|
Table of Content - Volume 13 Issue 1 -January 2020
P Sridhar1*, Sabapathy2, R Shankar3
1Associate Professor, Department of Anesthesiology, Danalakshmi Srinivasan Medical College and Hospitals, Perambalur - 621113 {2Professor, Department of Anesthesiology} {3Professor, Department of Preventive Medicine} Vinayaka Missions Kirupananda Variyar Medical College and Hospital, VMRF (DU), Salem. Email: drsridhar1502@gmail.com
Abstract Background: Recently introduced levobupivacaine and ropivacaine were considered as long-acting local anesthetic drugs that are commonly used for peripheral nerve blocks that is believed to provide prolonged postoperative analgesia. Addition of fentanyl to either of these two local anaesthetic drugs improves the quality of intraoperative and early postoperative subarachnoid block and also helps in prolonging the duration of analgesia. Aim: To compare the effectiveness of post-operative analgesia, hemodynamic changes, side effects and residual motor blockade effects between 0.125% of levobupivacaine and 0.125% of ropivacaine along with 1µg/ml of fentanyl. Methodology: A prospective longitudinal study was conducted for a period of one year in the department of anaesthesiology at Dhanalakshmi Srinivasan Medical College and Hospital. Patients in the age group between 18 and 60 years with a ASA grade of either I or II and were undergoing either elective or emergency abdominal surgeries were taken as our study subjects. . A total of 120 patients were taken as our study subjects and those 120 were divided into 4 groups of 30 each of which two groups received either ropivacaine or levobupivacaine and the other two groups received fentanyl along with the above two drugs. All patients received 5 ml of the study drug and then it was followed by an infusion of 8 ml/hr with top ups of 5 ml as required for break through pain. Pain assessment was done using the VAS scoring scale. Results: VAS pain score was significantly lesser among the patients who received ropivacaine or levobupivacaine along with fentanyl compared to the patients received the local anaesthetic agents without fentanyl and no significant difference in pain perception was seen between the ropivacaine and levobupivacaine group. The hemodynamic parameters and the incidence of side effects did not show a statistical significant difference between the four groups. Conclusion: Levobupivacaine with fentanyl and ropivacaine with fentanyl were almost of equianalgesic efficacy based on the VAS scoring both at rest and during movements and also their hemodynamic properties seems to be of same nature. Key Words: Levobupivacaine, ropivacaine, fentanyl, analgesic effect
INTRODUCTION Postoperative pain after any surgical procedure produces a range of detrimental acute and chronic effects on the patients. So to control and prevent this pain among the patients undergoing abdominal surgeries epidural analgesia was found to be a most effective and acceptable mode of pain relief technique. As this technique makes the patient get mobilized early in the post-operative period and the recovery may be fastened. Epidural analgesia being delivered through indwelling catheter is found to be safe and effective method of post-operative pain management and thereby improves the quality of life which is said to be the ultimate goal of anesthesiology. Epidural infusion of analgesia is given along with anaesthetic agents in the epidural space which includes spinal nerve roots, dorsal root ganglion or the spinal cord itself.1-3 Recently introduced levobupivacaine and ropivacaine were considered as long-acting local anesthetic drugs that are commonly used for peripheral nerve blocks that is believed to provide prolonged postoperative analgesia. Levobupivacaine was introduced more recently in India in 2012.4 It is a pure S-enantiomer of Bupivacaine and it is more lipophilic compared to ropivacaine. The use of ropivacaine in India was started in 2009, which is a monohydrate of hydrochloride salt of 1-propyl 2,6-pipecoloxylidide and it is prepared as pure s-enantiomer. Based on the pharmaco-dynamic and kinetic properties levobupivacaine was found to be more potent than rupivacaine in regard of providing effective post-operative analgesia.5 The reduced cardio-toxicity of levobupivacaine such as increase in PR and QT interval and negative ionotropic effect as reported for bupivacaine provides a wider safety margin for the use in routine clinical practice both as single shot and as a continuous infusion during the intra-operative or post-operative period for effective pain management.6,7 Though literature had shown that levobupivacaine is more potent in controlling the post-operative pain compared to ropivacaine based on their pharmacological properties but previous reports have not shown a longer duration of postoperative analgesia when levobupivacaine is used for brachial plexus blocks compared with ropivacaine, except in a single report which had showed levobupivcaine is more superior than ropivacaine for pain relief in the post-operative period.8,9 Of late fentanyl was considered to be a most preferred opiod than morphine because of its lesser side effects over cardiovascular system and more hemodynamic stability and the respiratory depression is minimum compared to morphine. The addition of fentanyl to hyperbaric bupivacaine improves the quality of intraoperative and early postoperative subarachnoid block and also helps in prolonging the duration of analgesia.10 As of today not much studies had been conducted comparing the analgesic property between ropivacaine and levobupivacaine with addition of fentanyl and so the present study was undertaken to compare the efficacy between these two drugs in providing post-operative analgesia.
