Official Journals By StatPerson Publication
|
Table of Content - Volume 10 Issue 3 -June2019
Prathibha Nair P U1*, Anand S2, Lailu Mathews3
1Post Graduate, 2Professor, 3Professor and HOD, Department of Anesthesiology and Critical care, Chettinad Hospital and research institute, kelambakkam, Chennai, INDIA. Email: drprathibhanair88@gmail.com
Abstract Background: Congenital diaphragmatic hernia results from incomplete closure of pleuroperitoneal fold during embryonic development which occurs around 8th to 10th week of gestation. Bochdalek hernia occurs as a result of defect in fusion of posterolateral part of diaphragm through which abdominal contents herniate into thoracic cavity. Left sided Bochdalek hernia is more common. Usually diagnosis is made during neonatal period. Presentation in adulthood is rare. Case presentation: This case report presents the anesthetic management of an elderly male with history of dyspnoea, orthopnoea, abdominal distension and was diagnosed to have left Bochdalek hernia with type II respiratory acidosis and corpulmonale who underwent laparotomy and diaphragmatic hernia repair. Conclusion: Diaphragmatic hernias are rare among adult population and hence arriving at correct diagnosis, proper preoperative evaluation, intra operative and post operative management is very crucial in preventing complications and improving the outcome. Key Word: Bochdalek hernia.
INTRODUCTION Congenital diaphragmatic hernia results from incomplete closure of pleuroperitonial folds during embryonic development. Bochdalek hernia is a type of congenital diaphragmatic hernia occurring as a result of defect in fusion of posterolateral part of diaphragm. Left Bochdalek hernia is the most common type of congenital diaphragmatic hernia. Most cases are diagnosed in neonatal period and rarely detected in adults.1 This case report presents the anesthetic management of an elderly male with left Bochdalek hernia with type II respiratory failure and corpulmonale who underwent laparotomy and diaphragmatic hernia repair.
CASE REPORT A 66 year old male diagnosed 6 months ago with diaphragmatic hernia and restrictive lung disease now presented with history of increasing difficulty in breathing, orthopnoea, drowsiness, bilateral leg swelling, decreased urine output and abdominal distension for 20 days duration. On examination, he was conscious, oriented, tachypnoeic, drowsy and cyanosed with 75% room air saturation. He had bilateral pedal edema extending till knees. His Heart rate was 96 beats per minute, blood pressure was 110/70 mmHg and respiratory rate of 34 per min. His chest examination revealed decreased air entry on left hemithorax. His abdomen was distended and shifting dullness was present. His chest x-ray revealed elevated diaphragm on left side and mediastinal shift to right (fig 1). His prior HRCT showed large defect of 10×9 cm defect in postero-lateral aspect of left hemi diaphragm and herniation of spleen, stomach, pancreas and splenic flexure through the defect into the left hemithorax and mediastinal shift to right side. Left lung was hypoplastic and fibrotic changes were noted in apico-anterior segment of left upper lobe with bilateral basal atelectasis (fig 2). His echocardiography revealed ejection fraction of 60%, mild PAH, dilated RA/RV, situs solitus. His arterial blood gas analysis showed type II respiratory failure with chronic respiratory acidosis with compensatory metabolic alkalosis pH was 7.2, PaCO2 of 93.5mmHg, PaO2 of 88.2mmHg, HCO3- of 36.7mmol/L (on 40% O2 through Venturi mask). Patient was initiated on NIV. But, patient’s PaCO2 remained high greater than 65mmHg and pO2 started to fall. 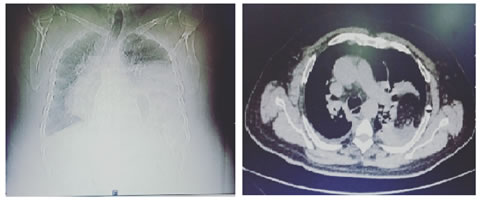
Figure 1 Figure 2 Figure 1: preoperative chest x ray revealing elevated diaphragm on left side and mediastinal shift to right, Figure 2: preoperative CT chest showing presence of abdominal organs in the thorax and mediastinal shift to right. In view of worsening respiratory failure, patient was intubated and put on pressure control ventilation FiO2 0.8%, PEEP 10cms of H2O, RR 14/min, pressure control 20 cm of H2O. Patient was maintained on paralysis and sedation. After three days of ventilation his arterial blood gas analysis improved to pH of 7.429, pCO2 50.4mmHg, pO2 103mmHg with FiO2 of 0.4. His Potassium was 2.5mmol/L (potassium correction started) and sodium was 132mmol/L. A rare case of congenital Bochdalek hernia with hypoplastic left lung who presented in 7th decade of life with type II respiratory failure with corpulmonale was stabilized, optimized and was taken up for emergency laparotomy and diaphragmatic repair under ASA IV. In the operating room, routine monitoring was done with ECG, NIBP, pulseoximeter, EtCO2. Arterial catheter