Official Journals By StatPerson Publication
|
Table of Content - Volume 12 Issue 2 -November 2019
Efficacy of intrathecal dexmedetomidine for prevention of shivering: A randomized controlled trial
Mimiksha Mahendra Giri1, Siddharthkumar B Parmar2*, Kinjalbahen Nitinkumar Shah3
1Mimiksha Mahendra Giri, 2Siddharthkumar B Parmar, 3Kinjalbahen Nitinkumar Shah, Department of Anaesthesiology, B J Medical College, Ahmedabad. Gujarat, INDIA. Email: drsid25@gmail.com
Abstract Background: Shivering after spinal anaesthesia is common, troublesome and distressing complication undergoing urological surgeries. We aimed to investigate the effects of intrathecal dexmedetomidine to prevent shivering under spinal anaesthesia. Methods: In this prospective, randomised controlled study, total 80 patients planned for elective urological surgeries under spinal anaesthesia were enrolled. Patients were randomly allocated by the use of sealed envelope assignment into two groups: Group D: patients received 2.9 ml of hyperbaric bupivacaine 0.5%, plus 10 mcg Dexmetomidine and Group C- patients received 2.9 ml of hyperbaric bupivacaine 0.5%, plus 0.1 ml Normal saline . The incidence and severity of shivering, peripheral body temperature, hemodynamic parameters, and adverse events was recorded. Results: The incidence of shivering was significantly lower in the group D (22.5%) than the group C (82.5%) (P<0.0001). Likewise, the severity of shivering was significantly lower in the group D than the group C (P<0.05). The incidence of adverse events, such as hypotension, nausea/vomiting, and bradycardia, was not significantly different between the two groups, although the grade of sedation was higher in the group D than the group C (P<0.005). Conclusion: We conclude that intrathecal dexmedetomidine is effective in reducing the incidence and severity of shivering in patients undergoing urological surgeries under spinal anaesthesia without any adverse effects. Key Words: Shivering, spinal anaesthesia, bupivacaine, dexmedetomidine.
INTRODUCTION Spinal anaesthesia (SA) is a safe and widely practiced anesthetic technique for urological surgery. Spinal Anaesthesia affect the thermoregulation system by inhibiting tonic vasoconstriction below the level of anaesthesia through sympathetic and somatic neural blockade 1. Incidence of shivering is about 36–85% after spinal anaesthesia. 2, 3, 4. In urological surgery, shivering also occurs due to irrigation and absorption of large amount of irrigating fluid at room temperature (4, 5). Shivering, increases O2 consumption, CO2production, and catecholamine secretion causes patient discomfort, interruption of monitoring and surgery 6. Many intravenous medications like Meperidine, clonidine and urapidil 7. Magnesium sulfate 8, ketamine, fentanyl and morphine are tried with variable success rates 9. Dexmedetomidine is highly selective Alpha (a)-2-adrenergicreceptor agonist. Only few studies are done to efficacy of intrathecal dexmedetomidine in attenuation and prevention of shivering in urosurgery. 10 So, we aimed to investigate the role of intrathecal dexmedetomidine in attenuation and prevention of shivering in urosurgery under SA in a randomized controlled trial. MATERIALS AND METHODS After local Ethics Committee approval, written, informed consent was obtained from all patients participating in this randomized controlled trial. Eighty patients, aged 20–60 years, ASA physical statuses I, II, and III scheduled for endoscopic urological surgeries under Spinal Anaesthesia, were enrolled in this study. Patients with contraindications to Spinal Anaesthesia, allergy to the study medication, patients receiving vasodilators or medications likely to alter thermoregulation, unstable coronary artery diseases, 2nd and 3rd degree heart block, congestive heart failure, tight mitral or aortic valve stenosis and ventricular tachyarrhythmia were excluded from the study. In the operating room basic monitoring of ECG, oxygen saturation by pulse oximetry and noninvasive blood pressure were applied to all patients and recorded at 5 min intervals using standard monitors. Intravenous line was inserted and intravenous preload with isotonic saline solution was infused to all patients at 15 ml/kg within 30 min. Afterward the rate of isotonic saline solution infusion was set at 10 ml/kg/hr. Patients in both groups were premedicated with 1 mg midazolam intravenously. Core body temperature was recorded of all patients on arrival to the operating room using a thermometer then at 15 min intervals. Operating room (OR) temperature was maintained at 22–24 0C. All patients were covered with one layer of surgical drapes over the chest, thighs, and calves during the operation. Core temperature below 36oC was considered hypothermia. Under aseptic technique, subarachnoid block was performed in sitting position using 23 G spinal needle at either the L3–L4 or L4–L5 