Official Journals By StatPerson Publication
|
Table of Content - Volume 10 Issue 2 -May 2019
Efficacy of supraclavicular brachial plexus block by using USG guided method versus peripheral nerve stimulator guided method: A comparative study
Raviraj Shivajirao Pol1, Abhimanyu Tarkase2*
1Junior Resident III, 2Associate Professor, Department of Anesthesiology, S.R.T.R. Medical College, Ambajogai, Beed, Maharashtra. Email: raviraj2320@gmail.com
Abstract Background: Regional blocks offer several advantages over general anaesthesia. Supraclavicular approach to brachial plexus block is the preferred regional anaesthesia for upper limb surgeries they achieve ideal operating conditions by producing complete muscular relaxation, maintaining stable intraoperative hemodynamic, and the associated sympathetic block. The sympathetic block decreases postoperative pain, vasospasm and edema. Aim and objectives: To study the efficacy of supraclavicular brachial plexus block by using USG guided method versus peripheral nerve stimulator guided method. Materials and Method: The present study conducted on 100 patients admitted for elective upper limb surgeries belonging to American Society of Anaesthesiologists (ASA) Grade I and II of either sex from 18 to 50 years of age. The selected patients were allotted in two groups by using randomization technique. Group USG (Ultrasound guided): received USG supraclavicular brachial plexus block using inj.bupivacaine 0.25% and Group PNS (Peripheral nerve stimulator): received supraclavicular brachial plexus block using PNS and using inj.bupivacaine 0.25%. All the patients underwent thorough pre-anaesthesia evaluation on the day prior to the surgery. The time taken for the procedure, the onset of sensory blockade and motor blockade were noted. Intra-operatively, hemodynamics were monitored at regular intervals. Following completion of surgery, the patients were monitored to assess the quality and duration of post-operative analgesia. At the time of each subsequent assessment, patients were observed and/ or questioned about any subjective and/or objective side effects (sedation, nausea, vomiting or respiratory depression, neurological injury). Results: The mean time taken for the procedure to administer the block by using an ultrasound was 14.08 ± 5.09 minutes, whereas by using Peripheral nerve stimulation was 9.76 ±3.45 minutes and the difference observed was statistically significant. The mean time of onset of sensory block and motor block in both the groups was not statistically significant. Similarly difference in mean duration of sensory block and duration of motor block in both the group was not significant. The block was successful in 84% of patients in group USG as compared to 74% in group PNS. But the difference observed was not statistically significant (P>0.05). Intra-operative complication like vessel puncture were more in PNS group (14%) than USG group (4%). Conclusion: Thus we conclude that the success rate and effective quality of the block were more with ultrasound group than peripheral nerve stimulator group. But time taken for the block performed by ultrasound was longer than the peripheral nerve stimulator technique which means expertise is required to administer and use ultrasound machine. The incidence of complications like vessel puncture was seen more in peripheral nerve stimulator technique as compared to ultrasound group. Key words: supraclavicular brachial plexus block, USG guided, PNS guided.
