|
Table of Content - Volume 13 Issue 3 -March 2020
Upasana Gupta1, Vasudha Jadhav2*
1Junior Resident, 2Professor, Department of Anaesthesiology, Bharti Vidyapeeth University Medical College and Hospital, Sangli, Maharashtra, INDIA.
Abstract Background: Introduction: Conventional laryngoscopes (Macintosh) are most used laryngoscope for endotracheal intubation for routine surgical patients. Difficulty with endotracheal intubation by DL is primarily a function of an inadequate view of the glottis. The TrueView EVO2 laryngoscope is a device with a blade that provides an optical view of the glottis It has a modified laryngoscope blade, which can be attached to the digital camera. It also has an unmagnified optic side port with anterior fraction of 42° in the line of sight allowing indirect tracheal intubation. Aim and Objectives: To compare TrueView evo2 video laryngoscopy with conventional laryngoscopy(Macintosh) in patients with anticipated difficult airway with respect to the view of the glottis by (Cormack–Lehane grading); Time for tracheal Intubation, Attempts required for intubation, manoeuvres to optimize the laryngeal view and success rate of intubation. Materials and Methods: A total of 60 patients ASA Grade-I – III MPG II-III, scheduled for surgery under general anesthesia were divided into two groups. Group VL- 30 Patients (TrueView evo2) and Group ML (Macintosh) Result: The demographic data and ASA status were comparable in both the groups. The TrueView evo2 laryngoscope provided a better glottic view than the conventional Macintosh blade as per Cormack lehane grading but required a longer intubation time than Macintosh laryngoscope (35 vs 20.1 s). Number of attempts were reduced with TrueView evo2, with increased number of successful intubations. Rescue manoeuvre were required more with conventional laryngoscopy. Conclusion: TrueView evo2 video laryngoscope improves the glottic view in patients with anticipated difficult airway at the cost of increased intubation time. With increased experience, the time for intubation might be reduced. Key Words: difficult intubation, intubation time, laryngoscopy, macintosh, TrueView eVo2 video-laryngoscopy
INTRODUCTION Airway management is of the major concern in the routine surgeries under general anesthesia. It is one of the prime importance for an anesthesiologist.1 Predictors for difficult laryngoscopy – Long upper incisors, Inability to protrude mandible, Mallampati classification III or IV, High arched palate, Short thyromental distance, Short thick neck, Limited cervical mobility. Cormack and Lehane developed a grading scale in 1984 to describe laryngoscopic views 2. The grades range from I to IV, beginning with grade I (the best view), in which the epiglottis and vocal cords are in complete view, and culminating with grade IV (the most difficult view), in which the epiglottis or larynx is not visualized. A modified classification scheme with five different grades based on the Cormack-Lehane scoring system is described by Yentis, who proposed that grade II be differentiated into IIA (partial view of the glottis) and IIB (arytenoids or posterior vocal cords only are visible).Intubation is rarely difficult when a grade I or IIA view is achieved; grades IIB and III are associated. In such patients, it is a challenging task to secure the airway. Macintosh blade, which is most used in day to day practice, frequently fails to help in intubation with direct laryngoscopy 3,4. Failures during intubation during emergency or unanticipated situation has almost accounted for 1.5-8.5%. 5 In difficult situation, many rescue maneuvers are employed which includes techniques like use of bougie, BURP maneuver etc. though, even these techniques are not fully effective in difficult scenarios and sometimes leads to failed intubation even after using all the techniques available. To overcome these technical difficulties, various video laryngoscopes has been brought into practice. One of which includes TrueView EVO2 laryngoscope (TL). TrueView EVO2 laryngoscope (Truphatek International®, Netanya, Israel) is a video-laryngoscope, with a unique blade that provides an optical view around the corner [Figure 1] with least manipulation of the head, neck, instrument or soft tissues.6. It facilitates a better view of an anteriorly placed larynx, using the optical principle of refraction of light. It has a modified laryngoscope blade which incorporates an unmagnified optic side port with anterior refraction of 35° in the line of sight allowing indirect tracheal intubation. 