intervertebral spaces. Patients were randomly allocated by the use of sealed envelope assignment into two groups: Group D: patients received 2.9 ml of hyperbaric bupivacaine 0.5%, plus 10 mcg Dexmetomidine Group C- patients received 2.9 ml of hyperbaric bupivacaine 0.5%, plus 0.1 ml Normal saline . Supplemental oxygen (4 L/min) was delivered via face mask during surgery time. After injection of local anesthetic, the assessment of sensory block level was done using pin-prick test (needle prick) to be above T10 dermatome. Patients with incomplete or failed Spinal Anesthesia were subsequently excluded from the study. Endoscopic urological surgery was performed using a continuous flow resectoscope with monopolar cautery using 1.5% glycine as an irrigant solution. All intravenous and irrigation fluids were warmed to 370C in warming cabinets. Shivering was assessed by Crossley and Mahajan scale (11) where 0= No shivering, 1= Cyanosis and piloerection, 2 = Visible tremors only in one muscle group, 3 = Visible tremors in more than one muscle group, and 4 = intense shivering, tremors of the head, arm. During surgery, shivering score was assessed and recorded at 15 min intervals. If shivering score was 3, tramadol 1mg/kg IV was administered intravenously. The number of patients treated for shivering with tramadol was recorded. Any adverse effects such as bradycardia, hypotension, nausea and vomiting were recorded. Bradycardia was defined as a decrease in heart rate below 50 beat/min and was treated with IV bolus of atropine 0.5 mg. Hypotension was defined as a decrease in MAP of more than 20% from baseline and was treated with IV boluses of mephentermine 6 mg. The number of patients treated for hypotension with mephentermine was recorded. If patients developed nausea or vomiting, IV bolus of ondansetron 4mg was administered. Total volume of irrigation solution used for each patient was recorded by the end of surgery. Heart rate (HR), mean arterial blood pressure (MAP), oxygen saturation, core body temperature and shivering scores were recorded to all patients at 15 min intervals over one hour postoperatively in PACU. Anesthesia time, surgery time and any adverse events were also recorded. Incidence of post-spinal shivering in previous reports (12) was 55%. With a power of 80% and @ =0.05, minimum 39 patients in each group was required to achieve 40% reduction. We enrolled 40 patients in each group. Qualitative data will be presented as number (percent) and compared by Chi-Square test. Quantitative data will be presented as mean± SD and compared by Student t-test. P <0.05 was considered to be statistically significant.
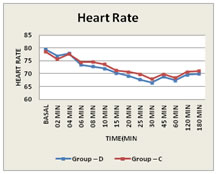
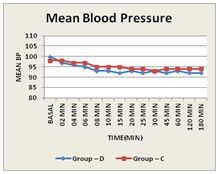
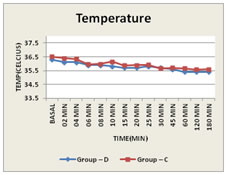
OBSERVATION AND RESULTSThe two groups were comparable regarding age, gender, BMI, anaesthesia and surgery times, and amounts of irrigation fluids. Heart rate, mean blood pressure and temperature were comparable between two groups at different time’s intraoperative (p > 0.05). Based on Crossley and Mahajan scale, the incidence of shivering was significantly reduced in group D compared with group C (p <0.0001) where 9/40 patients (22.5%) in group D developed shivering (five Patients with grade 1 and four patients with grade 2) while 33/40 patients (82.5%) in group C developed shivering (fourteen patients with grade 1, thirteen patients with grade 2 and six Patients with grade 3). No patient in both groups developed grade 4 shivering (Table 2, 3). The incidence of sedation was significantly higher in group D compared with group C (p <0.0001) where 32/40 patients (80%) in group D developed sedation (twenty four patients with grade 1 and eight patients with grade 2) while 8/40 patients (20%) in group C developed sedation (eight patients with grade 1). No patient in both groups developed grade 3 sedation (Table 4). The frequency of bradycardia (6 patients vs. one patient), hypotension (8 patients vs. 2 patients), Were significantly higher in group D compared with group C but statically not significant (P = 0.1084, P = 0.0872) respectively (Table 5). There was no significant difference in the incidence of nausea in both groups (p=0.4937). No patient in both groups had respiratory depression or needed GA due to failed SA. Table 1: Demographic data
Figure 1: Heart rate wise distribution Figure 2: mean blood pressure wise distribution Figure 3: temperature wise distribution
Table 2: Incidence of shivering
Table 3: Shivering score wise distribution
Table 4: Sedation score wise distribution
Table 5: Intraoperative parameters
