavicular brachial plexus block. Materials and Methods: After ethics committee approval this randomized, double-blinded, control study was conducted in the Department of Anaesthesiology, BKL Walawalkar Rural Medical College, Sawarde from July 2018 to November 2018. A total of 50 patients who met the inclusion criteria were enrolled into the study and were randomized to receive plain ropivacaine and ropivacine with dexamethasone. Group R (control group) patients (n = 22) received 35 ml of 0.5% ropivacaine with normal saline (2 ml) whereas Group RD (study group) patients (n = 23) received 35 ml of 0.5% ropivacaine with 8 mg dexamethasone (2 ml). Five patients (three patients in group R and two patients in group RD) failed to achieve satisfactory levels of anaesthesia and required induction of general anaesthesia and were excluded from the study. The primary outcome was measured as duration of analgesia that was defined as the interval between the onset of sensory block and the first request for analgesia by the patient. The duration of motor blockade was also noted in the post-operative period. The secondary outcome included visual analogue scale (VAS) hourly for first 6 hours and then two hourly till 24 hours, time of first analgesia (TFA), total rescue analgesia consumption, and side effects, if any. There was no statistically significant difference in the onset of sensory and motor blockade between both the groups. The mean duration of sensory blockade in group RD was 834±78.1min and in group R was found to be 276±38.73 min and was statistically significant (P ≤ 0.001).The mean duration of motor blockade in group RD was 376.4±39.99 min and in group R was 175.2±26.94 min and was statistically significant (P ≤ 0.001) .In Group R, patients required first rescue analgesia at 8 hour (480 ± 28.44 min) while in Group RD, patients required first rescue analgesia at 18hour 10min(1086.63±34.90min), which was found statistically significant (p< 0.0001). Group R patients received larger amount of Diclofenac as rescue analgesia(104.34 mg versus 81.81mg in Group RD) which was statistically significant (P 0.0099). Conclusion: We conclude that addition addition of dexamethasone to Ropivacaine in brachial plexus block significantly prolongs the duration of analgesia and motor block in patients undergoing upper limb surgeries and is a remarkably safe method of providing postoperative analgesia. Key Word: Adjuvant, Supraclavicular Brachial plexus, Dexamethasone, Ropivacaine
INTRODUCTION Brachial plexus block is a popular and widely employed regional nerve block of the upper extremity. Regional nerve block avoids the unwanted effects of anaesthetic drugs used during general anaesthesia and the stress of laryngoscopy and tracheal intubation. Minimizing the stress response and using minimal anaesthetic drugs is always beneficial for patients with various cardiorespiratory comorbidities. Various approaches to brachial plexus block have been described but supraclavicular approach is the easiest and most consistent method for anaesthesia and perioperative pain management in surgery below the shoulder joint. Pneumothorax, Hemothorax, Horner’s syndrome and phrenic nerve block are the potential complications of supraclavicular brachial plexus block.1Drugs like morphine, pethidine, clonidine, dexmedetomidine, have been used as adjuvant with local anaesthetics in brachial plexus block to achieve quick, dense and prolonged block. Since morphine, buprenorphine, pethidine, dexmedetomidine are associated with side effects of sedation, respiratory depression, drugs with minimal of these side effects are always looked for. Dexamethasone was selected as an adjuvant to local anaesthetics in brachial plexus block in our study because it has been reported to prolong duration of action of local anaesthetics and respiratory depression is not a major problem.
AIMS AND OBJECTIVESThe primary outcome was to compare the effect of addition of dexamethasone to 0.5% ropivacaine and 0.5% ropivacaine with normal saline in supraclavicular brachial plexus by studying onset and duration of sensory and motor blockade. Secondary outcome was to evaluate the efficacy of dexamethasone as an adjuvant in terms of visual analogue scale (VAS) pain score and consumption of rescue analgesia and note adverse effects such as nausea, vomiting, dysrhythmias, hypotension, convulsions, pneumothorax, horners syndrome, pruritus, and hypersensitivity reaction for the study drug.
