Official Journals By StatPerson Publication
|
Table of Content - Volume 10 Issue 1 -April 2019
A comparative study of intrathecal bupivacaine (3.5ml) with nalbuphine (0.6mg) and intrathecal bupivacaine (3.5ml) with nalbuphine (1.2mg) in lower abdominal surgeries
Ramesh Babu1, Prashanth Vadigeri2*, Mohan3, Lohit4, Sunil Kumar5, Rajashekar Mudaraddi6
1Associate Professor, 2Senior Resident, 3, 4Assistant Professor, 6Associate Professor, Department of Anaesthesiology, Navodaya Medical College and Hospital, Raichur, Karnataka, INDIA. 5 Assistant Professor, Department of Anaesthesiology, Raichur Institute of Medical Sciences, Raichur, Karnataka, INDIA. Email:rsjev6313@gmail.com
Abstract Background: Various adjuvants including opioids, have been used with local anaesthetics in spinal anaesthesia to reduce complications as well as to increase peri and postoperative analgesia. Nalbuphine is a semi synthetic opioid with mixed antagonist and k agonist properties. Objective: To compare 0.6mg VS 1.2mg of intrathecal inj. Nalbuphine with inj. bupivacaine heavy 0.5% 3.5cc to establish the most effective dose for maximum postoperative analgesia in lower abdominal and lower limb surgeries. Methodology: Patients were randomly allocated to one of two groups. They received either nalbuphine 0.6 mg (group A) or nalbuphine 1.2 mg (group B) diluted upto 0.5ml with normal saline, mixed with 17.5 mg of hyperbaric bupivacaine 0.5% (3.5 ml). Patients basal vital parameters were recorded preoperatively using multiparameter monitor in the O.T. Results: The difference in mean duration of sensory blockade in both groups was found to be not significant (p>0.05). Mean duration of onset of motor blockade in Group A was 80.1 ± 11.01 seconds and in Group B it was 79.02 ± 7.98. The difference in mean duration in both groups was found to be not significant (p>0.05). Two segment regression time showed that mean duration in Group A was 62.2 ± 7.1 seconds and in Group B it was 76.9 ± 6.19. The difference in mean duration in both groups was found to be statistically highly significant (p<0.001). The difference in mean duration of post operative analgesia in both groups was found to be statistically highly significant (p<0.001). Conclusion: Intrathecal Nalbuphine (1.2mg) added to Intrathecal Bupivacaine 0.5% heavy (17.5mg) provides prolonged postoperative analgesia without increasing risk of side effects. Further studies are required to determine optimal dosage of intrathecal Nalbuphine. Key Word:Spinal Anaesthesia; Nalbuphine; Bupivacaine, lower abdominal surgery
INTRODUCTION Spinal anaesthesia is a very commonly used anaesthesia technique for various lower abdominal and lower limb surgeries. This approach has various advantages like cost effectiveness, better performance, enhanced margin of safety, and also helps in providing good post-operative analgesia. The stress response associated with general anaesthesia and side effects of various drugs used for general anaesthesia were also blunted. Various adjuvants including opioids, have been used with local anaesthetics in spinal anaesthesia to reduce complications as well as to increase peri and postoperative analgesia. Nalbuphine is a semi synthetic opioid with mixed antagonist and k agonist properties1, 2. Previous studies have shown that Intrathecal administration of Nalbuphine produced a significant analgesia accompanied by minimal pruritis and respiratory depression. Various doses of Nalbuphine were tried but still there is a controversy about the most effective dose. In present study we have compared 0.6mg VS 1.2mg of Intrathecal inj. Nalbuphine with inj. bupivacaine heavy 0.5% 3.5cc to establish the most effective dose for maximum postoperative analgesia in lower abdominal and lower limb surgeries.
OBJECTIVE To compare 0.6mg VS 1.2mg of intrathecal inj. Nalbuphine with inj. bupivacaine heavy 0.5% 3.5cc to establish the most effective dose for maximum postoperative analgesia in lower abdominal and lower limb surgeries.