AIM To compare the effectiveness of post-operative analgesia, hemodynamic changes, side effects and residual motor blockade effects between 0.125% of levobupivacaine and 0.125% of ropivacaine along with 1µg/ml of fentanyl. METHODOLOGY A prospective longitudinal study was conducted for a period of one year in the department of anaesthesiology at Dhanalakshmi Srinivasan Medical College and Hospital. The study was started after getting the clearance from the institutional ethical committee and the informed consent was obtained from all the study participants. Patients in the age group between 18 and 60 years with a ASA grade of either I or II and were undergoing either elective or emergency abdominal surgeries such as appendicectomy, hernia repair, colostomy or ileostomy closure were included in our study. Patients with ASA grade 3 or 4 and with contraindications for spinal anaesthesia were excluded from the study. A total of 120 patients were taken as our study subjects and those 120 were divided into 4 groups of 30 each. Group I patients received 0.125% of ropivacaine infusion for 24 hours at the rate of 8 ml/hr epidurally Group II patients received 0.125% ropivacaine with fentanyl 1 microgram per ml at the rate of 8 ml per hour for 24 hours epidurally. Group III patients received 0.125% of levobupivacaine infusion for 24 hours at the rate of 8 ml/hr epidurally Group IV patients received 0.125% levobupivacaine with fentanyl 1 microgram per ml at the rate of 8 ml per hour for 24 hours epidurally. Pre-anesthetic work up was done on all patients with routine blood and urine examination along with ECG and X-ray chest. The procedure of epidural block was explained to the patients in the beginning about the position, the technique and the parameters to be observed. Intradermal sensitivity test was performed on all patients and patients with normal response alone are taken for the study. Pre-operative medication such as 0.5 mg of alprazolam along with 40 mg of pantoprazole was given for all the patients. Under strict aseptic conditions spinal anesthesia was administered in the space between L1 and L4 to achieve the subarchnoid block by injecting 3 cc of 0.5% hyperbaric bupivacaine hydrochloride and the patients vitals were monitored throughout the procedure. Post-operatively patients vitals were recorded and monitored continuously along with the pain score using the visual analog scale. Epidural infusion of drugs was given in the post-operative period based on the respective groups, initially all patients received 5 ml of the study drug and then it was followed by an infusion of 8 ml/hr with top ups of 5 ml as required for break through pain. VAS score for rest and movement were recorded at initiation of infusion, 1 hour, 3 hours, 6 hours, 12 hours, 18 hours and 24 hours. All data were entered and analysed using SPSS version 22, mean and standard deviation was calculated for all the parametric variables and percentage was derived for all the frequency variables. Chi-square test and ANOVA were used for deriving the statistical inference considering p<.05 as statistically significant.