Peripheral nerve blockade is now a well-accepted component of comprehensive anaesthetics care with analgesic care. Its role has expanded from the operating rooms into area of postoperative and chronic pain management to surgical and medicine intensive care units. Skillfull application of peripheral neural blockade broadens the anaesthesiologist’s range of options in providing optimal anaesthetic care. By providing surgical anaesthesia and postoperative analgesia to the entire upper limb, it has been intimately linked with advances in ambulatory surgery. Ambulatory surgery is becoming increasingly desirable because it offers massive economic advantage, much comfortable and convenient for the patient and also for the surgeon. It plays a major role in day care surgeries where top priorities of success are: alertness, ambulation, analgesia and alimentation. A peripheral nerve block is safer in high risk patients with cardiopulmonary diseases, diabetes or other chronic illness as it minimally disturbs the coronary hemodynamic and also blunts the stress response to surgery, also minimal changes in hemodynamic of the patient. Regional blocks offer several advantages over general anaesthesia. It avoids polypharmacy and reduces complications and side effects of general anaesthesia like post anaesthetic nausea and vomiting, atelectasis, hypotension, ileus, dehydration and deep vein thrombosis. It avoids stress of laryngoscopy and tracheal intubation. In addition it provides the advantages of early ambulation. Supraclavicular approach to brachial plexus block is the preferred regional anaesthesia for upper limb surgeries1 they achieve ideal operating conditions by producing complete muscular relaxation, maintaining stable intraoperative hemodynamic, and the associated sympathetic block. The sympathetic block decreases postoperative pain, vasospasm and edema. Brachial plexus blockade is a time tested technique for upper limb surgeries. Among the various approaches of brachial plexus block, supraclavicular approach is considered easiest and most effective approach. The first ever supraclavicular brachial plexus block was performed by Kulenkampff in 19112. The classical approach using paresthesia technique is a blind technique and may be associated with higher failure rate and injury to surrounding vessels, nerves and other structures like lung pleura3. To avoid some of these problems use of peripheral nerve stimulator was started which allowed better localisation of the nerve and plexus4,5. However this technique of nerve stimulator may not be fool proof with persistent risk of injury to surrounding structures, nerves6, and pleura leading to pneumothorax7. The application of Ultrasound technique for exact localisation of nerves/plexus has revolutionised the regional anaesthesia field where in ultrasound probes with suitable frequencies have been successfully tried. Ultrasound use for supraclavicular brachial plexus block has improved the success rate of block with excellent localisation of neuronal structures as well as improved safety of margin8. Hence the study was planned for comparing the efficacy of ultrasound guided technique with peripheral nerve stimulator guided technique for supraclavicular brachial plexus block. MATERIALS AND METHOD The present study was conducted in SRTR Govt. medical college, Ambajogai, Beed; tertiary care hospital after obtaining approval from institutional ethical committee and written informed consent was obtained from each patient. The study was conducted on 100 patients admitted for elective upper limb surgeries belonging to American Society of Anaesthesiologists (ASA) Grade I and II of either sex from 18 to 50 years of age. The selected patients were allotted in two groups by using randomization technique.
A sample size of 50 patients per group was calculated based on a review of literature to show a significant difference between groups, assuming 85% successful blocks in Group USG and 78% successful blocks in Group PNS, keeping a probability of Type 1 error of 0.05 and a probability of Type 2 error of 0.2 as acceptable by Kelsey formula. All the patients underwent thorough pre-anaesthesia evaluation on the day prior to the surgery. All systems were examined including airway and the surface anatomy where the block was going to be given and the procedure to be carried out was explained. They were informed about development of paresthesia. Patients were reassured to alleviate their anxieties. All the patients were kept nil per oral as per the fasting guidelines. All of them received Tab. Diazepam 10mg and Tab. Ranitidine 150mg night before the surgery. Written informed consent taken. Standard procedure protocol was followed for both the groups. The time taken for the procedure, the onset of sensory blockade and motor blockade were noted. Intra-operatively, hemodynamics were monitored at regular intervals. Following completion of surgery, the patients were monitored to assess the quality and duration of post-operative analgesia. Thus the patients were asked to classify analgesia as no pain, mild pain, moderate pain or severe pain every hour for the first 6 hours and then again at 8 and 10 hours and 12 hours up to 24 hours. At the time of each subsequent assessment, patients were observed and/ or questioned about any subjective and/or objective side effects (sedation, nausea, vomiting or respiratory depression, neurological injury). RESULTS Table 1: Demographic data of the two groups
In the present study the average age was 33.04 ± 8.05 years in group USG and 33.64 ± 8.74 years in group PNS, with p value of 0.7 (P>0.05) which is statistically not significant. Youngest patient in the study was 18 years and oldest was 48 years. The average weight of the patients were 63.94 ± 8.46 kgs in group USG and 62.5 ± 7.08 kgs in group PNS respectively. As the p value is 0.35 so there was no significant difference in the weight between the two groups. In group USG there were 27 males and 23 females whereas in USG group there were 26 males and 24 females, Both groups had male patients slightly more than (P>0.05).