MATERIAL AND METHODS Fifty patients (two groups of 25 each) of either sex, American Society of Anaesthesiology (ASA) Physical status class 1 and 2 in the age range of 18-70 years were enrolled in the study after obtaining approval from hospital ethics committee and written, informed valid consent from the patient at BKL Walawalkar Rural Medical College from July2018 to November 2018. Patients with history of uncontrolled diabetes, renal and liver disease, pregnant women, peptic ulcer disease, bleeding disorder, allergy to local anesthestic drugs and on long term steroid therapy were excluded from the study. All patients posted for upper extremity surgeries below the shoulder joint received ultrasound guided brachial plexus block by supraclavicular approach. Randomization was done by simple random sampling technique. Fifty patients were assigned a number. We used the table of random numbers to select each member of the sample. Double blinding was done by random assignment of the patient to case or control group. Anaesthesiologist administering the block was not informed about the group to which patient belonged. Key that identified the patients and the group they belonged to was kept by another independent observer and not given to the principal investigator until the study was over. Patients were allocated to one of the two groups Group RD (cases) & Group R (control). Patients in group RD received 2% adrenalized lignocaine (15ml) and 0.5% ropivacaine(18ml) plus dexamethasone 8mg(2ml) making a total volume of 35ml and patients in group R received 2% adrenalized lignocaine (15ml) and 0.5% ropivacaine(18ml) plus 0.9% normal saline (2ml) making a total volume of 35ml.Drug solutions were prepared by an independent anaesthesiologist not involved in the study. In the operation theatre after establishing 18 gauge intravenous access in the contralateral hand, vital parameters were observed throughout the procedure and oxygen at the rate of 4 l/min administered through oxygen mask. The brachial plexus block was carried out after thorough explanation of the procedure and emphasizing the need for patient cooperation. We used the in-plane needle approach to supraclavicular block using a single-injection, by Philips Nerve Ultrasound System using linear probes (6–15MHz). Supraclavicular brachial plexus block was performed under strict aseptic precautions with the patient in supine position and head turned slightly to the opposite side. A small pillow was placed in between the shoulders. The arm to be anesthetized was adducted and hand extended along the side toward the ipsilateral knee as far as possible. After injecting a small amount of 1% lidocaine to anaesthetise the skin, short bevel needle was inserted along the longitudinal axis of the ultrasound probe (in-plane needle approach),the needle tip and shaft continuously visualized in real time to avoid inadvertent pleural puncture. Needle was inserted lateral to the probe aiming medially and advanced towards the junction of the subclavian artery and first rib. Half of the local anaesthetic was injected in the area, commonly referred to as ‘‘the corner pocket.’ which is inferomedial to the plexus, posterolateral to the subclavian artery, and superior to the first rib in small 5-mL aliquots with repeated aspiration to reduce the risk of intravascular injection. The needle was then redirected towards the superficial aspect of the plexus or middle of the cluster, and the remaining local anaesthetic injected there. During the conduct of block and thereafter, the patient was observed vigilantly for any complications of the block and for the toxicity of the drugs injected. The time from injection to onset of analgesia in each of the major peripheral nerve distributions (ulnar, radial, medial and musculocutaneous) was defined as onset of sensory block & it was assessed by pinprick using the blunt end of a 27-gauge needle at 0, 2, 5,10, 15, 20, and 30 min. Sensoryblock was graded according to the following scale: 0 = no block(normal sensation), 1 = partial block (decreased sensation),and 2 = complete block (no sensation). The time from injection to the inability of the patient to move his/her fingers or raise their hand was defined as onset of motor block & it was measured at 0, 10, 20, and30 min by assessing the following motor functions: flexion at the elbow (musculocutaneous nerve), extension of the elbow and the wrist (radial nerve), opposition of the thumb and indexfinger (median nerve), and opposition of the thumb and smallfinger (ulnar nerve). Motor block was graded according to the following scale: 0 = no block (full muscle activity),1 = partial block (decreased muscle activity), and 2 = complete block (nomuscle activity).During the procedure, anaesthesia was considered satisfactory if the patient did not complain of any pain or discomfort and if no sedation was necessary. Postoperative follow up was carried out in the recovery and post operative ward. The duration of analgesia was noted according to 0-10 visual analogue score (VAS) for pain hourly for first 6 hours and then two hourly till 24 hours. When the patients began to experience the worst pain (VAS=6-8), it was considered that analgesic action of the drugs was terminated and rescue analgesic iv Diclofenac (1mg/kg) was given. The duration of motor block postoperatively was assessed every hourly by asking the patients to move their fingers and to see whether they are able raise the hand or not. This time was recorded and taken as cessation of motor block effect. Incidence of drowsiness, pruritus, nausea, vomiting, Horner’s syndrome, phrenic nerve palsy, pneumothorax, respiratory depression and sign and symptoms for local anaesthetic toxicity were looked for and noted, if any. The above assessments were carried out by the principal investigator who was blinded to the drugs administered in the plexus block. In the circumstance of inadequate or patchy action of the block, the block would be supplemented with general anaesthesia and the patient excluded from the study. If in case surgery was unduly prolonged and the effect of the block wore off, rescue analgesia with IV propofol would be given and the patient excluded from the study. Statistical Analysis: In this study, sample size was calculated using formula n = 4pq/E 2 which is based on Hardy-Weinberg principle. In this formula, P is the prevalence of upper limb surgery at our institute. Statistical analysis was carried out using Microsoft Office Excel 2010 and SPSS version 20. The data were analyzed using Chi-square test with Yates's correction and Fisher's exact test (two-tailed) for qualitative and Student's unpaired t test for quantitative data. P < 0.05 was considered to be statistically significant, P < 0.001 was taken as highly statistically significant, and P > 0.05 was considered to be nonsignificant.