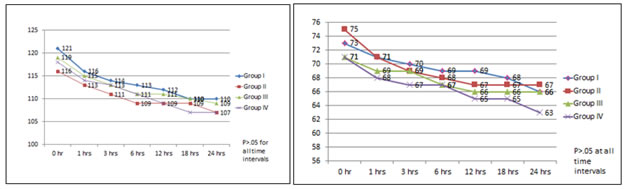
RESULTS The age and gender distribution of the study subjects shows that majority of them were in the age group between 35 and 40 years and most of them were males among all the four study groups and there was no statistical significant difference between the four groups with respect to age and gender distribution (table 1). Post-operative pain assessment at rest was done based on the VAS scoring system and the comparison of pain score between the four groups at various time intervals from one hr to 24 hrs. It showed a statistical significant difference (p<.05) in the pain score when the comparison was done by taking all the four groups but when the intergroup comparison was made between two groups the significant difference was seen only between group I and II and between group I and IV (table 2). Similar type of results was seen when the VAS score comparison was done during movement with the inter group comparison between two groups showed statistical significant difference between the groups I and II, I and IV and group III and IV (table 3). The hemodynamic parameters such as heart rate, systolic and diastolic blood pressure were measured in all the 4 groups at regular time intervals and it showed that no statistical significant difference was seen with respect to HR, SBP and DBP among the four groups as well as comparing between two groups (table 4, fig 1 and fig 2). The total amount of the local anesthetic drug used and the number of bolus doses used among the study subjects was found to be more among group I and then followed by group III, whereas the doses used among group II and IV was considerably lower because of usage of fentayl in these two groups. So it is proven that the group which received ropivacaine had showed increased amount of requirement of the dosage compared to the group which received levobupivacaine and the difference was found to be statistically significant (p<.05) (table 5). The incidence of the adverse events such as nausea, vomiting, urinary retention and hypotension were found to be very minimal among the study subjects in all the 4 groups and no statistical significant difference was seen between the groups (table 6). Table 1: Age and gender wise distribution of the study subjects
P value derived for inter-group comparison
Table 2: Comparison of VAS score at rest between the study groups
Table 3: Comparison of VAS score during movement between the study groups
Table 4: Comparison of the heart rate at various time intervals among the study groups
Figure 1 Figure 2 Figure 1: Line diagram showing the mean systolic BP at various time intervals among the study groups; Figure 2: Line diagram showing the mean systolic BP at various time intervals among the study groups
Table 5: Total amount of local anesthetic drug administered among the study groups
Table 6: Distribution of the adverse events reported among the study groups
DISCUSSION Adequate post-operative pain management especially after any abdominal surgeries has become a most challenging issue now days. Epidural analgesia with local anesthetics is considered as the most effective technique used for pain management which would further improve the patient outcome and the quality of life. Way back in 1931 the first study was conducted on continuous epidural infusion being used for pain management particularly among patients with severe trauma. Further addition of opioid to the epidural local anesthesia improves post-operative analgesia and decreases systemic response to trauma according to the study conducted by Zwarts SJ.11 Another study done by VirendraKumar on the effect of butorphanol as a continuous analgesic drug after thoracic surgery had showed a promising result in pain relief.12 A metaanalysis study done by Chistropher L. WU et al on comparison between epidural analgesia and intravenous analgesia with opioids and concluded that patients who received epidural analgesia had a better pain relief compared to the patients received intravenous opioids and it also showed that there is a higher incidence of adverse events such as nausea, vomiting and motor block among the patients received epidural analgesia.13 Local anaethetic drugs given via epidural route blocks the nociceptive input into the central nervous system thereby were providing a greater analgesic effect. Although studies were being showing that epidural local anesthetics with opioids provides superior analgesia, not much studies had been conducted with the usage of ropivacaine either alone or in combination of opioid agents like fentanyl as an epidural local anesthetic. The major advantage of combining opioid with local anesthesia is it gives superior analgesia without causing motor or sympathetic blockade. The primary mechanism of fentayl producing analgesic effect after epidural route of administration is through systemic. So the ultimate objective of administering opioids along with anesthetic agents for pain management is for 3 important reasons; 1. The dosage of both the drugs can be reduced 2. enhancement in the degree of pain relief 3. reduction in the incidence of adverse events.14-16 So the