Table 2: Distribution according parameters of block in each group
The mean time taken for the procedure to administer the block by using an ultrasound was 14.08 ± 5.09 minutes, whereas by using Peripheral nerve stimulation was 9.76 ±3.45 minutes and the difference observed was statistically significant. The mean time of onset of sensory blockade in group USG was 10.2±3.25 minute and in group PNS it was 10.4±2.58 minute. The slightly delayed onset of sensory blockade in group PNS was however not statistically significant as the P value is 0.7343 (P>0.05). The onset of motor block was within 14.42±3.33 minute in group USG and 14.28±2.97 minute in PNS group and the difference was not statistically significant (P>0.05). In group USG the mean duration of sensory blockade was 499.2±74.17 minute and in group PNS it was 484.8±121.12 minutes. The duration of sensory blockade was shorter in group PNS when compared to group USG, however it was not statistically significant (P>0.05). In group USG the mean duration of motor blockade was 462.2±76.49 minute, whereas in group PNS it was 449.6±120.44 minute. The duration of motor blockade was slightly shorter in group PNS when compared to group USG but it was not statistically significant (P>0.05). Table 3: Distribution according to overall effectiveness of the blocks in both the groups
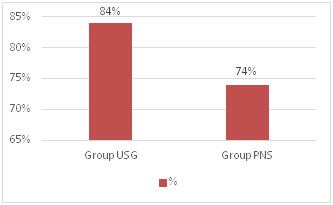
X2=0.219, df=1, p=0.326072 (not significant) It was seen that the block was successful in 84% of patients in group USG as compared to 74% in group PNS. But the difference observed was not statistically significant (P>0.05).
Figure 1: Overall effectiveness of the blocks in both the groups Table 4: Distribution according to complications occurred
X2=3.05, df=1, p=0.080 (not significant) Intra-operative and post-operative Minor complications like Nausea and vomiting, Hypertension and Hypotension, Horner’s syndrome, Recurrent laryngeal nerve palsy, phrenic nerve palsy Diaphragmatic palsy were nil in both the groups. While performing supraclavicular brachial plexus block, Intra-operative complication like vessel puncture were more in PNS group (14%) than USG group (4%). There were no cases of pneumothorax or nerve injury in our study groups.
DISCUSSION The present prospective comparative study was conducted in the Department of Anaesthesiology S.R.T.R. Medical college and Hospital at Ambajogai, Beed, on 100 patients aged between 18-50 years posted for upper limb surgeries compared with the Ultrasound guided and PNS guided supraclavicular brachial plexus block in terms of Time taken to give the block, Onset and duration of sensory and motor blockade, success rate and Incidence of complications. In the present study the mean age group was 33.04±8.05yrs in USG group and 33.64±8.74yrs in PNS group. While mean weight in both groups was 63.94±8.46yrs in USG group while 60.72±7.08yrs in PNS group. Stephan R Williams et al9 who studied Ultrasound guidance to speed execution and improve quality of supraclavicular brachial plexus block, there were no significant differences in the demographic characteristics of the two study groups. In Group US versus Group NS, respectively, mean age was 49±16yrs versus 47±15yrs, mean weight was 78±16kg versus 73±12kg. In their studies Dr.Dilip Kothari10 selected 250 patients of both sexes between the ages of 18-50 years who were posted for upper limb surgeries were administered brachial plexus block with a new technique of lateral approach with 20 degree tilt. Thus there were no clinical or statistical significant differences in the demographic profile of patients in either group. Time taken to give the block is defined as the interval between preparation of the parts to the administration of total dose of local anaesthetic agent. The mean time to perform the block with the help of ultrasound technique (14.08±5.09min) was significantly longer when compared to Peripheral nerve stimulator guided group (9.76 ± 3.45min). The longer time for the block performance found in group USG can be explained as the less experience and skills in using the ultrasound. The study done by Morros C, Perez- Cuenca MD et al11 suggest that the use of ultrasound in regional anaesthesia requires the acquisition of new knowledge and skills not only by anaesthesiologist in training but also by anaesthesiologist experienced in nerve stimulation guided peripheral nerve blocks, showing at least 15 ultrasound-guided axillary blocks are required before good results can be expected with the new procedure. Stephen R Williams