7,8 the laryngoscope is molded in such a manner that the glottis lying at the tip of the blade is best seen without any manipulation or tilt of the head, neck, instrument, or soft tissues. This improves the laryngeal view by more than 1 grade. Various studies have shown TrueView EVO2 laryngoscope to be associated with a better glottis view, expressed by the Cormack–Lehane Grade 8 ,14, reduced intubation time, and higher success rates as compared to the conventional laryngoscopy. Singh et al.7 showed that the Truview EVO2(C) improves Cormack and Lehane grading by one or more grades without much difference in time required for negotiation of the endotracheal tube when compared with ML in patients with anticipated difficult airway. AIMS and OBJECTIVE Considering various studies done previously, the current study was planned to access whether TL can be routinely used for intubation in patients with predicted difficult airway. We compared the efficacy of TL against the convention Macintosh laryngoscope (ML) in patients posted for surgery under general anesthesia with anticipated difficult airway characteristic. Our objective included to compare the:
MATERIALS and METHODS After obtaining approval from Institutional Ethical Committee, written informed consents were taken from all patients before entry into the study. This study was conducted on 60 adult patients from both genders, American Society of Anaesthesiologist (ASA) physical status I–III, scheduled for elective and emergency upper limb, lower limb, abdominal and neurosurgery under general anaesthesia during the period from August to December 2019. We excluded the patients below18 yrs., ASA grade IV and above, patients undergoing rapid sequence intubation, patients with mouth opening less than 2 cm, patients with difficult mask ventilation and at risk for aspiration and patients who were not willing to consent for the study. After the detailed preanesthetic evaluation, including history, general, and systemic examination, thorough airway assessment, and appropriate laboratory tests was carried out in each patient. Airway assessment was done. Mouth opening, condition of teeth, temporomandibular joint mobility, neck movement, modified Mallampati grading (MPG), and atlantooccipital extension was noted. Patients were explained the risks involved and an informed written consent was taken. Patients were sequentially numbered in sealed, opaque envelopes. They were randomized into 2 groups, each of 30 patients by lottery method. On arrival of the patient to the operating theatre, all standard monitors were applied including heart rate (HR), electrocardiogram (ECG), oxygen saturation (Spo2), end-tidal CO2, arterial blood pressure (systolic (SBP), diastolic (DBP) and mean (MAP) and temperature. The difficult intubation tray was kept ready and easily accessible. Premedication was done with i.v. ondansetron 4mg and i.v. glycopyrrolate 0.2 mg and inj. Midazolam 4 mg i.v. Patients were preoxygenated with 100% oxygen on mask for 3 min and were given inj fentanyl 60 mcg i.v. Induction was done with i.v. propofol 2 mg/kg and ventilation with bag and mask was checked and confirmed. Difficult mask ventilation or the patients who were unable to be ventilated were excluded from the study. Muscle relaxation was achieved with depolarising muscle relaxant i.v. succinylcholine 2 mg/kg. In Group VL, patients head was kept in in neutral position and intubation was done with Video laryngoscope (TrueVieweVO2), whereas the patients in Group ML were placed in sniffing position with their head on ring and intubated with blade of size 3 or 4 of the standard Macintosh laryngoscope. On visualization of cords, Cormack–Lehane grade was noted. Endotracheal intubations were performed using Portex cuffed Endotracheal Tube. Preformed “J” ‑shape stylet was used over the endotracheal tubes. BURP or bougie was used whenever it was necessary, to facilitate intubation. After successful intubation, the patients were mechanically ventilated and anesthesia was maintained with sevoflurane in a mixture of nitrous oxide and oxygen in a 1:1 ratio. Maintenance of muscle relaxation was done with inj Vecuronium (0.1mg/kg), monitored by ‘TOF’ for every 