Effect of intrathecal labor analgesia using fentanyl 25μg alone and fentanyl 20μg plus bupivacaine 2.5mg on the progress of labor
Gowrisree Kadimi1, Gopal Reddy Narra2*, Gopinath Sayani3, Pratusha4, Showri Reddy5
{1Assistant Professor, Department of Gynaecology} {2Professor, 3,4,5PG, Department of Anaesthesiology} Kamineni Institute of Medical Sciences; Narketpally, Telangana, INDIA.
Email: drgopalreddynarra@yahoo.com
Abstract Background: The aim of this study was regarding the effect of intrathecal analgesia using fentanyl or fentanyl and bupivacaine combination during normal vaginal delivery on onset and duration of analgesia, pain scores in the mother, on the progress of labor and hemodynamic changes in the mother and fetus. Materials and Methods: Sixty primigravida in the active phase of labor with a cervical dilatation of> 3to <5 cm was selected for this prospective study. Group A (n = 30) received an intrathecal injection fentanyl 25 μg only compared with Group-B(n = 30) with 20 μg of fentanyl plus 0.5% hyperbaric bupivacaine 2.5 mg. Result: Onset of sensory blockade 3.88±0.1min in group-A and 3.64±0.06min in the group –B. Duration of sensory block 138.23±13.55 and131.83±12.45 in both the groups respectively, p-value, 0.05. Duration of the active phase of first stage of labor was slightly shortened in group A as compared to group-B (117.9vs118.37) min. Duration of the second stage of labor was slightly prolonged in group-B as compared to group A (22.2vs25.07min,) and significant p-value. Rate of cervical dilation was faster in group A as compared to group-B (1.9 3 vs. 1.94 cm/h). Statistically significant changes noticed in the mean visual analog score, pulse rate, and mean arterial pressure and the fetal heart rates from the base level to at 4th and 10 min in their respective in A and B groups. Conclusions: Single-shot intrathecal analgesia with fentanyl. 25 μg or fentanyl 20 μg +bupivacaine 2.5 mg useful when given in the active phase of first stage of labor had a rapid onset with a satisfactory pain relief in both the groups and minimal motor block in group-B, with VAS scores <4 and good maternal and fetal hemodynamic.
Key Word: Labor pain, Labor Analgesia, fentanyl, bupivacaine, intrathecal injection.
INTRODUCTION
The pain of childbirth is the most painful condition that many women have to bear. The pain of the early first stage of labor arises from dilation of the lower uterine segment and cervix. The pain of the late first stage and second stage of labor arises from the descent of the fetus in the birth canal, resulting in distension, stretching and tearing of tissues in the vagina and perineum1, Labor pain is excruciating and contributing to fear, stress, and anxiety. Painful uterine contractions leading to maternal hyperventilation and hypoventilation, increased catecholamine concentration resulting in maternal metabolic changes and fetal hypoxemia.2 Labor pain when unrelieved has adverse effects on the course of labor. Effective labor analgesia leads to better and safe labor for both the mother and baby. Epidurals have long been associated with increased oxytocin use, increased fetal malposition, increased rates of instrumental and caesarean delivery, and longer labor3, But the spinal block is cheaper as well as less technically challenging when compared to the epidural. Opioid alone or combined with a small dose of local anaesthetic provides rapid analgesia. Use of lower doses of bupivacaine is having least placental transfer property, due to high rotein binding and minimal motor block compared to sensory block. It has become a popular choice for labor analgesia. In view of the above, the present study was undertaken to compare the progress of labor as the primary outcome and hemodynamic changes in the mother and fetus as a secondary outcome in parturients. Group A in received intrathecal labor analgesia using fentanyl 25 μg and group B received and fentanyl 20 μg plus bupivacaine 2.5 mg as neuraxial analgesia during normal vaginal delivery.