was inserted into the left radial artery for continuous blood pressure monitoring. Right internal jugular vein was cannulated for CVP monitoring. Morphine 10mg i/v, propofol 2mg/kg i/v and Atracurium 0.1mg/kg I/V was administered and patient was mechanically ventilated with Pressure Control mode (FiO2 0.4%, pressure control ventilation at 22 cm of H2O delivered 300- 350 ml of tidal volume, PEEP 10cm of H2O, respiratory rate 14/min). Anesthesia was maintained with oxygen, air and isoflurane. Atracurium was given intermittently to maintain neuromuscular blockade. Paracetamol and morphine was used for intraoperative analgesia. Patient remained hemodynamically stable throughout the surgery. His blood pressure was maintained between 130/80 mmHg and 150/90mmHg. His heart rate remained between 65 and 80 beats per minute. His saturation was maintained around 97% and CVP was maintained around 6-8 mmHg. Intraoperative Arterial Blood Gas analysis showed pH 7.44, PaO2 102mmHg, PaCO2 of 48.8mmHg, bicarbonate 33.2, sodium 136mmol/L and potassium 2.4mmol/L and hence potassium correction was continued. After reduction of contents, his tidal volume and lung compliance improved and we could come down on pressure control to 12 cm of H2O. Surgery lasted for 3 ½ hours. Patient was shifted back to ICU and mechanical ventilation continued. Post operatively, his lung compliance improved and his arterial blood gas analysis became normal. On 4th post operative day patient was extubated and shifted to ward.
DISCUSSION Congenital diaphragmatic hernia results from incomplete closure of pleuroperitonial folds around 8th to 10th week of embryonic development. Bochdalek hernia is presence of defect in posterolateral part of diaphragm2,3. This condition is usually associated with other malformations like pulmonary hypoplasia, cardiac malformations and malrotation of gut2. It is usually diagnosed during postnatal period when neonate presents with acute respiratory distress1,2. Adults usually have mild and chronic presentations like dyspnoea, orthopnoea, reduction in lung volume and hypoxia4. Presence of abdominal viscera in the thorax causes direct compression of heart, mediastinal shift by causing mass effect. Repeated chest infection, gastro intestinal disorders and palpitation may be present in some patients due to mass effect4. Our patient also presented to us in 7th decade with short history of repeated chest infection, dyspnoea, orthopnoea, and pulmonary hypoplasia. For control of infection, antibiotics, oxygen therapy and upright positioning may be needed in some symptomatic adult patient. Surgical correction may be needed in patients not responding to medical management4. Our patient didn’t show any improvement with medical management hence necessitating surgical repair for improvement of respiratory status. Anesthetic management of a case of diaphragmatic hernia requires securing a large gauge intravenous cannula, arterial line cannulation, central line cannulation and CVP monitoring4. Any cause leading to rise in intra abdominal pressure should be avoided. Compression of vena cava and pulmonary veins impairs venous return to heart and decreases the cardiac output4,5,6. Adequate depth of anesthesia must be maintained. Use of nitrous oxide should be avoided, as the expansion of intra abdominal viscera can impair both respiration and circulation4, 6. Lung compliance is very much reduced in our patient probably due to the mass effect produced by the abdominal contents in thorax. The presence of restrictive lung disease and lung hypoplasia with fibrotic changes can also be the other causes of decreased lung compliance in our patient. Decreased lung compliance necessitates the use of high pressure to maintain tidal volume at the start of surgery. But after reducing the contents, lung compliance improved and tidal volume was maintained with lower pressure. Because of the presence of hypoxia, acidosis and decreased lung compliance, elective ventilation was considered to aid in improving the oxygenation as well as preventing rise in intra abdominal pressure and preventing excessive strain to diaphragm. CONCLUSION In conclusion, diaphragmatic hernia in adult is very rare. Proper preoperative evaluation of patient’s condition, assessing the level of severity and preoperative optimization is very essential. Intraoperative management should aim at preventing increase in intraabdominal pressure and maintaining lung compliance and adequate oxygenation. Postoperative management should be directed towards maintaining adequate oxygenation, preventing pain and increase in intra abdominal pressure and other supportive therapies to improve lung compliance will improve the postoperative outcome.
REFERENCES
|
|
 Home
Home