DISCUSSIONShivering is just a protective mechanism to preserve body heat (13). The exact mechanism of shivering during SA is not clear but possibility includes cessation of central thermoregulation, internal redistribution of body heat and heat loss to the environment. 10 Dexmedetomidine is highly selective alpha 2 adrenergic receptors agonist. It is basically sedative, analgesic, sympatholytic drug having anesthetic-sparing, and hemodynamic stabilizing properties 14. Addition of intrathecal dexmedetomidine to heavy bupivacaine 0.5% was more advantageous than fentanyl with special regard to its analgesic properties in diabetic surgical patients 14, 15. Premedication with IM dexmedetomidine decreases the incidence of postoperative shivering 16. It is highly lipophilic, which facilitate its rapid absorption into the cerebrospinal fluid and binding to the spinal cord α 2 adrenoceptors(17). Improvement in quality of spinal anesthesia is reported by the addition of Dexmedetomidine (14) with less hypotensive effect and an added sedative effect without respiratory depression (10). Dexmedetomidine leads to Activation of a 2 adrenergic receptors in the brain and spinal cord and decreases sympathetic tone and attenuates the neuroendocrine and hemodynamic responses to anesthesia and surgery. In the current study, we choose urosurgery patients because shivering is more common due to irrigation fluids. The incidence of shivering was reduced in group D Compared with group C. 9 patients(22.5%) develop shivering in group Dexmedetomidine compared to 33 patients(82.5%) develop shivering in group Control. No shivering was seen in 31 patients of group D while 7 patients develop shivering in group C. Grade 1 shivering was seen in 5 patients and 14 patients in Group D and Group C respectively. So there was significant difference in two groups. (p<0.0356). Grade 2 shivering was seen in 4 patients and 6 patients in group D and group C respectively. So there was significant difference between two groups (p<0.0288). Grade 3 shivering was seen in 0 patients and 6 patients in group D and Group C respectively. So there was significant difference between two groups. (p<0.0335). No patient develop grade 4 shivering. Usta et al10 conducted a prospective controlled study to evaluate the effect of dexmedetomidine on shivering during SA upon 60 patients undergoing minor surgical operations, reported result, 3/30 (20%) in dexmedetomidine infusion group and 17/30 (56%) in the control group developed shivering (p= 0.001) (13). Coskuner et al 18 conducted a study upon 60 patients for lower abdominal surgeries to examine the effects of intravenous dexmedetomidine in epidural anesthesia, reported similar results to us of significant decrease in shivered patients in dexmedetomidine group, with a significant increase in patients experiencing bradycardia that was safely treated with atropine. Bicer and colleagues (19) conducted a placebo controlled study for the efficacy of dexmedetomidine compared with meperidine and placebo in preventing postanesthesia shivering after elective abdominal or orthopedic surgery. They concluded that, 22 patients (55%) in the placebo group, four patients (10%) in the Meperidine group and six patients (15%) in the dexmedetomidine group developed shivering. They concluded that intraoperative dexmedetomidine 1 mcg/kg administered intravenously reduces post anesthesia shivering similar to Meperidine 0.5 mg/kg in patients. Elvan and colleagues (20) in a prospective controlled study upon 90 patients evaluated the effect of dexmedetomidine on postoperative shivering in patients undergoing elective abdominal hysterectomy. They reported a similar results, 7/45 (15%) in dexmedetomidine group and 21/45 (46%) in saline group developed shivering (P =0.001). The incidence of bradycardia that safely treated with atropine was higher in dexmedetomidine group. In agreement with our results, Abdel Hamid et al21 conducted a randomized controlled trial upon 62 patients to evaluate the role of dexmedetomidine 5 mcg added to heavy bupivacaine 0.5% intrathecally for lower abdominal surgeries, reported lower incidence of shivering in dexmedetomidine group (2/31) compared with (12/31) in control group. Bradycardia was observed more (8/31) among patients in dexmedetomidine group while no patient in control group experienced bradycardia. In the current study, HR and MAP were nearly same after SA and there was not statically significant difference between two groups. The incidence of nausea, vomiting was insignificant between both groups in accordance with other reports 8, 10, and 13. In this study, no patients in both groups had respiratory depression or needed GA due to failed SA.
Limitation of this study 1. We did not assess different doses of dexmedetomidine; further studies are needed to evaluate the effects of dexmedetomidine with various doses. 2. We could not measure core body temperature. 3. We did not assessed incidence of shivering in post-operative period.
CONCLUSION We conclude that the use of 10 mcg intrathecal dexmedetomidine in patients undergoing urosurgery has a noticeable control of shivering with no significant side effects.
REFERENCES
|
|
 Home
Home