Official Journals By StatPerson Publication
|
Table of Content - Volume 12 Issue 1 -October 2019
Omprakash Verma1, Babita2, Bhupendra singh3*, Abhishek Kumar4, Surendra Jakhar5, M L Tak6
1IIIrd Year Resident, 3Assistant professor, 4,5 IInd Year Resident, 6Senior Professor, Department of Anaesthesia, S.N Medical College and Hospital. Jodhpur Rajasthan, INDIA. Email: vermaomprakash48@gmail.com, drbabita24@gmail.com, abhisekmgmmc@gmail.com, surendrajakhar08@gmail.com
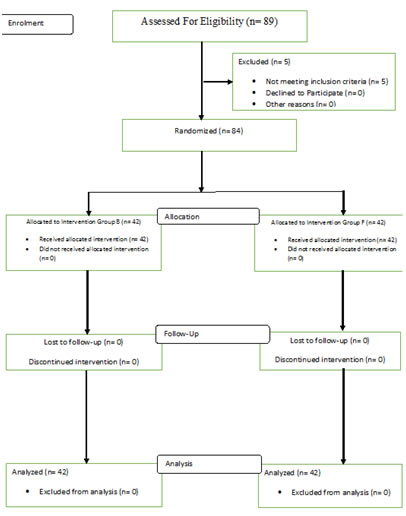
Abstract Background: For lower limb surgeries, neuraxial blockade is the preferred mode of anesthesia. Spinal block is still the first choice because of its rapid onset, superior blockade, less failure rates and cost effectiveness. The aim of current study is to compare the efficacy of Buprenorphine and Fentanyl added to intrathecal bupivacaine in orthopaedic procedures in lower limbs. Method: 89 patients scheduled to undergo lower abdominal and lower limb surgery were assessed, 5 excluded for not meeting inclusion criteria. Remaining 84 patients were divided randomly into two groups by computer generated random number sequence. Group B received 50μg of buprenorphine with 3cc (15mg) of Bupivacaine (heavy). Group F received 25μg of fentanyl with 3cc (15mg) of Bupivacaine (heavy). Results: Buprenorphine and Fentanyl with Bupivacaine in spinal anesthesia provide good quality intra operative and post-operative analgesia. Bupivacaine with Buprenorphine significantly prolongs sensory and motor block. Duration of Analgesia and Sedation are more in Buprenorphine group than Fentanyl group. Hemodynamic stability in both group were comparable and was statistically insignificant. Key Words: Spinal, Bupivacaine, Fentanyl, Buprenorphine
INTRODUCTION Effective management of peri-operative pain in lower extremity orthopedic surgery represents an important component of early postoperative recovery as it serves to blunt autonomic, somatic and endocrine reflexes with a resultant potential of decreasing perioperative morbidity.1 For lower limb surgeries, neuraxial blockade is the preferred mode of anesthesia. Spinal block is still the first choice because of its rapid onset, superior blockade, less failure rates and cost effectiveness, but has the drawbacks of shorter duration of postoperative analgesia and side effects such as hypotension and bradycardia resulting due to sympathetic blockade. Bupivacaine acts through reversible blockade of neuronal sodium channel and its higher lipid solubility makes it more potent than ropivacaine and results in a longer duration of action. Adjuvants like epinephrine 2, neostigmine 3, magnesium 4, midazolam 5, ketamine 6, and clonidine 7 have been added to intrathecal local anaesthetics in an attempt to prolong analgesia and reduce the incidence of adverse events. Opioids 8,9,10 are being used as intrathecal adjutants. However, significant adverse effects such as urinary retention, respiratory depression, hemodynamic instability, pruritus and occasionally severe nausea and vomiting, may limit their use. 11,12,13 Buprenorphine, a µ receptor partial agonist, centrally acting lipid soluble agent exhibits analgesic property both at spinal and supraspinal levels.14. Buprenorphine, is compatible with CSF and produces no or minimal adverse reactions like pruritis and nausea .It has high molecular weight and is lipophillic which may prevent its rostral spread and thus respiratory depression. It has consistently proven to prolong the duration of anaesthesia 15,16, Fentanyl is a potent synthetic µ receptor and it has local anesthetic action on the primary afferent sensory C nerve fibers causing analgesia. Till date, few studies have been reported on the effects of intrathecal fentanyl combined with local anesthetics in humans.09,18,19 In those studies, using 10–15 mg of bupivacaine and fentanyl(25 μg) prolonged the block duration of local anesthetics. There are no literature comparing the benefits and side effects of the drugs buprenorphine and fentanyl as adjuncts to bupivacaine for lower abdominal and lower limb surgeries. Hence, we undertook this study to investigate and compare buprenorphine and fentanyl as an adjuvant to hyperbaric bupivacaine for efficacy, hemodynamic stability, and duration of sensory and motor blockade, post-operative analgesia and side effects in lower abdomen and lower limb surgeries.
