Official Journals By StatPerson Publication
|
Table of Content - Volume 10 Issue 1 -April 2019
Ritika Deshwal1, Nidhi Kumar2*, Jagdish P Sharma3, Ranjit Kumar4
1Senior Resident, Department of Anaesthesia, Maulana Azad Medical College, New Delhi.-110011, INDIA. {2,4Associate Professor, 3Retired Professor, Department of Anaesthesia and Pain Management} {4Associate Professor, Department of Neurosurgery} Himalayan Institute of Medical Sciences, Swami Rama Himalayan University, Jolly Grant, Doiwala, Dehradun. Uttarakhand- 248016, INDIA. Email: drnidhiaries@gmail.com
Abstract Background- Patient undergoing spine surgery often suffer from moderate to severe postperative pain and may require large doses of analgesic drugs. Optimizing postoperative pain improves clinical outcomes and increases satisfaction while uncontrolled pain can considerably lead to morbidity and mortality. Aim- In this study we aimed to compare the effectiveness of dexmedetomidine as instillation at surgical site and as intravenous infusion in microdiscectomy. Setting and Design- Randomized, control trial in tertiary care hospital over a period of one year. Material and Method - 90 adult patients, undergoing elective microdiscectomy were randomised into three groups of 30 each. Group A received 100 ml normal saline (NS) infusion in 10 min and wound infiltration with 30 ml ropivacaine 0.2% before wound closure; group B received 100 ml NS infusion over 10 min and wound infiltration of dexmedetomidine 1μg/kg plus 30 ml ropivacaine 0.2% before wound closure; group C received dexmedetomidine 1 μg/kg in 100 ml NS infusion over 10 min and wound infiltration with 30 ml ropivacaine 0.2% before wound closure. The primary observations were visual analogue scores (VAS), postoperative pain scores (PPS) and postoperative fentanyl consumption for 24 hrs. Secondary end points included sedation score, recovery profile and patient satisfaction. Results: Group B showed less pain scores at 4h (p< 0.017), 8 h (p< 0.001), and 24h (p<0.001) when compared to Groups A and C. The requirement of postoperative fentanyl (µg) was 469.84±31.00, 294.17±39.22, 368.33±20.69 for groups A, B and C after 24h (p< 0.001). Group B patients were haemodynamically more stable while group C patients had higher sedation score compared with other groups. Conclusion: Subcutaneous wound instillation with dexmedetomidine and ropivacaine prolonged the pain free period and analgesic consumption, while it also enhanced patient satisfaction. Key Word: wound infiltration, microdiscectomy, dexmedetomidine, ropivacaine
INTRODUCTION Increasing number of spine surgeries are recently being performed based mainly on pain symptoms.1 As these patients often suffer from serious preoperative pain, so postoperative pain management in such patients is of great concern. Successful management of pain prevents development of chronic pain states.2 Acute postoperative pain usually starts with surgical trauma an inflammatory reaction and irritation of afferent neuronal barrage.3 Various techniques like intravenous, oral, epidural and local tissue infiltration are employed to provide effective pain management. Wound instillation of local anaesthetic at the surgical site not only has an obvious immediate action by blocking the afferent neurons but also has a longer effect due to a possible down regulation of pain receptor.4 Thus, we conducted a prospective study to evaluate the analgesic effect of dexmedetomidine by two routes; one is by iv infusion and second by wound infiltration with ropivacaine in microdiscectomy surgeries.
