Official Journals By StatPerson Publication
|
Table of Content - Volume 10 Issue 2 -May 2019
Poonam K Raipurkar1, Aparna G Kulkarni2*, Abhimanyu S Tarkase3
1Assistant Professor, Department of Anaesthesiology, Government Medical College, Nagpur, Maharashtra, INDIA. 2Associate Professor, 3Professor and Head, Department of Anaesthesiology, S.R.T.R. Rural Government Medical College, Ambajogai, Dist. Beed, Maharashtra, INDIA. Email: aparna.saumitra@gmail.com
Abstract Background: Monitored anaesthesia care (MAC) has gained importance in anaesthesia for both diagnostic and therapeutic procedures in view of providing safe sedation, controlling patient’s anxiety and pain control. MAC typically involves administration of local analgesics with IV sedatives, anxiolytics and/or analgesic drugs and is widely used in many ENT surgical procedures. The present study was carried out to compare the sedative and hemodynamic changes of combination of dexmedetomidine and midazolam versus midazolam and fentanyl during modified radical mastoidectomy. Material and Methods: 100 patients of ASA grade I and II, posted for modified radical mastoidectomy were randomly divided in two groups of 50 each. Group DM received injection dexmedetomidine 1 μg/kg and injection midazolam 0.06 μg/kg as loading dose followed by infusion of dexmedetomidine 0.5 μg/kg/hr, while group MF received injection midazolam 0.06 μg/kg and injection fentanyl 1 μg/kg as loading dose followed by infusion normal saline as placebo. Both the groups were studied with respect to the amount of sedation, hemodynamic changes and surgeon satisfaction. Results: The difference in the Ramsay sedation score and visual analogue scale was statistically significant in the two groups with significant sedation in DM group as compared to MF group. Also the number of doses of rescue analgesics, rescue sedation and rescue local infiltration was significantly less in DM group. The patient and surgeon satisfaction score was more in DM group than the MF group and the difference was statistically significant. The heart rate and blood pressure were significantly lower in DM group during administration of loading dose but were stable throughout. Conclusion: Finally to conclude, combination of dexmedetomidine and midazolam is better than combination of midazolam and fentanyl in modified radical mastoidectomy done under monitored anaesthesia care. Key Word: Dexmedetomidine, Midazolam, Monitored anaesthesia care, Modified radical mastoidectomy INTRODUCTION Monitored anesthesia care (MAC) has been described as a specific anesthesia service used for diagnostic or therapeutic procedures performed under local anesthesia along with sedation and analgesia, titrated to a level that preserves spontaneous respiration and airway reflexes, according to the latest American Society of Anesthesiologists (ASA) update in 20081 The three fundamental elements and purposes of a conscious sedation during a MAC are: a safe sedation, the control of the patient anxiety and the pain control2. Many surgical procedures such as minimally invasive surgery, gastrointestinal endoscopy, and interventional or radiological procedures can be performed using a MAC. MAC typically involves administration of local anaesthesia in combination with IV sedatives, anxiolytic and/or analgesic drugs which is a common practice during various ENT surgical procedures. This is also called as conscious sedation or ‘twilight sleep’3. Commonly used medications for MAC are benzodiazepines, opioids and propofol and recently alpha-2 agonist Dexmedetomidine.4 These drugs provide better sedation and analgesia when given in combination. In the literature survey, we observed that there are very few studies available on comparing combination of dexmedetomidine and midazolam and midazolam and fentanyl for modified radical mastoidectomy under monitored anaesthesia care. Therefore, the present study has been envisaged with an intention to compare sedative and hemodynamic changes of combination of dexmedetomidine and midazolam versus midazolam and fentanyl during modified radical mastoidectomy.