et al9 found that the amount of practice necessary to master Supraclavicular brachial plexus blockade remains an open question. The average time necessary to perform the block in their study was significantly shorter in Group US than in Group NS (5.0 ± 2.4 min versus 9.8 ± 7.5 min, respectively, it was due to hands on practice or blocks performed by anaesthesiologists master in Ultrasound techniques. One of the studies examining the number of brachial plexus blocks needed to attain a reasonable degree of proficiency with the technique estimated that at least 62 blocks should be performed to achieve a success rate of 87%. This number of blocks may not allow most residents to complete their nerve block learning curve before entering practice. Ultrasound guidance, by specifying for each patient the location of the target nerves, their relation to neighbouring structures, and the path of needle by which local anaesthetic will be injected, could allow trainees to become more safe and successful in nerve blockade within the limited exposure provided by a typical residency programme. The onsets of sensory blockade in our study in all major nerve distributions were almost similar in both PNS group and USG group. Onset time of sensory block with the use of Peripheral nerve stimulator in our study was 10.4 ± 2.58 min and 10.2 ± 3.25 min with the use of Ultrasound method. The times for sensory and motor blocks in the distribution of radial, ulnar, axillary and musculocutaneous nerves were assessed every 5 min until 15 min and then at 30 min and every 30 min after, from the end of local anaesthetic (LA) injection and found that block onset times and success rate were similar whether Nerve stimulator or Ultrasound was used. In contrast Marhofer P, Schrogendorfer K,et al12, who found that onset time was significantly shorter in USG group compared to PNS group and quality of the block was significantly better in ultrasound group than nerve stimulator group in many cases we studied. Duration of sensory blockade after giving supraclavicular brachial plexus block in our study were, in USG group it was 499.2±74.17 minutes and in PNS group it was 484.8 ± 121.12 minutes, so there was almost similar post-operative analgesia duration in both the groups. In the present study, the onset of motor blockade occurred within 14.42 ±3.33 min in USG group, while 14.28 ± 2.97 min in PNS group which was almost similar. Stephan R Williams et al9 found that the onset of motor blockade paralleled that of sensory blockade. EgonLanz, Dieter theiss, et al13 compared the extent of blockade by interscalene and supraclavicular brachial plexus block using 50ml of 0.5% bupivacaine and they found that motor blockade developed faster than the sensory blockade. They explained this to arrangement of motor fibres in the mantel and sensory fibres in the core of the trunks and cords. Stephen Kapral et al14 studied ultrasound guided Supraclavicular brachial plexus block. Patients were randomly assigned to Group A (axillary approach) and Group S (lateral paravascular approach) and they found that there was no significant difference in the extent of motor or sensory block. Onset of plexus block was similar in both groups between 10 and 20 min, with complete analgesia occurring in 40 min. In our study, the duration of sensory blockade was more in ultrasound group than the conventional group which was not statistically significant. The duration of motor blockade was almost equal in both groups. In contrast Kapral S et al15 compared ultrasound and nerve stimulator guided supraclavicular brachial plexus block in 160 patients and found that sensory, motor, and extent of blockade was significantly better in the ultrasound group when compared with the nerve stimulator group. In the present study it was observed that out of 50 patients in USG group 42 blocks were completely successful (84%); 8 blocks were failed and needed supplementation in the form of general anaesthesia (16%). Out of 50 patients in PNS group, 37 blocks were completely successful (74%); 13 blocks were failed and needed supplementation in the form of general anaesthesia (26%). Lack of expertise in Ultrasound might be one of the reasons for those 16% failed blocks. In a study conducted by Stephan R Williams et al9 found that out of 80 patients which were divided in to two groups of US(ultrasound) and NS (nerve stimulator) Surgical anaesthesia without supplementation was achieved in 85% of patients in group US and 78% of patients in group NS (p=0.28). No patient