Official Journals By StatPerson Publication
|
Table of Content - Volume 10 Issue 2 -May 2019
A clinical comparative study between bupivacaine with clonidine and bupivacaine alone in paravertebral block for simple breast surgery
C Sankaran1, Y Sukirtharaj2*
1Assistant Professor, Department of Anaesthesiology, Government Tirunelveli Medical College, Tirunelveli, Tamil Nadu, INDIA. 2Senior Resident, Department of Anaesthesiology, Government Thoothukudi Medical College, Thoothukudi, Tamil Nadu, INDIA. Email: sukirtharaj86@gmail.com
Abstract Background: Regional anesthesia using paravertebral block, intercostalblock, and epidural anesthesia have been suggestedas an alternative technique in simple breast surgery. Regional techniques reduce postoperative pain leading to decreased requirement of analgesics thereby, indirectly leading to a reduction of postoperative nausea and vomiting( PONV). Aim:: To assess intra operative and post opeartive hemodynamic response. To assess the duration of analgesia. To study the incidence of complications of the paravertebral block. Materials And Methods: Sixty patients posted for simple breast surgery were allocated into two groups-Group BC (receiving 0.5% bupivacaine with clonidine in PVB) and Group B(receiving 0.5% bupivacaine alone in PVB).The onset of sensory block was assessed using Pinprick test. Duration of sensory block measured. Level of postoperative pain was assessed using the Visual Analogue Scale (VAS). A complication of PVB measured. Results: Patient with Group BC had a faster onset of sensory block, better intraoperative and postoperative hemodynamic response, prolonged duration of analgesiawhen compared with group B. Both groups had no complications. Three failure of PVB block in patients of both the groups was recorded. Conclusion: Patients receiving bupivacaine with clonidine and bupivacaine alone in PVB provide better surgical anesthesia and prolonged postoperative analgesia, improved postoperative recovery, reduced hospital stay when compared with general anesthesia. Key Word: Paravertebral, Breastsurgery, Sensory block, Bupivacaine, Clonidine
INTRODUCTION A large number of patients hospitalized annually for surgical management of breast malignancy or breast disease entail heavy costs. Recent efforts are focused on containing hospital costs and reducing the length of hospital stay. 1General anesthesia (GA) is mostly used in the surgical treatment of benign breast disease and malignancies. The side-effects and complications of general anesthesia such as postoperative pain, nausea, vomiting, increase morbidity. This complication prolongs recovery room stays and necessitates hospitalization for patients.2 Most importantly, nausea and vomiting have been described by patients as most deliberating than the operative procedure itself. In addition, general anesthesia alone does not produce adequate postoperative pain relief.3 Parenteral narcotic use is routine after emergence from anesthesia and during the early postoperative interval, which further increases the incidence of nausea, vomiting, sedation and results in the prolonged recovery room and stay.4 Regional anesthesia using a thoracic paravertebral block (TPVB) is an ideal alternative to general anesthesia for benign breast disease and malignancies. Benefits include a reduction in the intraoperative and postoperative analgesic requirement, prolonged postoperative pain relief, thus improving postoperative recovery and indirectly leading to reduced postoperative nausea, vomiting and potential for early discharge.5 The thoracic paravertebral block involves the injection of local anesthetic at the site of emergence of the spinal nerve, from intervertebral foraminae. The paravertebral space contains dorsal and ventral rami and the sympathetic chain. Hence, infiltration of this space results in unilateral sensory, motor and sympathetic blockade.6 Paravertebral block has been used to relieve acute chest wall pain from rib fractures, herpes zoster, pleurisy, to manage acute and chronic post-thoracotomy pain, and as an anesthetic technique for surgery of the chest, breast, and cholecystectomy.7Paravertebral blocks are relatively easy to learn and perform, have low side effect and no additional nursing surveillance. This leads to early discharge and reduces hospital stay. Immediate post operative analgesia is achieved by pre-incisional PVB in patients who had undergone breast malignancy surgery. Paravertebral nerve blocks achieve excellent pain relief and inhibit the neuroendocrine stress response to surgical manipulation.8 MATERIALS AND METHODS Sixty patients posted for simple breast surgery were allocated into two groups-Group BC (receiving 0.5% bupivacaine with clonidine in PVB) and Group B(receiving 0.5% bupivacaine alone in PVB).The onset of sensory block was assessed using Pinprick test. Duration of sensory block measured. Level of postoperative pain was assessed using the Visual Analogue Scale (VAS). A complication of PVB measured. Procedure: All the Patients were instructed