MATERIAL AND METHODS After approval from the institutional ethical committee, the prospective, randomised double blinded study was carried out in 100 patients in the age group 18-45 years, both male and female, belonging to ASA grade I and II scheduled for modified radical mastoidectomy. Patients were explained about the procedure and only patients who were willing and co-operative were included in the study after obtaining their informed consent. Patients who were not willing, non co-operative, not nil by mouth, suffering from any drug allergy or pre-existing illness, history of sleep apnea or asthma, patients on psychotropic medications, with abnormal electrocardiogram and patients on a 2 agonists or antagonists were excluded from the study. Patients were randomised in two groups of 50 each using sealed envelope technique. IV line was secured in patients of both the groups and all patients were premedicated with inj. Ranitidine 1 mg I.V. and injection Ondanseteron 0.08mg I.V. The dexmedetomidine group (DM) received intravenous midazolam 0.06mg/kg and then intravenous dexmedetomidine 1 μg/kg over 10 min followed by a continuous infusion of 0.5 μg/kg/h using an infusion pump having 50 ml syringe whereas the fentanyl group (F) received intravenous midazolam 0.06 mg/kg plus intravenous fentanyl 1μg/kg over 10 min followed by continuous infusion of normal saline at 0.5 ml/kg/h using a 50ml syringe. During this period the patients were assessed every two minutes using Ramsay sedation score(RSS). The target end point was patient having RSS=3. If the target end point was reached before completion of the infusion, then the infusion was stopped and noted. After loading drug infusion, if any patient in either of the groups had lesser sedation score then bolus IV midazolam 0.01mg/kg was administered which was repeated till RSS was 3. The maintenance infusion in both the groups was commenced immediately, once the loading infusion was stopped. After completing the loading infusion of the drugs and when RSS of 3 was achieved, the blinded ENT surgeon administered local anaesthetic using 2% lignocaine with adrenaline (6-7 ml) (1:2,00,000) in the postauricular area to block greater auricular and lesser occipital nerves, in the incisura terminalis to block auriculotemporal nerve and the four quadrants of the external auditory canal. Surgery was commenced after confirming adequate analgesia. Intraoperatively heart rate (HR), mean blood pressure (MAP), respiratory rate and SpO2 were recorded 2, 5 and 10 min during loading infusion of the study drugs and thereafter at 15 min intervals in first hour, and thereafter every 30 min till the end of surgery. Intraoperative pain intensity was evaluated using Visual Analog Scale (VAS) (0-10). Inadequate analgesia was treated with infiltration of 2% lignocaine with adrenaline (2-3 ml) at the surgical site and noted. If the pain was still persistent and VAS >3, then rescue IV fentanyl in the dose of 1μg/kg was given. Total number of rescue doses of fentanyl during surgery were recorded. Maximum three doses of rescue analgesic was permitted for the patients in the study. Adverse events like bradycardia (HR <50 bpm), hypotension (drop in systolic blood pressure >30% of baseline or MAP <60 mmHg), hypertension (an increase in systolic blood pressure or MAP >30% of baseline), bradypnea (RR <8 breaths/min), desaturation (SpO2 < 90%), nausea, vomiting, dry mouth or any other event during or within two hours of the procedure were recorded . After completion of the surgery the patients were shifted to recovery room and monitored for hemodynamic parameters and requirement of postoperative analgesia. Similarly the surgeon and the patient satisfaction score was recorded with zero being least satisfied and 10 being most satisfied. The primary end point of our study was the patient satisfaction score using NRS from 0 to 10. Efficacy of the sedation technique was defined as the ability to complete the surgery without any rescue sedatives and analgesics. Safety of the technique was determined based on the frequency of analgesia/ sedation related intra or postoperative adverse events. Statistical Analysis: Statistical evaluation was done 2 independent sample t-test and Mann-Whitney U test. OBSERVATIONS AND RESULTS Table 1: Number of patients and age in years
By using 2 independent sample t-test the p-value > 0.05 therefore there was no significant difference between mean age (years) in Group DM and Group MF
Table 2: Gender of patients
By using Chi-square test the p-value > 0.05 and hence there was no significant difference between distribution of gender in Group DM and Group MF
Table 3: Weight of patients in kilogram
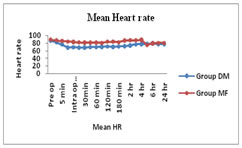
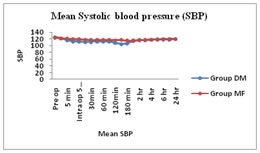
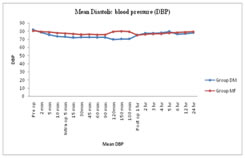
By using 2 independent sample t-test p-value > 0.05 there was no significant difference between mean weight (kg) in Group DM and Group MF. Figure1: Heart Rate in preoperative, intra-operative and post-operative period The difference in the heart rate between the two groups was statistically significant ( p<0.001) from five minutes after drug administration and lasted for throughout intra-operative period and four hours post-operatively as shown in fig. no. 1. Figure 2: Preoperative, intra-operative and post-operative systolic blood pressure The difference in the systolic blood pressure was statistically significant in the two groups (p<0.001) from 10 min to completion of surgery as shown in fig. no. 2 Figure 3: Preoperative to intraoperative and postoperative mean diastolic blood pressure By Mann-Whitney U test p-value < 0.05 which shows that there is statistically significant difference between patient satisfaction score and surgeon satisfaction score in group DM and group MF as shown in fig. No. 9
