Official Journals By StatPerson Publication
|
Table of Content - Volume 10 Issue 2 -May 2019
Comparative study on efficacy of caudal bupivacaine and ropivacaine in providing postoperative pain relief in children
C Sankaran1, Aldona Shaji2*
1Assistant Professor, Department of Anaesthesiology, Government Tirunelveli Medical College, Tirunelveli, INDIA. 2Senior Resident, Department of Anaesthesiology, MOSC Medical College, Kolenchery, Kerala, INDIA. Email: aldona.shaji@gmail.com
Abstract Background: Pain is an unpleasant subjective sensation which can only be experienced and not expressed, especially in children. Pain relief is even more important in children who rely on their parents or caregivers for their well-being. The concept of postoperative pain relief and its use in the pediatric age group has improved dramatically over recent years. Aim of the study: The objectives of the study were to compare the efficacy of caudal Bupivacaine and Ropivacaine to provide post-operative pain relief in children and also to compare the motor block and hemodynamic effects caused by them in the pediatric population. Methods: In a randomized, prospective, parallel group, double-blinded study, 50 children were recruited and allocated into two groups: Group B (n=25) received 0.25% Bupivacaine 1ml/kg and Group R (n=25) received 0.2% Ropivacaine 1ml/kg. Induction of anesthesia was achieved with 50% N20 and 8% Sevoflurane in oxygen in spontaneous ventilation. An appropriate sized LMA was then inserted and a caudal block performed in all patients. Peri-operative hemodynamic parameters were monitored. The pain was assessed with Face, Legs, Activity, Cry and Consolability (FLACC) pain score and degree of motor blockade was assessed with Bromage scale. Results: Group B patients achieved a statistically significant higher Bromage score compared with Group R patients (p<0.001). The quality and duration of analgesia were comparable between both the groups. The peri-operative hemodynamics were stable and comparable between both the groups. Conclusion: Caudal Ropivacaine 0.2% (1ml/kg) provides effective postoperative analgesia similar to caudal Bupivacaine 0.25%(1ml/kg) and less motor blockade as compared to Bupivacaine, making it a suitable agent for day care surgery with an increased safety margin in younger children. Keywords: Analgesia, anesthesia, caudal, Ropivacaine, Bupivacaine, motor blockade, post-operative period.
INTRODUCTION The various pain relief methods have some side effects which prohibit their use in children for e.g., narcotics, because of their respiratory depression, the other analgesics which can’t be given for general anesthesia due to the chance for vomiting and aspiration, the objection to the needles in the case of parentally administered analgesics.1 The regional anesthetic technique significantly decreases the postoperative pain and the requirement for systemic analgesics. The caudal route was chosen for this study because it is one of the safest and simplest techniques that can be used in the pediatric age group and have a high success rate.2 The epidural space in children favors the rapid longitudinal spread of drugs thus giving good postoperative pain relief. Usually, the caudal block is placed after the induction of general anesthesia and so is used as an adjunct to intraoperative anesthesia along with postoperative analgesia in children undergoing surgical procedures below the level of the umbilicus.3 Caudal analgesia can decrease the amount of inhaled and IV anesthetic administration, attenuates the surgical stress response, facilitates a rapid, smooth recovery, and provides good postoperative analgesia.4 Unfortunately, the motor block produced by caudal anesthesia may be a cause of distress to children in the postoperative period.5 Bupivacaine has proved its efficacy in providing long-lasting analgesia when administered caudally. Ropivacaine is a long-acting amide local anesthetic-related structurally to bupivacaine. It provides a similar type of pain relief with less motor blockade. Literature suggests that ropivacaine is less cardiotoxic than bupivacaine.6 METHODS In a randomized, prospective, parallel group, double-blinded study, 50 children were recruited and allocated into two groups: Group B (n=25) received 0.25% Bupivacaine 1ml/kg and Group R (n=25) received 0.2% Ropivacaine 1ml/kg. Induction of anesthesia was achieved with 