to be in sitting position. The part was cleaned and painted with an antiseptic solution. Sterile drapes were placed. Planned needle insertion point was infiltrated with a local anesthetic in such way analgesia extended from T1 To T6. Tuohy‟s epidural needle perpendicularly inserted from the skin to hinge transverse process at 3-5 cm depth. A syringe with prefilled air was connected to the Tuohy‟s epidural needle. From the transverse process, the needle is superiorly walked off, and advanced 0.5 to 1cm.On introduction loss of resistance to air could be elicited. The syringe was detached from the needle and drug injected. In single-level technique, the total volume of drug 21 ml was injected or in multiple level block, 3-4 ml of drug/dermatome was injected. At the time of injection, negative aspiration was done to prevent intravascular injection. The maximum dosage used was 3 mg/kg of body weight. The patient was then made to lie down supine. The onset of sensory anesthesia occurred 10 -15 minutes after the injection. Group BC was injected with 21 ml of 0.5% bupivacaine with clonidine (2 mics/kg).Group B was injected with 21 ml of 0.5% bupivacaine with 1ml of normal saline. After the block patient was sedated with intravenous opioids. Oxygenation with a facemask (4lit/min).In case of any block failure, patient excluded from the study. The onset of Sensory block, HR, MAP, and SpO2 were recorded 5, 10,15,20, 30, 45,60, and 90minutes after the block and 1, 2, 4, 8, 12and 24hours after the end of surgery. Sensory block for each dermatome was assessed by a pinprick test using a 3- point scale:
The onset of sensory block time was defined as the time period between the end of the local anesthetic administration to loss of touch sensation (score 2 in each dermatome.) Duration of sensory block is defined as the time period between the ends of local anesthetic injection to complete recovery of anesthesia on each dermatome. Duration of analgesia was calculated from the end of local anesthetic injection to the first complaint of pain. Visual Analog Scale (0 –10) was used for postoperative pain assessment Inj. diclofenac 75 mg i.m. was given when the Visual Analog Scale >4. Statistical Analysis: The observations recorded in each group were compared using statistical analysis. The raw data collected using the protocol was converted into grouped data. After the collection of data, the mean and standard deviation was calculated for each variable in both the groups.If the two means in two groups were found to be separated by more than twice of standard error(>2SE) then the two means were considered as highly significant (p<0.05).If the two means were found to be separated by more than thrice of standard error(>3SE),then the two means were considered as very highly significant(p<0.001).ANOVA, Student‟s paired t-test was used when data were normally distributed. The software used for the calculation of p-value was Stata (Version 10).
OBSERVATION AND RESULTS The study was conducted at Tirunelveli Medical College Hospital. After obtaining approval from the Hospital Ethical Committee, sixty patients were randomized into two groups. Group BC consisted of patients receiving bupivacaine with clonidine in PVB while Group B consisted of patients receiving bupivacaine only. There was a total failure of the block in 3 cases of which 2 in Group B and 1 in Group BC. They were excluded from the study. In both, the group's complications were not observed. Age, the weight of the patient and duration of surgery between both the groups were comparable and were not statistically significant (P>0.05) Table 1: Comparison of age (yrs), wt(kg) distribution between the two groups
Table: 1 The mean age(yrs) and weight in kg of BC group was 32.9and55.33 and the B group was 32.33and55.87,the difference between two groups statistically not significant (p>0.05).
Table 2: Comparison of baseline pr, map, spo2 between the two groups
Table: 2 shows The preoperative baseline PR, MAP, SPO2 among the two groups comparison were statistically not significant (p>0.05).
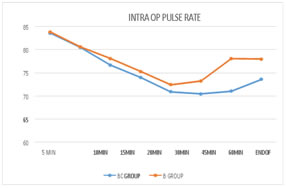
Graph 1: Comparison of intraoperative Pulse Rate between two groups at various intervals Graph: 1 The mean intraoperative PR was lower in group BC, Except 5th and 10thminute,when compared to group B. This was statistically significant (p<0.05) Table 3: comparison of onset of sensory block between two groups
Table 3: shows The mean onset of sensory block was 8.937 minutes in group BC and 11.32 minutes in group B. When compared it was statistically high significant(p<0.05).
Table 4: Comparison of Total Duration of Sensory Block Between Two Groups
Table: 4 shows The mean total duration of sensory block was HIGH in group BC when compared with group B. It's statistically highly significant(p<0.01). Table 5: comparison of duration of analgesia between twogroups
Table: 5 shows The mean duration of analgesia was 1098 minutes in group BC, and 713 minutes in group B when compared, It was statistically highly significant(p<0.05).