MATERIALS AND METHODS The study was approved by the local institutional ethics committee and written informed consent was obtained from all patients before participation. Sixty patients with ASA physical status I or II, aged 20-60 years, weighing 40- 80 kgs, scheduled for elective lower abdominal and lower limb surgeries, of duration less than 2 hrs, under subarachnoid block, were included in the study. Patients were randomly allocated to one of two groups. They received either nalbuphine 0.6 mg (group A) or nalbuphine 1.2 mg (group B) diluted upto 0.5ml with normal saline, mixed with 17.5 mg of hyperbaric bupivacaine 0.5% (3.5 ml). After overnight fasting, all the participants were premedicated with inj. Rantac 50mg i.v. 1 hour before surgery. Patients basal vital parameters were recorded preoperatively using multiparameter monitor in the O.T.Spinal block was performed with 25G Quincke’s spinal needle at the level of L3-L4 or L4-L5 intervertebral space, in the left lateral position, maintaining aseptic precautions. Following freeflow of CSF, drug was injected slowly over 10 seconds and patients were immediately placed in the supine position for surgery. I.V fluids were given intraoperatively as and when necessary. The onset of sensory blockade i.e. time taken from the end of injection to loss of pin prick sensation at L1 dermatome, onset of complete motor blockade i.e. time taken from the end of injection to development of grade II motor block (modified Bromage's criteria), two-segment regression time from highest level of sensory blockade, duration of complete analgesia i.e. time from the intrathecal injection to the first complain of pain, duration of motor blockade (time required for motor blockade to return to Bromage's grade 0 from the time of onset of motor blockade) were studied and recorded. The changes in pulse rate, systolic and diastolic blood pressure, oxygen saturation (SpO2) and respiratory rate were monitored and recorded at 0, 5,10, 20 and 30 min and thereafter at every 30-min intervals up to 120 min after subarachnoid Block. Any side effects in the form of intra or postoperative hypotension, bradycardia, sedation, respiratory depression, nausea and vomiting and pruritus were recorded and treated. Intensity of pain was assessed by visual analogue score at 0, 10, 15, 30 and 60 minutes and then at 30-min intervals till 300 min after injection or until the patient received a rescue analgesic. Patients reporting a visual analogue score 3 or more or demand analgesia, were given rescue analgesics in the form of injection Diclofenac 1.5mg/kg IM. RESULTS Table1: Comparative assessment of both groups
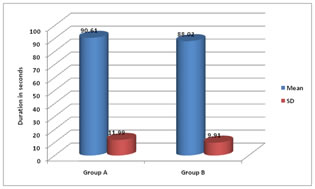
Mean age group of Group A was 39.2± 9.96 years and in Group B it was 42.46±10.8 years. The difference in mean age in both groups was found to be not significant (p>0.05).Mean weight in kg of Group A patients was 56.2± 7.1 and in Group B it was 57.2±5.2. The difference in mean weight in both groups was found to be not significant (p>0.05).Mean duration of surgery in Group A was 89.3 ± 15.9 minutes and in Group B it was 88.45 ±15.23 minutes. The difference in mean age in both groups was found to be not significant (p>0.05).t- 1.6, p- 0.87, not significant Mean duration of onset of sensory blockade in Group A was 90.61 ± 11.99 seconds and in Group B it was 88.02 ± 9.91. The difference in mean duration in both groups was found to be not significant (p>0.05). It means there is a small difference in both groups.
Table 2: Comparison of duration of onset of motor block between two groups
Mean duration of onset of motor blockade in Group A was 80.1 ± 11.01 seconds and in Group B it was 79.02 ± 7.98. The difference in mean duration in both groups was found to be not significant (p>0.05). It means there is a small difference in both groups. Table 3: Comparison of duration of two segment regression time between two groups
Two segment regression time showed that mean duration in Group A was 62.2 ± 7.1 seconds and in Group B it was 76.9 ± 6.19. The difference in mean duration in both groups was found to be statistically highly significant (p<0.001). It means there is more time required in Group B as compared to Group A.
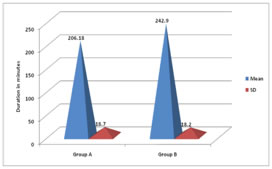
Figure 2 Figure 1: Comparison of duration of onset of sensory block between two groups; Figure 2: Comparison of post operative analgesia between two groups The above bar diagram shows that post operative analgesia in minutes in both groups. Mean duration in Group A was 206.18 ± 18.7 minutes and in Group B it was 242.9 ± 18.2 minutes. The difference in mean duration in both groups was found to be statistically highly significant (p<0.001). It means there is more time required in Group B as compared to Group A.