50% N20 and 8% Sevoflurane in oxygen in spontaneous ventilation. An appropriate sized LMA was then inserted and a caudal block performed in all patients. Peri-operative hemodynamic parameters were monitored. The pain was assessed with Face, Legs, Activity, Cry and Consolability (FLACC) pain score and degree of motor blockade was assessed with Bromage scale. Exclusion criteria: 1. Suspected coagulopathy 2. Infection at the site of caudal block 3. History of developmental delay 4. Neurological diseases 5. Skeletal deformities 6. Allergy to local anesthetics Preoperative evaluation: In all children, age, I.P. No., body weight, and baseline vital parameters were recorded. History regarding previous anesthesia, surgery, any significant medical illness, medications, and allergy was recorded. Complete physical examination and airway assessment were done. Following laboratory investigations were done: hemoglobin %, blood sugar, urea, serum creatinine, and urine analysis. Study Method: After getting institutional ethical committee approval and written informed consent from parents, the patients were randomly allocated into two groups. Group B (n = 25) was taken as Bupivacaine group and Group R (n=25) as Ropivacaine group. All the patients were premedicated with Inj.Atropine 0.02mg/kg i.m. 45 min prior to anesthesia. Induction of anesthesia was achieved with 50% N20 and 8% sevoflurane in oxygen in spontaneous ventilation. Appropriate size LMA was inserted. After the insertion of LMA, Sevoflurane concentration was reduced to 3% in 50% nitrous oxide, patients were left in spontaneous ventilation and a caudal block was performed in all patients according to the group. The inhaled concentration of sevoflurane was adjusted to achieve hemodynamic changes < 30% of the baseline values. No other narcotics, analgesics or sedatives were used intraoperatively. Standard monitoring was used during anesthesia and surgery. HR, MAP, and SpO2 were recorded before surgery and every 5min till the end of surgery. The occurrence of intraoperative hypotension requiring a fluid bolus, bradycardia requiring atropine and the maximum maintenance concentration of sevoflurane(%) were recorded. Using the pediatric observational FLACC pain scale with its 0 – 10 score range, each patient’s pain intensity was assessed. If the FLACC pain scale was 4 or more, syrup paracetamol 15mg/kg was administered. The duration of analgesia (from the time of caudal injection to the time at which FLACC score 4 or more) was also recorded. Motor blockade was assessed using Bromage score(Grade 1 to 4). The patient is considered a reversal of motor blockade if the score is grade 1. The following times were recorded: The anesthesia time (time from induction of anesthesia to the end of surgery when sevoflurane discontinued)1. Time from caudal block to skin incision.2. Time from caudal block to end of surgery. Complications such as PONV, respiratory depression, hypotension, and bradycardia were also noted. Respiratory depression was defined as a decrease in SpO2 of less than 95%% requiring supplementary oxygen. Hypotension was defined as systolic arterial pressure 70 plus twice the age in years and associated with altered peripheral perfusion. Bradycardia was defined as heart rate below 80 beats/ min for ages, 1 yr and 60 beats/ min for ages above 1 yr. Failure of the caudal block was defined as an increase in HR or MAP >20% than pre incision values.7,8 STATISTICAL ANALYSIS The collected data were analyzed with IBM.SPSS statistics software 23.0 Version. To describe about the data descriptive statistics frequency analysis, percentage analysis was used for categorical variables and the mean and S.D were used for continuous variables. To find the significant difference between the bivariate samples in Independent groups the Unpaired sample t-test and the Mann-Whitney U test was used. To find the significance in categorical data Chi-Square test was used similarly if the expected cell frequency is less than 5 in 2×2 tables then the Fisher's Exact was used. In all the above statistical tools the probability value .05 is considered as significant level. RESULTS In this study, 5 failed caudal blocks were encountered. Those cases were excluded from the study. Age, gender, the weight of the children and duration of the surgery were comparable between both the intervention groups and were not statistically significant.