MATERIALS AND METHODS
After approval from the Institutional ethical committee and obtaining written and informed consent from patients, 60 primi parturients at term pregnancy (American society of Anaesthesiologists physical status grade I and II), aged between 20-25 years were recruited for this prospective study between Jan2018 to Feb-19. Only patients with singleton pregnancies and vertex presentation who were in the active phase of labor with a cervical dilatation of more than3 cm and normal fetal heart rate (FHR) tracings were enrolled for this study. Patients in the group A (n = 30) received an intrathecal injection of fentanyl 25 μg and group-B fentanyl 20 μg plus 0.5% hyperbaric bupivacaine 2.5 mg (0.5 ml) and all volumes made to 1.5 ml with normal saline. The two groups were evaluated with regards to the progress of labor, maternal hemodynamic variations, fetal heart rate, and neonatal outcome during labor in parturient undergoing normal vaginal delivery. Whenever foetal distress noted patient was taken for caesarian section and they were excluded from the study. After securing intravenous line with an 18 G cannula the parturients were preloaded with 500 ml of ringer's lactate solution; oxygen was administered by nasal cliffs at 2 L/min. To perform the block, parturients were placed in a left lateral position and the L3-L4 interspace was identified and 25 G spinal needle was used to enter the subarachnoid space. After return of clear cerebrospinal fluid, patients were given a single intrathecal injection of solutions mentioned previously. Then, parturients were repositioned in a supine position with left uterine displacement. The block was given by trained anaesthetist under aseptic precautions and recordings done by obstetrician. No patients were allowed to walk during the study period due to the need for continuous maternal and fetal monitoring for safety reasons. All vitals recordings including onset, duration of sensory block, pain scores were recorded by anaesthetist and the frequency and intensity of uterine contractions, dilation, and effacement of the cervix, descent of the presenting part, and requirement of oxytocin and foetal recordings done by the obstetrician. APGAR scores were recorded by Pediatrician.
Statistical analysis: Statistical analysis was performed using software Statistical Package for the Social Sciences SPSS). Unpaired and paired student t-test was used to analyze the data; P-value of 0.05 was considered to be significant.
OBSERVATIONS AND RESULTS
Table 1: Parturients characteristics
S.No |
Characteristics |
Group-A (n=30) |
Group-B (n+30) |
1 |
Age |
22.27±1.7 |
22.37±1.75 |
2 |
Height |
160.2 ±2.9 |
160.8±2.69 |
3 |
Weight |
64.9±4.61 |
64.53±4.7 |
4 |
Cervical Dilatation |
4.23±0.58 |
4.22±0.59 |
5 |
oxytocin units used |
7.17±1.47 |
7.2±1.24 |
6 |
VAS score baseline |
7±0.64 |
7.13±0.63 |
7 |
Onset of sensory block |
3.88 ± 0.1 |
3.64±0.06 |
8 |
Duration of sensory block |
138.23 ± 13.35 |
131.83± 12.45 |
Both groups were almost similar in terms of age, height and weight of parturients. Both groups are comparable in terms of mean cervical dilation and VAS score at the time of study initiation [Table 1]
Table 2: Mean visual analog scale score
S.No |
Time in Minutes |
Group-A (n=30) |
Group-B
(n+30) |
p-value |
1 |
0 |
7±0.64 |
7.13±0.63 |
0.16 |
2 |
4 |
3.73±0.74 |
3.6±0.67 |
0.16 |
3 |
10 |
2.5±0.57 |
2.53±0.56 |
0.32 |
4 |
20 |
2.4±0.49 |
2.43±0.5 |
0.33 |
5 |
40 |
2.46±0.45 |
2.3±0.47 |
0.35 |
6 |
60 |
2.33±0.47 |
2.3±0.46 |
0.33 |
7 |
90 |
2.4±0.5 |
2.37±0.49 |
0.32 |
8 |
120 |
2.4±0.49 |
2.43±0.5 |
0.32 |
9 |
150 |
2.7±0.63 |
2.73±0.64 |
0.57 |
10 |
180 |
3.57±0.57 |
3.7±0.65 |
0.16 |
The VAS scores were similar in both the groups that were provided intrathecal analgesia at all time intervals are comparable [Table 2] less than 4 till delivery and rate of cervical dilations were also almost similar.
Table 3: Comparison of the progress of labor
S.No |
Characteristics |
Group-A (n=30) |
Group-B
(n+30) |
p-value |
|
Duration of active 1st stage in min |
117.9±10.65 |
118.37±8.39 |
0.83 |
2 |
Duration of 2nd stage in min |
22.2±2.22 |
25.07±4.521 |
0.003 |
3 |
Rate of cervical dilatation cm/h |
1.93±0.23 |
1.94±0.21 |
0.84 |
4 |
APGAR score 2min after birth |
6.93±0.77 |
6.83±0.63 |
0.58 |
5 |
APGAR score
5min after birth |
8.87±0.67 |
8.84±0.58 |
0.83 |
Duration of 1st active stage of labor are comparable. But 2nd stage of labor is shortened in group-A when compared to group-B. Rate of cervical dilatation are also similar. APGAR scores at 2nd and 5th mins are comparable.