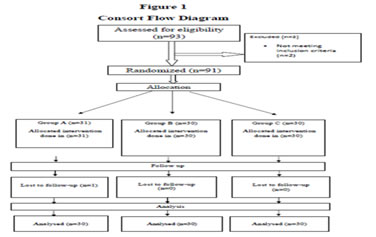
METHOD AND MATERIAL The randomized, prospective, double blinded single hospital study cleared by Ethical committee of the Institution, was conducted on patients with primary diagnosis of unilevel disc herniation without ligamental hypertrophy after obtaining written informed consent. The study included a total of ninety patients of either sex, between 18 and 60 years of age, ASA physical status I and II who underwent lumbar microdiscectomy under general anaesthesia. Patient with history of clinically relevant hepatic, renal, and/or cardio-pulmonary insufficiencies, severe cognitive impairment, history of analgesic intake were excluded from the study. After exclusion, eligible patients were assigned randomly into one of the three groups according to computer generated numbers. Group A: received 100ml NS infusion over a period of 10 minutes and surgical wound infiltration with 30 ml, 0.2% ropivacaine before wound closure. Group B: 100 ml NS infusion in 10 min and surgical wound infiltration with dexmedetomidine 1 μg/kg and 30 ml, 0.2% ropivacaine before wound closure. Group C: dexmedetomidine 1 μg/kg in 100 ml NS infusion in 10 min plus surgical wound infiltration with 30 ml, 0.2% ropivacaine before wound closure. All patients were kept fasting for 6-8 hrs and were premedicated with tablet diazepam 0.1 mg /kg and tablet ranitidine 150 mg at night. Patients were explained visual analogue scale (VAS) and the use of patient-controlled analgesia (PCA) pump for postoperative pain relief. In the operating room, standard ASA monitors were attached, and baseline vitals were recorded. The surgeon and the investigator recording the data postoperatively were completely blinded towards the patients. The randomization was not disclosed until completion of the study. The study drugs for each patient were prepared by an investigator who was not involved in data collection. Patients were induced with fentanyl (2mcg/kg) and propofol (2mg/kg). Neuromuscular blockade for tracheal intubation was achieved by vecuronium (0.1mg/kg). Ventilation was volume controlled with a tidal volume of 7-8 ml/kg. Intraoperative anesthesia and muscle relaxation were maintained with sevoflurane aiming to maintain a MAC of 1.5 and injection vecuronium. Infusion of study drugs was started at the time of wound closure. Previously prepared drugs were infiltrated by the operating surgeon under all aseptic conditions. After surgery neuromuscular blockade was reversed with glycopyrolate and neostigmine in weight adjusted doses. Postoperative pain was taken care of by giving fentanyl through PCA pump intravenously. PCA was programmed with following settings: bolus, 25µg; lockout time, 15 minutes; maximum dose, 400µg / 4 hour with no background infusion. Pain assessment in postoperative period was done by Visual Analogue Score (VAS) (0-no pain and 10 as severe or worst imaginable pain) and Postoperative Pain Score (PPS) (0 = no pain; 1 = moderate pain only when moving; 2 = moderate pain at rest, severe pain when moving and 3 = constant severe pain). After shifting the patients to recovery room their pain scores were recorded was recorded and at 30min, 1, 2, 4, 8, 12, 24hr postoperatively. The analgesic quality was assessed in two conditions: static pain till 6 hrs postoperatively when patients are confined to bed, and dynamic pain during log rolling in bed 6 h after operation. For log rolling, help of nursing staff was taken. The patient was supported from all four sides with one person supporting the neck. The patient was then turned to first right side up to 90°, then made supine and turned similarly to the left side. Care was taken at all times to avoid flexion of spine and any unsynchronised movements of the limbs. Sedation was measured by Ramsay Sedation Score (grade 1- patient appears anxious, agitated or restless, grade 2- patient is cooperative, tranquil and oriented, grade 3- patient responds to verbal command, grade 4- patient is asleep and shows response only to light, glabber tap or loud auditory stimuli, grade 5- patient is asleep and sluggish response to above and grade 6- patient is asleep and shows no response to above) (5). The primary outcome measure was the static and dynamic visual analogue score (VAS), post‑operative pain score (PPS) and the requirement of rescue analgesic over a period of 24h.and sedation score. The secondary outcomes were patient satisfaction and quality of sleep which were graded from 0 to 3 points: unsatisfactory, regular, satisfactory and excellent. Future repetition of the technique was recorded as 0 for does not know, 1 for no and 2 for yes. Perioperative