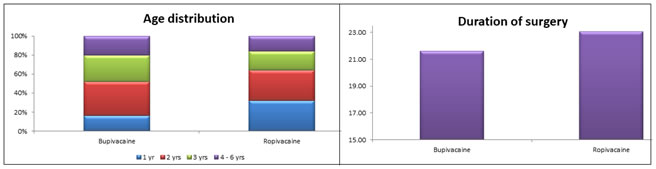
Graph 1: Age distribution Graph 2: Duration of Surgery
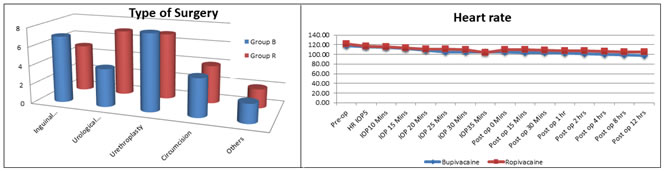
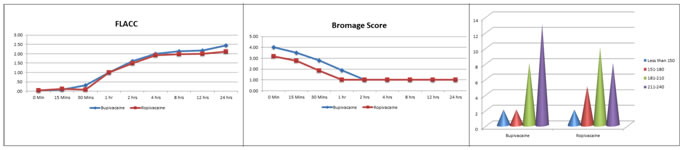
Graph 3: Type of Surgery Graph 4: Comparison of Heart Rate Between Two Groups Graph 5: Comparison of FLACC score Graph 6: Comparison of bromage score Graph 7: Duration of analgesia
Graph 1: shows the Majority of the Bupivacaine group patients belonged to the 2 years age class interval (n=9, 36%) with a mean age of 2.68 years. In Ropivacaine group patients majority belonged to the 1 year (n=8, 32%) and 2 years age class interval (n= 8, 32%) with a mean age of 2.32 years. The association between the intervention groups and age distribution is not statistically significant as p-value is greater than 0.05. In the Bupivacaine group, 20% were females (n=5) and 80% were males. In Ropivacaine group 16% were females (n=4) and 84% were males (n=21). The association between the two groups were statistically not significant. Graph 2: shows The mean duration of surgery in Group B was 21.60 and in Group R it was 23.04. The difference in means was not statistically significant. Graph 3: Shows the type of surgeries between both groups were comparable, but not statistically significant. Graph: 4 The difference in mean heart rate between Group B and Group R during pre-operative, intra-operative and post-operative periods are considered to be statistically insignificant as the p-value is greater than 0.05 as per unpaired t-test. Graph 5: The difference in FLACC pain score between the two groups during the post-operative period was statistically insignificant according to the Mann-Whitney U test (p-value greater than 0.05). Graph 6: shows The mean Bromage score was more in the Bupivacaine group when compared to the Ropivacaine group during the early post-operative period from 0 mins-1 hour. This difference was statistically highly significant with a p-value less than 0.01 according to the Mann-Whitney U test. Graph 7: shows Majority of patients in the Bupivacaine group belonged to 211-240 minutes time of duration of analgesia class interval with a mean time of 216 minutes. In Ropivacaine group majority of patients belonged to 181-210 minutes class interval with a mean time of 204.50 minutes. The difference in duration of analgesia between the two groups was statistically not significant (p-value greater than 0.05).