DISCUSSION Modified radical mastoidectomy is an operation to eradicate disease of the middle ear cavity and mastoid process, in which the mastoid and epitympanic spaces are converted into an easily accessible common cavity by removing the posterior and superior external canal walls. Modified radical mastoidectomy is mostly done under general anaesthesia as it requires steady field with minimal patient movement. But general anaesthesia for these surgeries has its own problems. Direct laryngoscopy and endotracheal intubation may not lead to serious complications in healthy patients but there are potential hazards of increase in sympathetic activity associated with laryngoscopy and intubation like hypertension, tachycardia, and dysrrhythmias. Also endotracheal intubation is associated with postoperative hoarseness of voice. General anaesthesia is also associated with increased blood loss at surgical site and prolonged exposure of the patients to the anaesthetic gases like inhalational agents and intravenous induction agents. These complications of general anaesthesia can be avoided by performing these procedures under local anaesthesia with intravenous sedation under monitored anaesthesia care. There are many advantages of local anaesthesia supplemented with intravenous sedation such as less bleeding at surgical field that leads to appropriate surgical field visibility, steady intraoperative haemodynamics, cost effectiveness, postoperative analgesia, faster mobilization of patient, and ability to test hearing intra-operatively as well as to detect injury to facial nerve intra-operatively. Many drugs are used under MAC. Commonly used medications are benzodiazepines, opioids and propofol. Occasionally, the administration of sedatives or hypnotics in conjunction with analgesics can cause significant respiratory depression and/or transient upper airway obstruction. Use of propofol for MAC has risk of cardiorespiratory depression, oversedation and disorientation.11 Also use of propofol has been associated with local anesthetic injection pain, more incidence of breakthrough pain, patient discomfort or patient movement. Hence use of propofol is not encouraged for MAC. Benzodiazepines like midazolam has been used for sedation in tympanoplasty and mastoidectomy. Though it has quick onset, it can cause prolonged sedation after prolonged use and repeated administration.5 Hence its use in combination with other drugs such as opiods like fentanyl or α2-agonists like dexmedetomidine is found to be advantageous. Since fentanyl has risk of respiratory depression it has to be used cautiously in patients with poor respiratory drive. Dexmedetomidine is a new potent alpha 2 agonist with its action on the locus ceruleus, inhibits sympathetic stimulation, and provides analgesia and sedation without respiratory depression and haemodynamic instability.6 Sedation is achieved when patients are undisturbed, but they can be easily aroused with minimal stimulation allowing for the performance of frequent neurological examinations. In our study we compared effect of dexmedetomidine and midazolam with midazolam and fentanyl in modified radical mastoidectomy under monitored anaesthesia care. Dexmedetomidine drug was studied previously by many authors and have shown that it can be used to provide sedation, analgesia and bloodless field for surgeries under LA resulting into high surgeon and patient satisfaction.7,8 Most of the studies done on dexmedetomidine are supportive. In our study the age, sex and weight were comparable in both the groups and hence bias due to these factors was minimised. While comparing the hemodynamics it was observed that intraoperative hemodynamics like pulse rate and blood pressure are more stable in DM group as compared to MF group. This could be explained by markedly decreased sympathetic activity of dexmedetomidine in DM group. By attenuating sympathetic activity, it inhibits norepinephrine release and produces predictable, dose-dependent reduction in the arterial blood pressure and heart rate.7,8 These effects prove advantageous in microsurgeries on middle ear in which even a small amount of blood will obscure the surgeons view. Mean heart rate in DM group was significantly lower at 2,5 and 10 min during loading infusion of drugs as well as at 5,15,30,45,60,90,120,150,180 min of intraoperative period as compared to MF group (P<0.0001). The difference in the two groups was statistically significant. This shows that dexmedetomidine provides better analgesia and sedation intra-operatively resulting in stable hemodynamics whereas fentanyl group had slight pain intra-operatively which led to sympathetic stimulation and increase in heart rate. Similarly there was a statistically significant decrease in mean systolic and diastolic blood pressure at 5 and 10 min of loading infusion and at 5,15,30,45,60,90,120,150,180 min of intaoperative period