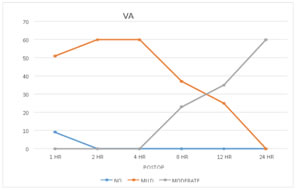
Graph 2: Comparison of visual analog score for pain between two groups a various intervals The mean of the visual analog score was 1hr,2hr,4hr,8hr,12hr,24hr was low in group BC when compared with group B. Its statistically significant (p<0.05), except 1hr VAS, is not statistically significant. DISCUSSION In our study we observed, demographic data like age (yrs), sex, weight in(kg), ASA grade are not statistically significant when compared in both groups. Diagnosis, a procedure such as a lumpectomy, excision, wepster procedure, simple mastectomy, and duration of surgery are not statistically significant when compared both the groups. Addition of clonidine with bupivacaine in the thoracic paravertebral block provided effective surgical anesthesia and reduced the onset of sensory blockade time.It prolonged the total duration of sensory blockade time and also prolonged total duration of analgesia when compared to the control group.10 Patients had the low postoperative visual analog score inHR,4HR,8HR.12HR,24HR. Patients were hemodynamically stable in both intraoperative and postoperative period and there was no bradycardia. The α 2 agonists dose-dependently, enhance the potency and prolong the duration of local anesthetic by combining with α 2 receptors at the peripheral level. The other action includesVasoconstriction around the site of injection. Thus the absorption of the local anesthetic drug will be delayed, resulting in a prolongation of the local anesthetic effect.Clonidine directly inhibits the peripheral nerve action. Release of local enkephalin like substances.A decrease in the release of local inflammatory mediators. Increase in the release of anti-inflammatory cytokines.Clonidine and Dexmedetomidine are the currently used α 2 receptor agonists.11 In my study mean duration of analgesia is prolonged >18.3 HRS in group BC, which is closely related to,Millan MJ.et.al Fifteen patients with breast malignancies, who underwent surgical management under PVB, in the form of MRM with axillary dissection were studied retrospectively. The onset of sensory blockade was prolonged upto 23 hrs effectively relieving postoperative pain.12 In a study conducted by Olson Jet .al, in patients posted for simple mastectomy, PVB with bupivacaine was used. Duration of analgesia was 17hrs and all patients observed no pain for the first 8hrs after surgery, which was comparable to my study. 13 Ready LBet al, the studyobserved that PVB with fentanyl and clonidine in combination with levobupivacaine (0.05%) are effectiveanalgesics, a significantly reduced the supplemental postoperative morphine consumption after breast surgery.14 Richardson J. et al retrospective study of 145 cases, who underwent surgical treatment for breast malignancies using paravertebral block and 100 cases receiving general anesthesia alone. TPVB alone was enough for completing the surgery in 85% of patients, while 5.7% of patients required supplementation with a local anesthetic.15 In a study conducted by Schaible HGet al, twenty-five patients underwent breast surgery with paravertebral block and sedation as an alternative to general anesthesia. Postoperatively, patients had minimal nausea, vomiting, and pain. The procedure was satisfactory for all patients.16 In a study conducted by Stein Cet al, TPVB with 0.5% bupivacaine at the level T3,prior to general anesthesia in patients posted for breast cancer surgery(MRM).only three patients had pain on the first postoperative day in comparison to the control group which had twelve patients with postoperative pain(p=0.007).In the 24 hours postoperative follow-up, VAS scores were higher in the control group in comparison to the group receiving PVB block.17 Tasmuth Tet al, in their study of sixty patients, found that patients receiving PVB experienced statistically significantly less pain at 30 min, 1 hr, 24 hr and 72 hr in comparison to patients receiving GA only. In our study, no complication occurred in both groups, except for 3 patients with failure of the blockade, similar to the study conducted by Moller and Greengrass. Various studies on paravertebral blocks have quoted different rates ofcomplications18
CONCLUSION Paravertebral block, when used in alone, provides effective surgical anesthesia and superior analgesia in the post operative period. Paravertebral block reduces the incidence of postoperative nausea andvomiting. Paravertebral block provided effective intra operative and postoperative hemodynamicstability. Paravertebral block leads to a reduced hospital stay and earlydischarge. Complication rates of the paravertebral block are significantly low thereby proving it to be a relatively safe procedure.
REFERENCES
|
|
 Home
Home