OBSERVATIONS AND RESULTS The study conducted consists of two groups; Group RD (cases i.e. with dexamethasone) and Group R (Control i.e. without dexamethasone), with 25 patients undergoing upper limb surgeries below shoulder in each group (n=25 in each group). Five patients (three patients in group R and two patients in group RD) failed to achieve satisfactory levels of anaesthesia and required induction of general anaesthesia. They were excluded from the study. The two groups were comparable with respect to age, weight, height, ASA grade & duration of surgery (Figure 1).
Table 1: Demographic Data
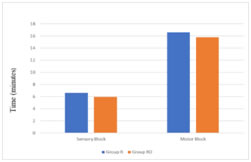
The time from injection to onset of analgesia in each of the major peripheral nerve distributions (ulnar, radial, medial and musculocutaneous) was defined as onset of sensory block. The time from injection to the inability of the patient to move his/her fingers or raise their hand was defined as onset of motor block. There was no statistical significant difference in onset of sensory & motor block between two groups as shown in figure 2 Table 2: Block Characteristic
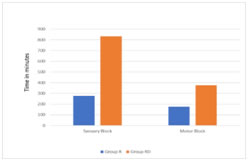
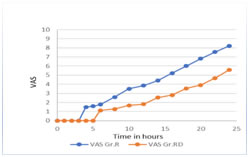
Figure 1: Onset of Sensory & Motor blockade Figure 2: Duration of Sensory &Motor Block between Groups Duration of analgesia was taken as time from the onset of sensory blockade to the reappearance of pain. The mean duration of analgesia (sensory block) was significantly prolonged in Group RD as compared to Group R (834±78.1min versus 276±38.73min), (p < 0.0001) as shown in figure 1 & figure 2. The duration of motor block in group RD was significantly more than that of group R (376.4±39.99 min versus 175.2±26.94 min)as shown in figure 2. VAS score was zero in both the groups in the immediate postoperative period and remained as such up to 4 hours of postoperative period.The mean VAS score was 1.5 ± 0.5 at the end of 4 hour in Group R, while it was 0 (zero) in Group RD at the same time. The difference was statistically highly significant (P< 0.001)
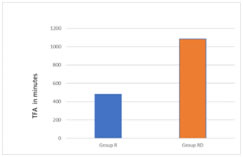
Figure 3: Comparison of VAS between Group RD and Group R Figure 4:Comparison for time of first analgesic between Group R & Group RD
Figure 5: Comparison for Diclofenac requirement between Group R & Group RD Out of 50 patients who were given supraclavicular brachial plexus block, we did not observe any complication of the block or the toxicity of the local anaesthetic drugs. We encountered just one case of Horner’s syndrome which subsided itself after few hours.