in DM group as compared to MF group (P<0.0001). This was because of adequate sedation and analgesia provided by dexmedetomidine causing less sympathetic stimulation. In addition, the property of dexmedetomidine to cause hypotension has contributed to this finding. This effect has advantage of providing bloodless field for the microscopic surgeries of ear and hence adds to a surgeon satisfaction. Similar finding was observed by Devangi A Parikh et al7, Alhashemi JA et al8, Memon N et al9, Bishnoi V et al10, Vyas DA11 et al. In the present study, respiratory rates were comparable at their baseline and there was no evidence of decrease in respiratory rate i.e. bradypnea in either of the groups. These findings are in accordance with the findings in other studies like Devangi A Parikh et al. Dexmedetomidine is unique in that it does not cause respiratory depression because its effects are not mediated by the gamma aminobuteric system. In the present study, saturation i.e.SpO2 was comparable at baseline and there was no evidence of desaturation at any time in either of the groups. In our study, all patients in both groups reached RSS of 3 at the end of loading dose infusion and no additional supplementation was required. Three patients from group DM required stopping of loading dose infusion before 10 min as they had reached target RSS of 3 which shows that sedation is achieved earlier with dexmedetomidine. This result of our study was in accordance with study conducted by Devangi A Parikh.7 In present study, there was no statistically significant difference in mean RSS between group DM and group MF at 2,5 and 10 min during loading infusion and at 5,15,30,45 ,60, 90,180 min during intra-operative period and during postoperative period. But the difference in mean RSS in both the groups was statistically significant at 90 and 180 min. This finding could be due to the analgesic effect wearing off at 90 min after administration of fentanyl in group MF while the analgesic effect was persistent in DM group. This shows that dexmedetomidine provides smooth intra-operative analgesia resulting in patient’s comfort. In our study, in group DM, 3 patients required one dose and 1 patient required three doses of rescue analgesia and in group MF significantly more number of patients required rescue analgesia with 5 patients requiring one dose, 10 patients requiring two doses and 7 patients requiring three doses. That’s why difference in number of rescue analgesia was statistically significant between group DM and group MF (P<0.001). The results were comparable with the study carried by Devangi A Parikh et al7 In the present study, 4 patients from group MF required rescue sedation with the midazolam during intraoperative period. No patients from group DM required rescue sedation, and the difference was statistically insignificant. This finding was comparable with the finding by Devangi A Parikh et al7 but were in contrast with the study conducted by Zeyneloglu et al12 where more rescue sedation was required in dexmedetomidine group. In our present study, in group DM, 6 patients required rescue local infiltration and in group MF 18 patients required rescue local infiltration with 2% lignocaine with adrenaline. Therefore there was significant difference between requirement of rescue infiltration in group DM and group MF(P 0.009) (P<0.05). This finding was in accordance with the study conducted by Memon N et al9 The surgeon satisfaction score was more in DM group as compared to MF group due to better analgesia and sedation and bloodless surgical field provided by dexmedetomidine. This makes dexmedetomidine a better option for surgeries under MAC. Bishnoi et al10, Candiotti KA et al13 and Na HS et al14 have also reported better satisfaction scores with dexmedetomidine. While comparing the side effects, the incidence of bradycardia was more in DM group than MF group but the difference was not statistically significant. In our study, we didn’t observe other side effects associated with drugs like hypotension, shivering, nausea and vomiting, respiratory depression and itching.
CONCLUSION Finally to conclude, combination of dexmedetomidine and midazolam is better than combination of midazolam and fentanyl in tympanoplasty and modified radical mastoidectomy done under monitored anaesthesia care as it provides. Stable intraoperative and postoperative haemodynamics as compared to fentanyl that causes less surgical bleeding and improves visibility of surgical field. Better intraoperative and postoperative sedation and analgesia and decreased number of doses of rescue analgesia, rescue sedation and rescue local infilteration as compared to fentanyl during intraoperative period. Decreased number of doses of rescue analgesia in postoperative period. Higher patient and surgeon satisfaction score as compared to fentanyl. No side effects/complications and no effects on respiration and saturation during intaoperative and postoperative period. So, the patient remains comfortable in the intra-operative and postoperative period with considerable therapeutic benefit and without any potential side effects.
ACKNOWLEDGMENTS Special thanks to the postgraduate students of Department of Anaesthesiology, S.R.T.R.G.M.C, Ambajogai, for their valuable support
REFERENCES
|
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||
 Home
Home