adverse effects like hypotension, bradycardia, nausea and/or vomiting were noted. Hypotension (MAP value < 20% of the baseline value on two successive readings), not responding to a 200 mL fluid, was treated with ephedrine, 5mgs incremental doses. Bradycardia (heart rate <60 beats/min) was treated with glycopyrolate 0.2 mg iv bolus. Nausea and vomiting were treated with ondansetron 0.1 mg/kg, intravenous. Close monitoring of the surgical site was done in the post‑operative period to detect any excessive inflammation or infection Sample size was calculated on the basis of previous studies6. With α = 0.05 and a power of 80%, assuming 15 - 20% reduction in analgesic requirement, we needed to include 25 patients in every group. To reduce the consequences of data loss, 90 patients in total were included in the study. Computer assisted data analysis was performed with the help of commercially available software (SPSS 22, SPSS South Asia Pvt., Ltd., Bengaluru, India). One-way analysis of variance (ANOVA) was used to calculate statistical significance for analgesic requirement. Nonparametric data (pain scores, sedation scores, and patient satisfaction scores) were compared by Kruskal–Wallis ANOVA and Mann–Whitney U-test for intergroup differences. Quantitative data was expressed in terms of median (IQR). Comparisons of hemodynamic data was made using repeated measure ANOVA. Side effects were tested by chi-square test and p<0.05 was regarded as statistically significant. RESULT In all, 90 patients could complete the research protocol (Figure 1). All patients were almost similar regarding their demographic data, ASA physical status, and duration of surgery (Table 1). Patients who were given dexmedetomidine by either route had significantly lower static VAS at all interval of time and on log roll at 6 hr and 12 hr when compared with patients who received ropivacaine alone.(Table 2) The difference in dynamic VAS was highly significant between dexmetedomidine infusion and infiltration group at 8 and 24 hours (0.001%). (Table 3) Postoperative pain score was also lower in both dexmedetomidine groups as compared to patients receiving ropivacaine alone. Significant difference between group B and C was seen only at 8 hrs. (Table 4) The 24 hours fentanyl consumption was significantly lower in both dexmedetomidine groups when compared with group A. On comparing the two dexmedetomidine groups, 24 hr fentanyl consumption was lower in infiltration group (p<0.001). (Table 5) Sedation scores were higher for the first two hours after surgery in group C (median, IQR=4.00, 3.00-4.00) when compared with the group A (median, IQR=2.00, 2.00-3.00; p< 0.001) and group B (median, IQR=3.00,2.00-3.00 ; p<0.001) and was statistically significant. Time to tracheal extubation, time of following verbal commands and orientation time was significantly higher in dexmedetomidine infusion group. (Table 6) Satisfaction with the quality analgesia was excellent and satisfactory in 100% patients in group B, 60% patients in group C and 6.7% patients in group A which was statistically significant (0.001%). Readiness for repetition of technique in future was highest in group B patients (93.3%) than in group C patients (76.7%) and group A (3.3%) patients. (Table 7)
Table 1: Patients’ Criteria
Data are presented as mean ± standard deviation p< 0.05 significant ASA-American Society of Anaesthesiologists; kg - kilogram Table 2: Postoperative Static Visual Analog Scale {Median (IQR)} at different time interval
*(p<0.05) statistically significant, **(p< 0.001) statistically highly significant IQR- Interquartile range; hr- hour after completion of surgery
Table 3: Postoperative Dynamic Visual Analog Scale {Median (IQR)} among different groups at different time interval
**p<0.001 statistically highly significant
Table 4: Post operative Pain Score {Median (IQR)} of Different Groups at Different Time Interval
*p<0.05statisticallysignificant, **p < 0.001 statistically highly significant hr - hours after completion of surgery IQR-Interquartile range
Table 5: Fentanyl consumption (msg) Mean± SD and total number of PCA pushes in 24 hrs
**(p<0.001 statistically highly significant), SD- standard deviation; mcg – micrograms; PCA – patient controlled analgesia
Table 6: Recovery Profile (Mean ± SD) of Different Groups
*p<0.05 statistically significant, **p< 0.001 statistically highly significant T0 – time of completion of surgery SD- standard deviation; min - minutes Table 7: Distribution of patients according to Patient satisfaction, Sleep quality, Readiness for future repetition parameters