in group US and 8% of patients group NS required general anaesthesia (p=0.12). Geiser T, Lang D, Neuburger M, et al16 in their study on 56 patients ‘Perivascular brachial plexus block, Ultrasound versus nerve stimulator’ found that at the beginning of surgery complete nerve blockade was achieved in 89% in the US(ultrasound) group and 68% in the NSt(electrical nerve stimulation group) (p=0.006), 3 (US) versus 7 (NSt) patients needed supplementation and 3 (US) versus 11 (NSt) patients needed general anaesthesia (p=0.022). Stephan R Williams, Philippe Chouinard,et al9 compared ultrasound and nerve stimulator for the supraclavicular brachial plexus block. They have reported that in group USG 85% of blocks could be successfully achieved (surgical anaesthesia) without supplementation, compared with 78% in nerve stimulator group. General anaesthesia was required in 0% and 8% of USG and nerve stimulator patients respectively. Complications during supraclavicular brachial plexus block can be intraoperative or postoperative which includes major complications like Pneumothorax, vessel injury and hematoma, nerve injury and minor complications like transient recurrent laryngeal nerve injury, hemi- diaphragmatic paresis, nausea and vomiting, Horner’s syndrome. In our present study we found that vessel puncture formation occurred in the PNS group 14%; whereas in ultrasound group it as 4%, because ultrasound provides direct visualisation of vessel around the plexus and also needle path, this complication was less in USG group. We can also take the help of Doppler to visualise the vessels. We did not found any other major complications like nerve injury or pneumothorax in both of the groups. Yuan Jia-min et al17 studied complications of Ultrasound and Peripheral nerve stimulator guidance for upper extremity peripheral nerve blocks (brachial plexus) and he found that ultrasound decreases risk of complete hemi-diaphragmatic paresis or vascular puncture and improves success rate of brachial plexus nerve block compared with technique that utilizes PNS for nerve localization. Larger studies are needed to determine whether or not the Ultrasound can decrease risk of neurological complications. Fear of pneumothorax limits the use of supraclavicular technique. The incidence of pneumothorax with the classic supraclavicular technique ranges from 0.5% to 6%. Many authors have studied the anatomy of brachial plexus and analyzed methods to prevent pneumothorax. These include use of several modifications of Supraclavicular brachial plexus block such as modified lateral technique or plumb bob approach. Ultrasound gives a real-time visualisation of structures including not only the blood vessel, bone, nerve, but also pleura. No patient in our study showed any clinical evidence of pneumothorax in both the groups. Dilip Kothari10 administered Supraclavicular brachial plexus block in 250 patients of age 18yrs to 50yrs undergoing upper limb surgeries by eliciting paresthesia, he found that 6% cases had vessel puncture during the procedure but block could be performed successfully in these patients once the pressure stopped the bleeding, No serious complications like pleural puncture, pneumothorax or any other cardio-respiratory side effects were observed during the procedure. In a study conducted by Perlas A et al18 Five hundred ten ultrasound-guided supraclavicular blocks were performed (50 inpatients, 460 outpatients) by 47 different operators at different levels of training over a 24- month period. Successful surgical anaesthesia was achieved in 94.6% of patients after a single attempt; 2.8% required local anaesthetic supplementation of a single peripheral nerve territory; and 2.6% received an unplanned general anaesthetic. No cases of clinically symptomatic pneumothorax developed. Complications included symptomatic hemi-diaphragmatic paresis (1%), Horner syndrome (1%), unintended vascular punctures (0.4%), and transient sensory deficits (0.4%).
CONCLUSION Thus we conclude that the success rate and effective quality of the block were more with ultrasound group than peripheral nerve stimulator group. But time taken for the block performed by ultrasound was longer than the peripheral nerve stimulator technique which means expertise is required to administer and use ultrasound machine. The incidence of complications like vessel puncture was seen more in peripheral nerve stimulator technique as compared to ultrasound group.
REFERENCES
|
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
 Home
Home