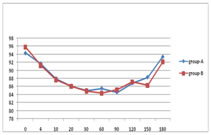
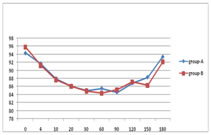
Graph 1: Pulse rate Graph 2: Mean arterial pressure
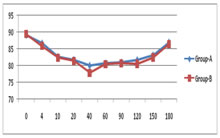
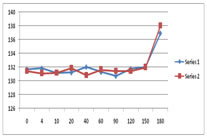
Graph 3: Fetal heart rate
Both A and B groups are comparable regarding maternal pulse rate during labor. Both A and B groups are comparable regarding mean arterial pressures. Both A and B groups are comparable regarding foetal heart rate.
DISCUSSION
Clement P et al4 studied intrathecal narcotics for labour analgesia and found that they represent a safe and effective alternative to conventional epidural analgesia and provide significant, rapid relief of labour pain. Hence, the intrathecal injection was administered in the active phase of labor (>3 cm cervical dilation) in our study. Intrathecal fentanyl 25 μg in group-A and in group-B fentanyl 20 μg plus 0.5% hyperbaric bupivacaine 2.5 mg were used in our study. At these doses, onset was rapid, duration of analgesia also maximum with a least maternal and fetal side effect. Bupivacaine was added to relieve somatic pain.3 The onset of labor analgesia was very rapid. The mean onset of sensory block was 3.88 ± 0.1 and 3.64±0.06 mins in group-A and group-B respectively and the value is clinically significant. The highest level of sensory block attained was T8 in 20%, T9 in 70%, and T10 in 10% of group A and T8 in 16.67%, T9 in 66.67% and T10 in 16.67% in group-B. The duration of analgesia was 138.23 ± 13.35 min in group-A and 131.83± 12.45in group -B [Table-1] with significant p-value<0.05. The parturients of both groups had excellent pain relief throughout labor. Group A parturients experienced pain at the time of delivery of baby, although the VAS score was less than 4. Potdar et al.5,6 reported a similar result in both groups. Duration of the active phase of first stage of labor was slightly shortened in group A as compared to group-B (117.9vs118.37) min. Duration of the second stage of labor was slightly prolonged in group-B as compared to group A (22.2vs25.07min,) and significant. Rate of cervical dilation was faster in group A as compared to group-B (1.9 3 vs. 1.94 cm/h). (Table-1). The mean VAS scores at the base level, 4th min and 10th min were very significant in when compared with their own group. The VAS scores were7±0.64at base level, 3.73±0.74at 4th min and 2.5±0.57 at 10th min in group –A. Whereas in group-B they were 7.13±0.63 at base level3.16±0.67 at 4th min and2.53±0.56min respectively and clinically significant for the specific group-B, as the p-values are less than0.05inbith respective groups [Table-2]. Craig M Palmer et al5,6 studied the dose and found a median effective dose of fentanyl is 14µg. The Mean VAS scores were less within 5 minutes post-injection in 20-25µg groups and within 10minutes post-injection in 15µg group. Also, there was no benefit to increasing the dose beyond 25 µg, when used as sole agent for intrathecal labour analgesia. Cascio M et al7 studied the effects of intrathecal fentanyl on plasma catecholamine levels in term laboring parturients and concluded that there was a significant decrease in plasma epinephrine levels by 52%. Because of this, the VAS) scores were decreased and in turn reducing the stress of labor. There was a significant reduction in pulse rate and mean arterial pressures at 4th and 10th min when compared to baseline readings in both the groups. The pulse rates at the base level, at 4th min and at 10th min were 94.33and95.8, 91.7and91.23 and87.96and87.68 in both the groups A and B and They are clinically significant at the given timings [Graph-1]. The mean arterial pressures were 89.08and89.36 at the base level,86.6and82.66 at 4th min and 85.86and82.37 at10th min in group-A and Group-B [Graph-2]. They are clinically significant at the given timings in their respective groups as p-value is<0.05. Mandell GL et al8 studied the hemodynamic effects of subarachnoid fentanyl 25µg in laboring parturients and noticed a decrease in maternal blood pressures and also the heart rates. This was attributed to the decrease in catecholamine levels and pain scores in the mother. Bindu HN et.al9 studies correlate well with our study because our study observed a significant decrease in VAS scores post injection of intrathecal fentanyl in all the groups. In our study, the mean VAS scores were<4 within 4 minutes post-injection in both the groups: We concluded that epidural analgesia did not affect the duration of labor or cesarean section rate and has no effect on perinatal outcome and can, therefore, be recommended to mothers as a satisfying and effective method of pain relief during labor. The mean duration of the second stage of labor was significantly prolonged in group A (22.2 ± 4.27 min) as compared to group B (25.15± 5.46 min). This