present compared the effect of local anesthetic with and without opioid in the post-operative pain management. Ropivacaine is a recently introduced epidural anesthetic drug used for pain relief and it was shown to be superior than bupivacaine because of its reduced tendency in causing motor block such a way making it less toxic. The optimal concentration of ropivacaine when used alone is 2% for getting an effective analgesic effect but even sometimes it was shown that this concentration was not sufficient enough to produce analgesic effect and it might also lead on to motor blockade. So combining an opioid analgesic like fentanyl along with this drug shows a superior pain management even with 0.1% of ropivacaine when fentayl was used in the dosage of 1 – 5 µg/ml. A study conducted by R Whiteside et al on pain management for patients who had undergone gynecological oncology procedures found that 0.1% ropivacaine with 1 µg/ml of fentanyl showed a satisfactory result in pain management when compared to 0.2% ropivacaine with 2 µg/ml of fentayl and so based on the above results in our study we had chosen the concentration of ropivacaine as 0.1%.17 Levobupivacaine the racemic mixture of bupivacaine has the benefit of reduced cardiac and CNS toxicity compared to bupivacaine and studies had shown it produces excellent analgesic and anesthetic effect in the routine clinical practice. A study by Senard M et al showed that levobupivacaine when used with or without opioid analgesic had showed an adequate post-operative analgesic effect among patients who had undergone major abdominal surgeries and this results were almost in par with our study which showed the VAS score did not showed a significant difference between group III and IV at rest but a significant difference was observed between these two groups during movement.18 Whereas the VAS score both at rest and movement was found to be higher in the group which received ropivacaine alone compared to the group which received fentayl along with ropivacaine and the difference was found to be statistically significant and this result was almost in par with the study done by Wai-Keung Lee et al.19 Contradicting to the results of the present study, a study done by Berti et al had found no statistical significant difference in pain relief among the group received 0.2% ropivacaine alone and with fentayl.20 Another study done by Casati et al comparing 0.2% ropivacaine with 0.125% of levobupivacaine for postoperative pain management after major orthopedic surgery had found that the quality of analgesia was similar in both the groups but in our study we used 0.1% ropivacaine.21 Few other studies done by Etches etal, Capogna and Camorica et al had showed that the analgesic potency of ropivacaine is upto 20% lesser than levobupivacaine, whereas our study shows that the analgesic property between these two drugs at a concentration of 0.125% is equivocal only the difference is seen when fentanyl is added along with it.22,23 A study done by Paraskevi et al, Pasquale De Negri et al had shown that the analgesic property of 0.125% levobupicaine and ropivacaine when used alone or with fentanyl was found to be similar but in our study there was a statistical significant difference observed in VAS score when fentayl is added along with ropivacaine.24,25 A study done by Shin-Yan Chen et al compared with 0.1% and 0.6% bupivacaine with and without fentanyl and found that the resting and dynamic VAS score did not show statistical significant difference between the groups but in our study the dynamic VAS score was significantly lesser in the group that received fentanyl along with the local anesthetic and a similar finding was reported by the study done by Smet etal.26,27 In the current study the hemodynamic parameters such as heart rate, systolic and diastolic blood pressure did not show any significant difference between the four groups at various time intervals and a similar type of results was also reflected in the studies done by Paraskevi et al and Smet et al.24,27 In the present study adverse events such as nausea, vomiting, hypotension and urinary retention were reported only in one or two patients in all the 4 groups and no significant difference was observed between the groups and a similar type of results was shown in the study done by Karis Bin Misiran et al, Smet et al, Lyon et al and Paraskevi et al.24,27-29
CONCLUSION From the results of the present study it is concluded that levobupivacaine with fentanyl and ropivacaine with fentanyl were almost of equianalgesic efficacy based on the VAS scoring both at rest and during movements and also their hemodynamic properties seems to be of same nature. Adverse events reported were very minimal in both these groups, whereas a gross difference was found in the analgesic property when levobupicaine and ropivacaine were used without fentanyl. So it is always a better option to add fentanyl along with either levobupicaine or ropivacaine for achieving a better pain control during the post-operative period.
REFERENCES
Policy for Articles with Open Access |
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
 Home
Home