DISCUSSION Mean duration of onset of sensory blockade in Group A was 90.61 ± 11.99 seconds and in Group B it was 88.02 ± 9.91. The difference in mean duration in both groups was found to be not significant (p>0.05). It means there is a small difference in both groups. Mean duration of onset of motor blockade in Group A was 80.1 ± 11.01 seconds and in Group B it was 79.02 ± 7.98. The difference in mean duration in both groups was found to be not significant (p>0.05). It means there is a small difference in both groups. This is in contrast to the results obtained by Mukherjee A et al.3.In 2011 when they compared effect of different doses of nalbuphine as adjuvant to bupivacaine on sensory and motor blockade. They found that the onset time of sensory blockade following intrathecal injection of study solution containing 0.5 ml normal saline (NS) or 0.2, 0.4 and 0.8 mg Nalbuphine made up to 0.5 ml with NS added to 0.5% hyperbaric bupivacaine 12.5 mg (total volume 3 ml) to patients belonging to group A, group B, group C and group D were 1.75 ± 0.27, 1.69 ± 0.20, 1.63 ± 0.24, and 1.59 ± 0.18 minutes respectively. Similarly, onset time of motor blockade in group A, group B, group C and group D were 5.9 ± 0.57 5.8 ± 0.76, 5.7 ± 0.62 and 5.6 ± 0.53 minutes respectively. Among the groups, onset time of sensory and motor blockade were comparable and found to be statistically insignificant (P > 0.05) but when compared to our study, the early onset time in our study may be due to larger dose of inj. Nalbuphine and also use of different assessment criteria (for sensory blockade, use of L1 dermatome instead of T10 and for motor blockade, use of Bromage II instead of Bromage IV). Tiwari A.K. et al4 in 2011, did a comparative study between two different doses of Intrathecal Nalbuphine admixed with 2.5ml of Bupivacaine. They randomly allocated 75 patients to 1 of 3 groups. Group A (n = 25) received 2.5 mL of 0.5% hyperbaric bupivacaine + 1ml sterile water Intrathecally; group B (n = 25) received 2.5ml of 0.5% hyperbaric bupivacaine + 1ml (200mcg) Nalbuphine Intrathecally and group C (n = 25) received 2.5ml of 0.5% hyperbaric bupivacaine + 1 mL (400 mcg) Nalbuphine Intrathecally. It was found from the study that, two segment regression time of sensory blockade as well as duration of analgesia were maximally prolonged in group C compared to group A and group B (P < 0.05). similar results were found in our study, the two-segment regression time (in minutes) in group A (60 ± 7.02) and group B (75.66 ± 6.26) were prolonged and mentioned study. The analgesic as well as motor blocking effect of Nalbuphine appears to increase with increase in the dosage. Mostafa GM. et al5 found that 2mg of Nalbuphine when used intrathecally as an adjuvant to Bupivacaine, has produced comparatively prolonged analgesic and motor blocking effect lasting for 8.5 ± 3.67 hours and 5.9 ± 0.9 hours respectively. Mukherjee A et al3 in 2011, studied the effect of varying dose of intrathecal Nalbuphine (0.2mg vs. 0.4mg vs. 0.8mg) on duration of analgesia and motor blockade when used as an adjuvant to Bupivacaine. The duration of analgesia was progressively prolonged in groups 0.2mg, 0.4mg and 0.8mg with P < 0.05. 0.8mg recorded the longest duration of analgesia with a mean of 278.5 min compared with 237.3 min in 0.4mg. They recommend 0.4 mg as the optimal dose of Nalbuphine if used Intrathecally along with bupivacaine. The motor blockade was not altered significantly with change in the dosage of Nalbuphine. Lin ML6 compared the analgesic effect of subarachnoid administration of low dose morphine with that of Nalbuphine when administered as adjuvant with tetracaine for spinal anaesthesia and they didn’t find significant differences in duration of analgesia between the groups. Fournier et al7 compared Intrathecal morphine with Nalbuphine for postoperative pain relief after total hip replacement. They concluded that administration of Intrathecal Nalbuphine resulted in a shorter duration of analgesia than Intrathecal morphine. Culebras X et al8 compared effects of intrathecal morphine with that of Nalbuphine. They found that durations of complete and effective analgesia were significantly increased in morphine 0.2 mg (275 ± 228 min., 585 ± 446 min.) compared with Nalbuphine 0.2mg (108 ± 23 min., 136 ± 22 min.), Nalbuphine 0.8 mg (176 ± 62min., 212 ± 72min.), Nalbuphine 1.6 mg (148 ± 45min., 193 ± 77min) and further they found that increasing the Nalbuphine dose to 1.6 mg did not further improve analgesia.
CONCLUSION Intrathecal Nalbuphine (1.2mg) added to Intrathecal Bupivacaine 0.5% heavy (17.5mg) provides prolonged postoperative analgesia without increasing risk of side effects. Further studies are required to determine optimal dosage of intrathecal Nalbuphine.
REFERENCES
|
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
 Home
Home