difference was statistically significant (P < 0.003). Further, recent studies suggest that a longer second stage is, in itself, not harmful to the mother or neonate as long as the FHR pattern is reassuring and there is ongoing descent of the fetal head. The possible reason for a prolonged second stage in group-B could be the relaxation of the abdominal wall musculature secondary to neuraxial local anaesthetic resulting in decreased effectiveness of maternal expulsive efforts.13 Changes in the mean heart rate and blood pressure did not require any intervention throughout the observed period. Mendall et al.8 had investigated effect of subarachnoid 25 μg fentanyl in parturients and observed a significant decrease in heart rate and systolic blood pressure and diastolic blood pressure after 25 min, which was not due to vasodilatation but due to the onset of effective analgesia. In our study, intrathecal labor analgesia in healthy parturients was not found to be associated with any FHR abnormalities, fetal distress or adverse neonatal outcome. ecreasing epinephrine due to effective labor analgesia causes an increase in the uterine tone, which will decrease placental blood flow and may subsequently lead to fetal bradycardia. There were no significant changes in FHR as compared to the baseline in both the groups, and none resulted in intervention for fetal compromise. All FHR decelerations prior to and after intrathecal analgesia administration were transient [Graph 3]. The mode of delivery in most of the parturients was vaginal delivery and only a few required LSCS. The parturients who required caesarean section due to fetal distress were not excluded from the study. APGAR score at 2minute remained between 5 or 7 and at 5 minutes remained between 7 and 9 in all neonates of both the groups. No neonatal respiratory depression was noted [Graph 3]. Nausea was reported in 9% parturients in group A and 6% parturients in group B; 9% parturients in group A 6% in group B complained of pruritus. Hypotension, bradycardia, vomiting, and fetal distress were not found in either group. There were significant changes observed in the APGAR scores at 2and5 min in respective groups. No neonatal respiratory distress was found in either group. Fyneface et al.10 also found APGAR score >7 and >9 at 2 and 5-min intervals after intrathecal administration of bupivacaine and fentanyl. The most common side effect was pruritus which was seen in 4 parturients of group A and 3 in group-B, which was mild and no intervention was required. In group A, 3 parturients complained of nausea as compared to 3 parturients of group B.
CONCLUSION
In conclusion we found that single shot intrathecal analgesia useful using fentanyl 25 μg or fentanyl 20 μg +bupivacaine 2.5 mg, when given in the active phase of the first stage of labor, had rapid onset with satisfactory pain relief in both the groups and minimal motor block in group-B, with VAS scores <4 and good maternal and fetal hemodynamics.
REFERENCES
-
Reena kasturi,Bandyopadhyay KH, Afzal M, Mishra AK, Paul A. Labor epidural analgesia: Past, present and future. Indian J Pain 2014;28:71-81.
-
Dilesh PK, Eapen S, Kiran S, Chopra V. A comparison of intrathecal dexmedetomidine verses intrathecal fentanyl with epidural bupivacaine for combined spinal epidural labor analgesia. J Obstet Anaesth Crit Care 2014;4:69-74.
-
Minty RG, Kelly L, Minty A, Hammett DC. Single-dose intrathecal analgesia to control labour pain: Is it a useful alternative to epidural analgesia? Can Fam Physician 2007; 53: 437-42
-
Potdar MP, Kamat LL, Jha T. Intrathecal isobaric ropivacaine-fentanyl versus intrathecal isobaric bupivacaine-fentanyl for labor analgesia: A controlled comparative double-blinded study. J Obstet Anaesth Crit Care 2014;4:12-7.
-
Palmer CM, Cork RC, Hays R, Van Maren G. Alves D. The dose response relation of intrathecal fentanyl for labor analgesia. Anesthesiology 1998; 88: 355-61.
-
Palmer CM, Van Maren G, Nogami WM, Alves D. Bupivacaine augments the effect of intrathecal fentanyl for labour analgesia. Anesthesiology 1999; 91: 84-9.
-
Cascio M, Pygon B, Bernett C, Ramanathan S. Effects of intrathecal fentanyl on plasma catecholamine levels in term labouring parturients. Society for Obstetric anesthesia and Perinatology Annual Meeting, Montreal, Quebec; 1995.
-
Mandell GJ, Jamnback L, Ramanathan S. Hemodynamic effects of subarachnoid fentanyl in laboring parturients. Reg Anesth 1996; 21: 103-11.
-
Bindu HN, Nisty GM, Impashree CM. Effects of Epidural
Analgesia on the Mother and Fetus in Labor. J Evol Med Dent Sci 2014;66: 14262-9.
-
Fyneface-Ogan S, Gogo Job O, Enyindah E. Comparative effect of single shot intrathecal bupivacaine with dexmedetomidine and bupivacaine with fentanyl on labor outcome. Anesthesiology 2012;2012:1-6.
 Home
Home