MATERIAL AND METHODS This study was carried out in the Department of Anesthesiology and Critical Care, Dr. S. N. Medical College and associated group of hospitals. A written and informed consent was taken from every patient. Sample size: A sample size of 42 in each group with 80% power to detect a difference between means of 142.28 with a significance level (alpha) of 0.05 (two- tailed). Inclusion criteria 1) American Society of Anesthesiologist [ASA] grade 1 and 2 patients. 2) Patients belonging to age group 18 - 60 years. Exclusion criteria 1) Patients with history of bleeding disorders or patients on anticoagulants 2) Patients with infection at the site of injection 3) Patients with allergy to local anaesthetics 4) Patients with cardiac disease, heart blocks, dysrhythmias, anemia, severe hypovolemia, shock, septicemia and neurological defects. 5) Patients on β-blockers and α-antagonists. 6) Anatomical abnormality at the regional site 7) Pregnant women PRE ANAESTHETIC EVALUATION: •During preoperative visits, patients’ detailed history, general physical examination and systemic examination and routine blood investigation, chest x-ray and ecg was carried out. •Patients were explained in detail about the anesthesia procedure and drug. •All patients were kept nil per oral for 8 hours. All patients were premedicated with Inj. Midazolam 0.03mg/kg, given 5 minutes before procedure to reduce the anxiety. METHODOLOGY They were randomized by computer generated random number sequence into two groups: Group B received 50μg of buprenorphine with 3cc (15mg) of Bupivacaine (heavy). Group F received 25μg of fentanyl with 3cc (15mg) of Bupivacaine (heavy). The drug solution was prepared by an anesthesiologist not involved in the study. On arrival to the operation room (OR), 18G IV cannula was secured and patient was preloaded with 10ml/kg of crystalloid over 15 minutes. Patient monitoring included Non Invasive Blood Pressure (NIBP), pulse oximetry and three lead electrocardiogram (ECG). The baseline systolic and diastolic blood pressures (SBP, DBP), heart rate (HR) and oxygen saturation (SpO2) were recorded. Under strict aseptic precautions subarachnoid block was performed by 25G Quincke spinal needle in the L3-L4 interspace in sitting position. The loaded drug was injected over 10-15 seconds following free flow of Cerebrospinal Fluid (CSF). The time of completion of injection was considered as zero time of the study and all measurements was recorded from this point. Following subarachnoid block, patients was made to lie supine. Hemodynamic variables was recorded at 0 minute 1, 3, 5, 7 and 10 minutes after the administration of subarachnoid block and every 5 minutes thereafter up till 60 minutes of surgery. Hypotension was defined as fall in SBP 30% from baseline and was treated with intravenous fluids and injection Mephentermine in 6mg stat and incremental dose. Bradycardia was defined as HR <50 beats per minute and treated with intravenous atropine 0.6 mg. The incidence of any adverse effects such as hypotension, bradycardia, shivering, nausea, vomiting, pruritus, and respiratory depression and were noted. Post-operatively the hemodynamic variables and oxygen saturation was recorded in the post anaesthesia care unit until complete recovery of the patients from anaesthesia. Duration of analgesia was taken from the time of intrathecal drug administration to the first supplementation of rescue analgesic when patient complained of pain (VAS˃4). Injection Tramadol 1mg/kg intravenous was administered as a rescue analgesic. Total dosage of rescue analgesic agent in 1st 24 hours should be calculated. INTRAOPERATIVE OBSERVATIONS
Sedation score:- Sedation was assessed by Ramsay sedation scale on arrival in OR or, 10 minutes post spinal anesthesia and post operatively. VAS Score-It is a 10 cm long slide ruler with “no pain” written at one end and “Maximum Pain” at the other. VAS more than 4 was considered as cut off for analgesic dose to be given and duration of analgesia was noted. Statistical data:
RESULT Demographic variable and duration of surgery are comparable between both groups (p ˃0.05) in table 1.