DISCUSSION In the present study, patients who received dexmedetomidine by either route (IV or infiltration) had improved postoperative pain scores when compared with the plain ropivacaine group. The 24 hr fentanyl consumed through PCA pumps was less in patients receiving dexmedetomidine (group B, C) compared with group A (P<0.001). The VAS scores at rest were comparable to each other in group B and C uptil 4 hours after surgery. However after 4 hours, improved VAS scores were seen in group B as compared to group C. In other studies comparing infiltration and infusion techniques, similar results were found. In a study done by Bharti N et al, it was observed that addition of clonidine to bupivacaine infiltration at surgical wound provided superior post operative pain relief and decreased morphine consumption as on intravenous administration but had less complications7. Researches show that dexmedetomidine used as an adjuvent to pre-emptive ropivacaine instillation enhances pain control and lessens the need for pain killers in the postoperative period .8 The possible mechanism of action of dexmedetomidine can be attributed to a number of reasons. Firstly, any form of surgical intervention stimulates the sympathetic nervous system to release nor-epinephrine at the wound site. This causes excitation of nociceptive receptors9. Dexmedetomidine infiltration at the wound site inhibits the prejunctional nor-epinephrine release thus blocking the pain transmission. Secondly, dexmedetomidine increase antiinflammatory cytokines and causes a decrease in proinflammatory products at the wound site. Hence, it reduces perineural inflammation as compared to sole use of local anesthetic.10 Apart from this, dexmedetomidine also accentuates local anesthetic action by selective blockage of conduction in Aδ and C fibers11.In our study, group C patients had higher sedation score at extubation (RSS- No 4,5) when compared to group A (RSS- No 2,3) and B(RSS- No 1,2) and also postoperatively which was highly significant (p<0.001). However patients did not develop respiratory depression and there vitals signs were within physiological limits. Our results were similar with the study of Ahmed M et al who found that the dexmedetomidine infusion showed more sedation in comparison to the dexmedetomidine given by infiltration.12. Time of tracheal extubation and time when patients start following verbal commands was significantly more in infusion group as compared to other two groups. Our results are in contrast to the study of Manimaram R et al. They concluded that the Group which received dexmedetomidine infusion took longer time to verbal response but there was no statistically significant difference in the two groups regarding time to extubation. This difference from our study might be because of the fact that they had given dexmedetomidine in infusion rate of 0.4 ug/kg/hr while we used a bolus dose of 1mcg/kg.13, 14 Satisfaction level regarding quality of analgesia was higher postoperatively in dexmedetomidine wound infiltration group as compared to other two groups. Patients in group B showed greater satisfaction in sleep quality assessment in the first postoperative day. Maximum patients in Group B and C were willing for repetition of the modality for analgesia in other future surgeries they might undergo. Concerns have always been raised regarding risk of postoperative wound infection after use of incisional infiltration with local anaesthetics. This concern has not been substantiated by clinical studies and it appears that local anaesthetics, may have both bacteriostatic and bactericidal actions.15 Although dexmedetomidine infusion shows biphasic effect on blood pressure that is, an initial rise in BP for 5-10 mins followed by a 10-20 % decrease in BP. However in our study, we did not observe this biphasis response which is in accordance with previous studies. This is probably due to the fact that we used a low dose of dexmedetomidine 1mcg/ kg .15 No incidence of any side effects like bradycardia, hypotension, PONV, respiratory depression, neurological deficit. No incidence of wound infection were noted in the postoperative period. The limitation of the present study was that we did a short follow up of 24 hours postoperatively. Long term follow up should be done in future researches. In conclusion, wound instillation is a simple and effective method to block transmission of pain from the surgical wound and also to reduce local inflammatory response to the injury as compared to intravenous infusion. The addition of dexmedetomidine to ropivacaine improves the quality and duration of analgesia. It is accompanied by hemodynamic stability and less side effects.
REFERENCES
|
|
 Home
Home