30 minutes and incremental dose adjusted to maintain 1–2 responses to ‘TOF’ stimulation. Lungs were mechanically ventilated to maintain normocapnia (Etco2 35–40 mmHg). Intubations in both the groups were performed by the same anaesthesiologist, experienced with both the techniques in managing difficult airways. The time taken for intubation was measured from the time of insertion of the laryngoscope into the patient’s mouth till the inflation of the cuff of the endotracheal tube. The number of attempts needed by anaesthesiologist were also recorded. The incidence of mucosal trauma and dental injury was noted in both the groups. The heart rate (HR), ECG, oxygen saturation (SpO2), and mean arterial pressure (MAP) were recorded at the baseline, post induction, just after tracheal intubation and at 1, 3, and 5 min post intubation. Any episode of hypotension (MAP <20% of baseline), bradycardia (HR <50 bpm), hypertension (MAP > 20% of baseline), hypoxemia (SpO2 <90%) and cardiac arrhythmia were noted. If more than one attempt was required for intubation, the patient was ventilated with bag and mask and then fresh attempt was made. Failure to intubate was considered after three failed attempts and alternative techniques were used to maintain airway. An independent observer was assigned the job to note the data. All the observations done in the study was subjected to statistical analysis. Hemodynamic parameters: HR, BP, SpO2 Time taken for intubation. No of attempts for intubation CL grading Rescue maneuver required Success rate Post intubation trauma
STATSTICAL ANALYSIS To detect at least 20% difference in means of hemodynamic variables in the patients at different time points during surgeries under general anaesthesia, with a power of 95% and alpha error over 0.05, 27 patients were required. We have included 30 patients in each group to compensate for possible dropouts from the study. Data was collected and tabulated in excel sheet. Data was compared and analysed statistically for the significance of observed differences if any. P values < 0.05 were considered significant and <0.01 was considered highly significant. The results were expressed as Mean ± Standard Deviation (S.D.). Unpaired t-test was used for inter-group comparison. Hemodynamic parameters and numerical data were compared within the group against baseline values using paired t-test. Statistical package for social sciences (SPSS) version 22 for windows was used for statistical analysis and to draw conclusions.
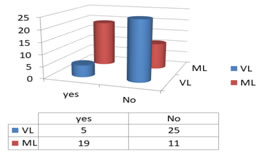
RESULTS Demographic and airway assessment data of the patients are shown in Table 1. The two groups were comparable in terms of age, sex, weight and height. There was an even distribution of airway assessment parameters among the two groups. Both the groups had similar patient distribution with respect to difficulty level. In Group VL, 6.6% patients had difficult in neck extension, while 13.3% in group ML. 8 out of 30 patients showed MPG III in Group VL against 10 out of 30 in Group ML.26 % in group VL had short thyromental distance while 23% had short thyromental distance in group ML [Table 2]. Cormack–Lehane Grade I was seen in 33.3% and 20% in Group VL and Group ML respectively, Cormack–Lehane Grade II was seen in 43.3% and 36.67% patients in Group VL and Group ML, respectively, Cormack–Lehane Grade III was seen in 20% and 36.7% patients in Group VL and Group ML respectively, while CL grade IV was seen in 3% and 6% in group VL and ML respectively. These values were statistically significant and there was a significant difference in the median Cormack–Lehane grading. The view of the glottis improved by one Cormack–Lehane grade in patients with MPG IV and by two grades in patients with MPG III, limited neck extension and history of difficult intubation. Thus, TrueView EVO2 improved the view of the glottis by two grades as compared with Macintosh blade the median Cormack–Lehane Grade was II in Group VL as compared with Grade III in Group ML[FIG2]. Hence, by using Mann–Whitney U test P < 0.05 therefore there is significant difference between median Cormack–Lehane grade in GroupVL and Group ML. TTI in Group VL was 30.5±5.09 while the TTI in group ML was 23.0±7.9[Table 3] [fig1] This difference was statistically significant, P value was < 0.05. More than one attempt was needed in 20% of the cases in group ML while only 