Table 1
Onset time of motor and sensory block and duration of motor block was comparable between groups (p ˃0.05) in table 2.
Table 2
Time for Sensory Regression to S2 from highest sensory level, Modified Ramsay Sedation Score and Analgesia duration are more in Buprenorphine than Fentanyl and total dose requirement of rescue analgesia is less in buprenorphine group. (P ˂ 0.05) in table 3 Table 3
Table 4: VAS SCORE VAS score was observed significantly lower in Buprenorphine Group after 210 min of Subarachnoid Block
TABLE 5: side effects In our study, none of the patients had respiratory depression, hypotension and Bradycardia in both study group
DISCUSSION Long bone fractures during trauma can result in significant pain, especially prior to stabilization, due to the significant number of nerve endings located in the periosteum and mineralized bone 20. Meta-analyses suggest that regional anaesthesia, specifically central neuraxial anesthesia, decreases the incidence of deep venous thrombosis (DVT) and pulmonary embolism as well as the incidence of postoperative confusion, in addition to reducing the risk of postoperative pneumonia in patients who require surgical stabilization 21,22,. Since Buprenorphine dissociates slowly from μ-Opioids receptor, it has long duration of action and less addiction potential15, 16, 24.The demographic profile i.e. age, sex, weight, height and Baseline hemodynamic parameters Mean heart rate, Systolic blood pressure, Diastolic blood pressure, Mean arterial pressure in both groups were comparable and was statistically insignificant and similar with other study16,26. ASA status and duration of surgery between two groups of our study was comparable (P > 0.05) and quite similar with other study16, 26 and provided us the uniform platform to evenly compare the results obtained. Time To Reach T-10 Sensory Level (sensory onset time) In our study the mean time to reach sensory level T-10 in fentanyl group was 5.61+0.82 minutes and in Buprenorphine group was 5.80+0.80 minutes. So we can conclude that Buprenorphine needed more time to reach sensory level T-10 as compare to fentanyl but the value was statistically insignificant. Our result are comparable with the study done by kamal sonya(29), safiya I seikh(30) and Aravinder Pal Singh et al (17). Time To Reach Modified Bromage Grade 0 To 3 (motor onset time) In our study the mean time to reach modified bromage grade 3 in fentanyl group was 6.69±0.71 minutes and in Buprenorphine group was 6.90±0.65 minutes. So we can conclude that buprenorphine needed more time to reach modified Bromage score 3 as compare to fentanyl but the value was statistically insignificant. Similar result was found by Fauzia A Khan et al31, Mahima Gupta et al27 ,Poupak Rahimzadeh et al37. Ramsay Sedation Score At The End Of Surgery: In our study the mean sedation score at the end of surgery in Fentanyl was 1.11±0.32 and in Buprenorphine group was 2.02±0.86 which is statistically significant (p value˂0.0001). So we can conclude that intrathecal buprenorphine produce much more sedation than fentanyl. Fentanyl produces sedative effect by acting on synthetic µ receptor. The cause of sedation after intrathecal buprenorphine may be due to its systemic absorption and vascular redistribution to higher centers or cephalad migration in CSF.(16,32).Sedation score increased with higher dose of buprenorphine.15 Total Duration Of Motor Block: In our study duration of motor block in fentanyl group was 175.5±11.39 min and in Buprenorphine group was 176.02±7.19 min which was statistically significant ( p value ˂0.0001). Similar study was done by Jaishri Bogra et al33, Rajni Gupta et al26 , Ayman Eskander T et al25and found similar results. Time For First Rescue Analgesia: In our study the mean time for first rescue analgesia in Fentanyl group was 257.95±10.20 min and in Buprenorphine group was 391.19±14.92 minutes which is statistically significant( p value˂0.0001). Similar studies were done by Safiya et al 32, Rajni Gupta et al26 Soumya Samal et al34, Harbhej Singh et al23, Major Vishal Arora et al28 and found similar results as our study. Buprenorphine has been frequently used in spinal anesthesia to improve the quality of local anaesthetics 35. But, side effect such as hypotension, bradycardia, and sedation is increased as dose of Buprenorphine is increased36.
CONCLUSION Our study has shown that the addition of Buprenorphine with bupivacaine significantly prolongs both sensory and motor block. Both fentanyl and Buprenorphine provided good quality intra operative and post-operative analgesia and hemodynamic stability. The analgesia was clinically better in Buprenorphine group as compared to fentanyl group and it was statistically significant.
REFERENCES
|
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
 Home
Home