DISCUSSION Regional anesthesia techniques are commonly used in pediatric patients for intraoperative analgesia and post-operative pain relief. Regional techniques are advantageous since there is a little requirement of systemic narcotics and there is a resumption of early feeding as well as early ambulation.9 For surgeries below the umbilicus, caudal anesthesia was the most commonly used procedure which was simple, safe and effective.10 It provides excellent analgesia during surgery and also during the post-operative period in lower abdominal surgeries in children. Bupivacaine is commonly used local anesthetics for caudal anesthesia with good success, while ropivacaine has been extensively used for regional anesthesia in adults and children.11 In the caudal block, the duration of analgesia depends on the volume and concentration of local anesthetics as well as the concentration of the adjuvant used. The volume of local anesthetic required in the caudal block is directly proportional to the weight; the larger volume of the drug increases the cephalad spread leading to higher levels of block.12 Motor blockade resulting from the caudal block is a very distressful situation for children in the postoperative period and it delays hospital discharge. Ropivacaine when compared to Bupivacaine, has less motor blockade, a wider margin of safety, less cardiovascular /neurological toxicity and similar duration of analgesia.13 It can be safely used for regional anesthesia and analgesia in the ambulatory setting in pediatrics.In our study, we compared 0.25% bupivacaine and 0.2% ropivacaine for a single injection caudal anesthesia in children undergoing lower abdominal surgeries. Both the groups were homogenous with reference to age, weight, gender, and duration of surgery and found no statistically significant difference between the two groups.14 Intraoperatively and postoperatively, no statistically significant differences with respect to mean heart rate and systolic blood pressure, diastolic blood pressure and mean arterial pressure were noted between the groups. Manjushree Ray et al did a comparative study between 0.375% Bupivacaine and 0.375% Ropivacaine administered caudally in pediatric patients undergoing lower abdominal surgeries. All vital parameters were comparable throughout the peri-operative period. They concluded that caudal anesthesia with Ropivacaine 0.375% in pediatric patients was effective with less motor block during the post-operative period. Our study showed that 0.2% Ropivacaine produced less motor block when compared to 0.25% Bupivacaine in the early post-operative period.15 S. M. Walker et al conducted a study comparing 0.25% Bupivacaine and 0.25% Ropivacaine, 0.75ml/kg, administered caudally in pediatric patients undergoing urogenital surgeries. This study showed that hemodynamic parameters, quality, and duration of analgesia were comparable between the two groups, but the motor blockade was significantly less in the Ropivacaine group.16 ANAND K J, et al compared caudal Ropivacaine, 0.25%, 1ml/kg with Bupivacaine, 0.25%, 1ml/kg, in 81 children undergoing ambulatory procedure. They observed that Ropivacaine provided adequate postoperative analgesia with no difference from Bupivacaine in quality and duration of pain relief, motor/sensory effects or time to first micturition.Our study also showed no difference in quality and duration of analgesia between Bupivacaine and Ropivacaine group, but the motor block was found to be less with Ropivacaine group compared to the Bupivacaine group.17 Gaurav Kuthiala et al conducted comparative study between caudally administered 0.2% Bupivacaine and 0.2% Ropivacaine, 0.5ml/kg, in paediatric patients undergoing circumcision and showed that there were no significant differences in pain intensity and degree of motor blockade between the two groups upon awakening from anesthesia, and 1 and 2 hours post-caudal injection. The times to unsupported ambulation and discharge were also similar for both groups. Our study results were contradictory to this, which showed a high mean Bromage score in the Bupivacaine group than in the Ropivacaine group during the 1st postoperative hour which means motor blockade is less with Ropivacaine.18 Da Conceicao MJ et al. did a comparative study between 0.25 % Bupivacaine and 0.2 % Ropivacaine and 0.2% Levobupivacaine administered caudally in the pediatric age group undergoing infra-umbilical surgeries. This study found that there is no significant difference in the effect of analgesia in all the three groups but the duration of analgesia is longer in the Bupivacaine group. The group receiving Bupivacaine had high residual motor blockade and prolonged duration of the block than Levobupivacaine and Ropivacaine. In our study also Bupivacaine group showed high residual motor blockade and prolonged duration of block compared to the Ropivacaine group.19,20
CONCLUSION The study results conclude that 1 ml/kg of caudal Bupivacaine (0.25%) and 1 ml/kg Ropivacaine (0.2%) provides effective postoperative analgesia in children. But Ropivacaine given caudally provides less motor blockade as compared to Bupivacaine, making it a suitable agent for day care surgery with an increased safety margin, particularly in younger children.
REFERENCES
|
|
 Home
Home