3% in group VL and it was statistically significant. Thus, with TrueView EVO2 blade a smaller number of attempts were required for intubation as compared with those using Macintosh blade. In Group VL, only 16.6% of the patients required rescue manoeuvre to facilitate intubation, whereas 83.4% of the patients did not require any optimizing manoeuvre. In Group ML, 63.3% of the patients required optimising manever. These findings were statistically significant. Thus, the number of optimizing manoeuvres required to facilitate intubation is significantly less with TrueView EVO2 blade as compared with those using a Macintosh blade [FIG3]. Success rate were equal in both the groups and values were not significant. Thus, both the techniques were comparable to each other in terms of success rate of intubation. Incidence of trauma was seen in 10% in group VL while 33.3% in group ML. Rescue techniques was used more frequently in group ML than group VL[FIG4]. Hemodynamic variables were comparable in both groups and were not significant. TABLE 1: DEMOGRAPHIC DETAILS
TABLE 2: DISTRIBUTION OF AIRWAY DIFFICULTIES
TABLE 3: TIME TAKEN FOR INTUBATION
FIGURE 4: RESCUE TECHNIQUES USED
DISCUSSION Routinely used Macintosh blade for direct laryngoscopy is the conventional method for intubation. In patients with difficult airway, conventional methods sometimes lead to failed intubation 14. Frequent manipulation of the airway to secure the endotracheal tube may sometimes lead to airway trauma or mucosal injuries. In such scenarios, video laryngoscope like TrueView eVo2 proved to a better option. This study was designed to evaluate the efficacy of Video laryngoscope in routine scenarios with difficult intubation. The videoaryngoscope TruView EVO2 has been used in various studies done previously. It provides a better laryngeal view using its optical system. It provides a 42° deflection view through a 15‑mm eyepiece. It applies the optical principle of light refraction to provide a more anterior view of the larynx. Thereby, providing a better view in a greater proportion of patients and thus allowing intubation to be performed under direct vision more frequently than is possible with a conventional laryngoscope. It has a continuous O2 flow system which delivers 4-5 l/min which can be attached to the laryngoscope, thereby reduces lens blurring. There are various studies reported for the successful use of TrueView EVO2 for endotracheal intubation in patients with normal airway as well as suspected difficult airways. In our study, TrueView EVO2 and Macintosh blade laryngoscopes were compared by noting the Cormack–Lehane grades during laryngoscopy. In our study we observed that , TTI in TrueView group was 30.5±5.09 and the TTI in Macintosh group was 23.0±7.9 sec, the longer time taken for intubation in TrueView group might be attributed to the technical skills required to operate the TrueView laryngoscope, associated with hand eye coordination and viewing through the lens or in camera. We also observed that with increasing expertise, the TTI reduced. Ramesh et al. (2011) 9 published that the time taken for intubation (TTI) was 23.11 s in the Macintosh Group and 33.62 s in the TrueView Group. He stated that intubation is performed in an indirect manner with TrueView that is seeing the tube and the cords through the lens, and focuses on the cords, then the endotracheal tube is passed blindly till the tip enters the TrueView visual field. It requires a requires good hand– eye coordination and expertise. The anesthetists who are new to this technique, experience considerable difficulty in advancing the tracheal tube toward the view of the lens; this may be the reason for increased TTI with TrueView. Torun et al. (2011) 15 reported that the time for intubation in Macintosh Group was 23 s and in TrueView Group it was 42 s, which was statistically significant. Singh et al. (2011) 16 observed that in their study, the mean TTI in TrueView Group was 28.6 s. The average time taken for negotiation of ETT was much less than that reported by other authors. 