DISCUSSION Supraclavicular block provides a rapid, dense and predictable anesthesia of the entire upper extremity in the most consistent manner of any brachial plexus technique. It is the most effective block for all the portions of the upper extremity and is carried out at the “division” level of the brachial plexus; with high volume the “trunk” level of the plexus may also be blocked in this approach.2,3 Any method of postoperative pain relief must meet three basic criteria. It should be effective, safe, and feasible. Currently available local anaesthetics can provide analgesia for limited period of time when used as single injection. To extend the analgesia period beyond the operating rooms, various methods have been tried with the aim of prolonging the local anaesthetic action, like continuous infusion of local anaesthetics via indwelling catheters, use of different additives in local anaesthetics. Our study showed that there was no significant difference in the onset time of sensory and motor block between two groups. Similar observations in terms of time taken for onset of the sensory and motor blockade were made by Shrestha BR et al4, Ali Movafegh et al5 VAS score was used to assess duration of analgesia every hourly in the first 6 hours and every 2nd hourly in the next 18 h. In our study, the patients belonging to dexamethasone group had no pain from 1st-5th hours, The VAS score remained within a range of 3-4 until 20 hours of post-operative period. The VAS score in both the groups were zero in the first 3 hours after initiation of block; later the VAS score in the control group started to rise progressively and by the 8th hour majority of the patients had inadequate pain relief necessitating rescue analgesia. Group R, patients required first rescue analgesia at 8 hour (480 ± 28.44 min) while in Group RD, patients required first rescue analgesia at 18hour10min. Our observations show that comparatively dexamethasone group had 3 folds prolonged post-operative analgesia with respect to the control group R resulting in significantly less requirement of rescue analgesic intravenous diclofenac. In our study, the mean duration of analgesia in group RD was 834±78.1 minutes whereas in group R it was 276±38.73 minutes and the mean duration of motor block in group RD and group R were 376.4±39.99 and 175.2±26.94 minutes. Both these data were highly significant statistically which demonstrated the multifold augmentation of the duration of analgesia and motor blockade by addition of dexamethasone to ropivacaine. Several studies have shown that addition 4-8 mg of dexamethasone to local anaesthetics effectively and significantly prolongs the duration of analgesia. Kopacz DZ et al6 found that addition of small amounts of dexamethasone to bupivacaine incorporated in microcapsules prolonged local analgesia compared with microcapsules with plain bupivacaine after subcutaneous administration in humans. In another study by Droger C et al7,it was found that incorporation of dexamethasone into bupivacaine microspheres significantly prolonged intercostal nerve block in sheep. These authors believe that there is a causative relationship between the suppression of inflammation and the remarkably longer duration of effect. The mechanism of the analgesia induced by corticosteroids is not fully understood. This effect is suspected to be mediated by their anti-inflammatory or immune-suppressive effects.8,9 Corticosteroids cause skin vasoconstriction on topical application. The vasoconstriction effects of topical steroids are mediated by occupancy of classical glucocorticoid receptors rather than by nonspecific pharmacological mechanisms.8,9 According to the traditional theory of steroid action, steroids bind to intracellular receptors and modulate nuclear transcription. However, dexamethasone produced a relatively rapid effect which cannot be explained by the above mechanism. Therefore, vasoconstriction, the presumed mechanism of action for epinephrine’s adjunctive effect on local anaesthetics, is probably not responsible for block prolongation by dexamethasone. Corticosteroids may have a local effect on the nerve; the dexamethasone effect may be related to this action.10Many authors believe that the block prolonging effect of dexamethasone is due to its local action and not a systemic one. They found that steroids produce analgesia by blocking transmission in nociceptive c-fibres and suppressing ectopic neuronal discharge. Local application of methyl prednisolone has been found to block transmission in c-fibres but not in a and B fibres.11 The effect was reversible, suggesting a direct membrane action of steroids. Steroids might bring about this effect by altering the function of potassium channels in the excitable cells.12There are others who believe that analgesic properties of corticosteroids are the result of their systemic effect.13The safety of dexamethasone use in a nerve sheath may raise some concerns. In animal experiments, repeated intrathecal injections of small-dose betamethasone and triamcinilone acetate did not induce spinal neurotoxicity.14 Nerve injury is a rare complication of dexamethasone injection, and it usually occurs in the context of needle trauma. In our study, one side effect which was observed was one case of Horner’s syndrome. It is a known complication of supraclavicular block and it subsided as the effect of block wore off. Offering pain relief to the patient during perioperative period eliminates the stress response to surgery and helps in smoother transition of the patient from surgery to the routine preoperative state. Our study has shown that addition of dexamethasone to Ropivacaine in the brachial plexus block, using supraclavicular approach, produced prolonged motor blockade and effective postoperative analgesia which lasted longer than that produced by local anaesthetics alone without any significant side effects.
CONCLUSION Addition of dexamethasone to local anaesthetic drugs in brachial plexus block significantly prolongs the duration of analgesia and motor block in patients undergoing upper limb surgeries and is a remarkably safe method of providing postoperative analgesia.
REFERENCES
|
|
 Home
Home