9,15 On comparing the Cormack-Lehane grades using the TruView EVO2 and Macintosh blade, we observed that the median Cormack– Lehane grade I in Group VL was 43.3% and grade II in 36% whereas CL grade I was seen in only 20% in Group M and median CL grade was II. It was statistically significant and showed that TrueView EVO2 improved the glottic view by at least one Cormack–Lehane grades as compared with Macintosh blade. Similar studies done by Barak et al. (2007)17 showed that the TruView blade provided a better laryngoscopic view than the Macintosh blade, that is, in 100% patients with anticipated difficult intubation in TrueView Group the Cormack–Lehane grade was I, whereas in Macintosh Group only 14.2% of the patients had Cormack–Lehane grade I and 28.5% and 57.14% of the patients had Cormack–Lehane grades II and III, respectively. Timanayakar et al. (2011) 18 found that in patients with MPG III TrueView provided Cormack–Lehane Grade I in 68.48% cases, whereas Macintosh blade provided grade I in 22.22% of the cases. In patients with MPG IV no patients had Cormack–Lehane grade III/IV in TrueView Group while 50% patients in Macintosh Group had Cormack–Lehane III/IV. Li et al. (2007) 19 also observed that MPG determined prior to laryngoscopy was significantly related to the view of the glottis for both the Groups. Tutuncu et al. (2009) [20] found that only 3.3% of the patients in TrueView Group had Cormack–Lehane Grade III, whereas 33.3% of the patients in Macintosh Group had Cormack–Lehane Grade III. Singh et al... (2007) 4 stated that 93.75% of the patients showed improvement in glottic view by one Cormack–Lehane grade, whereas 76.47% of the patients showed improvement by two. In our study we achieved a success rate of 100% in both the group and were not significant. Similarly, Malik et al. (2008),14 Torun et al... (2011),[15] Singh et al. (2007),16 Barak et al. (2008)17 Timanayakar et al. (2011),18 Li et al. (2007),19 and found in their studies that there was no difference in both the techniques with respect to success rate of intubation. Dalal et al. (2015) 23 found a success rate of 100% in Group VL and of 94.2% in Group ML. We also studied and compared the number of attempts required to intubate the patients. If the anesthesiologist had to change the blade, it was considered a second attempt and If the patient could not be intubated after three attempts, it was considered as failure of intubation. More than one attempt was needed in 20% of the cases in group ML while only 3% in group VL and it was statistically significant. Similarly, Jungbauer et al. 200921, found that with video laryngoscopy, 99% patients were intubated in the first attempt, whereas with Macintosh 92% were intubated in the first attempt. This was statistically significant and agreed with the findings of our study. Dalal et al. (2015) 23 had similar findings. In contrast to our study, Studies by Malik et al. (2008),14 Torun et al. (2011),15 Barak et al. (2007)17, and Timanayakar et al. (2011)18 found no significant difference in the number of attempts with both the techniques. In our study, we compared the optimizing maneuvers such as BURP or Bougie required to facilitate intubation with both the techniques. In Group VL, only 16.6% of the patients required rescue manoeuvre to facilitate intubation, whereas 83.4% of the patients did not require any optimizing manoeuvre. In Group ML, 63.3% of the patients required optimising manoeuvre. These findings were statistically significant. Thus, the number of optimizing manoeuvres required to facilitate intubation is significantly less with TrueView EVO2 blade as compared with those using a Macintosh blade. Malik et al. (2008) 22, Dalal et al (2015) 23 had similar findings. Hemodynamic data were comparable in both groups and there was no significant difference. In Group ML there was increased hemodynamic changes attributed to the handling and manipulation. It was less in Group VL, but the increased duration of time taken for intubation made it insignificant in comparison with group VL.
CONCLUSION To conclude our study we could say Tracheal intubation using TrueView Video laryngoscope showed improved laryngeal view with improved in Cormack-Lehane grade by 1-2, with decreased number of attempts and rescue maneuvers in patients with anticipated difficult airway characteristics. There were similar changes in hemodynamics at the cost of increased time taken for intubation, which could be countered by frequently using the instruments and increased expertise. LIMITATIONS: The study could not be double blinded, as the laryngoscopes were significantly different.
REFERENCES
Policy for Articles with Open Access
|
|
 Home
Home