|
Table of Content - Volume 13 Issue 3 -March 2020
Effect of oral clonidine premedication on haemodynamic parameters in patients undergoing laparoscopic surgery
Malti J Pandya1, Dhruvi J Patel2*, Divyang V Shah3 1Additional Professor, 2Resident, 3Professor and HOD, Department of Anaesthesia, Surat Municipal Institute of Medical Education and Research (SMIMER), Bombay Market Road, Surat, INDIA. Email: idhruvi27@gmail.com
Abstract Background: Abdominal surgery can be done by conventional open approach or laparoscopy. Laparoscopy has advantages of less blood loss, small scar and early return to work. The disadvantage of laparoscopic surgery is hemodynamic changes due to CO2 insufflation. Clonidine is an α-2 adrenergic agonist having central sympatholytic properties considered to blunt the stress response to pneumoperitoneum. This study was done to determine the response of oral clonidine premedication on the hemodynamic effects in laparoscopic surgery. Method: Forty patients of ASA grade I and II, aged between 18-60 years undergoing elective laparoscopic surgery under general anaesthesia were divided in to two groups. Group C received Tab clonidine (150µg) and Group P received placebo orally, 90 min before induction. Haemodynamic parameters were compared at baseline, before induction, at the time of intubation, 10 min, 30 min, 60 min after CO2 insufflation, 10 min after CO2 release and at extubation. Results: All patients who received clonidine showed good hemodynamic stability at various intervals during the surgery as compared to placebo. Conclusion: Oral clonidine 90 min before laparoscopic surgeries effectively attenuates the hemodynamic response to pneumoperitonium. Keywords: hemodynamic response, laparoscopic surgery, Oral clonidine, premedication.
INTRODUCTION A large number of abdominal surgeries are performed by a laparoscopic approach nowadays. The advantages of laparoscopy over open surgery are smaller scars, less blood loss, shorter hospital stay, less postoperative complications and early ambulation1. There is increased vascular resistance leading to increase in mean arterial pressure and decrease in cardiac output. Due to compression of Inferior vena cava which further causes reduction in cardiac output and peripheral perfusion. CO2 insufflation also causes diaphragmatic displacement causing reduced lung capacity and compliance, increased V/Q mismatch and hypoxia. These changes in haemodynamics from combined effect of pneumoperitoneum, patient positioning and hypercapnea from the absorbed CO2 makes laparoscopy a challenge for anesthetists.1 To counteract these effects of pneumoperitoneum several non pharmacological and pharmacological means are used. Pharmacological methods include use of β-blockers, a adrenergic agonist, opioids, vasodilators. Clonidine is a centrally acting α-2 receptor agonist. It has central sympatholytic action, reduces peripheral sympathetic discharge and potentiates parasympathetic nervous system5. Oral clonidine has the advantage of ease of administration and it has got excellent bioavailability1. This study was done to determine the effect of oral clonidine premedication on haemodynamic parameters at various intervals during laparoscopic surgeries.
MATERIALS AND METHODS A prospective randomized study was conducted over 40 patients undergoing laparoscopic surgery under general anaesthesia. The patients were divided into two groups. Group C was given tablet clonidine (150µg) orally and Group P was given tablet Vitamin C, 90 min before induction. All the hemodynamic parameters were monitored intra-operatively. Inclusion criteria: Patients between 18-60 years of age of both sexes, ASA grade I and II. Exclusion criteria: Patients with H/O allergy to the drug, Patients with pre-operative cardiorespiratory diseases like hypertension, IHD, valvular heart diseases, patients with psychiatric illness. A detailed history and examination of each patient was done prior to surgery. Basic laboratory investigations like complete haemogram, blood sugar, renal function test were done. ECG and chest x-ray were reviewed. Patients were kept nil by mouth for 6-8 hours prior to anaesthesia. Preoperative informed consent was taken from patients. I.V line was secured and preloading was done. In the pre-operative room baseline pulse rate, systolic and diastolic blood pressure, oxygen saturation were noted. Patients were randomly divided in to two groups: Group C (n=20) received tablet clonidine 150µg 90 min before induction of anaesthesia. Group P (n=20) received tablet Vitamin C 90 min before induction of anaesthesia. All the patients were given Inj. Glycopyrrolate 0.2mg i.m and Inj pentazocine 30mg i.m before 30 minutes of induction of anaesthesia. After shifting the patients to operation theatre standard monitors like pulse oxymetry, ECG, NIBP, ETCO2 were attached and pulse rate, blood pressure (systolic, diastolic and mean) were recorded before induction. Pre-oxygenation was done with 100% oxygen for 3 minutes. Induction was done by inj thiopentone sodium (2.5%) 3-7 mg/kg + inj suxamethonium Chloride 1.5-2 mg/kg iv. + IPPV. Endotracheal intubation was done with appropriate size of cuffed endotracheal tube. Maintenance of anaesthesia was done with O2 (50%) + N2O (50%) + Isoflurane + inj vecuronium bromide. The vitals of the patients were monitored and noted down just before induction of anaesthesia, at the time of intubation, at 10 min, 30 min and 60 min after CO2 insufflation, at 10 min after CO2 release and at extubation. At the end of surgery inj neostigmine 0.05 mg/kg + inj glycopyrrolate 0.008 mg/kg i.v was given. Extubation was done after adequate tidal volume and reflexes were achieved. Any side effects like bradycardia (Pulse rate<60/min), hypotension (decrease in blood pressure more than 20% of baseline), nausea or vomiting were noted. Statistics: All the values were calculated by using open EPI software and paired t-test. Results were expressed in mean and standard deviation.
OBSERVATION AND RESULTS Table 1: Demographic data
In our study there were 11 males and 9 females with average age of 41.85 years and weight of 59.15 in group C and 9 male and 11 female with age 39.85 and weight 59. Both the groups were comparable in terms of demographic data (p>0.05) as seen in table 1. The average duration of surgery was 136+29.3 min in group C and 122 +31.6 min in group P which was comparable and statistically insignificant. Table 2: Comparison of Pulse rate/min
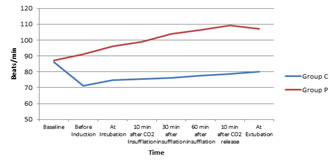
Figure 1: Pulse Rate/min
The mean Pulse rate at baseline was 86 + 6.424 in group C and 87.1 + 8.908 in group P which was statistically not significant (p>0.05) as shown in table 2. There was statistically significant difference in Pulse rate in both groups before induction, at intubation, at 10 min, 30 min and 60 min after CO2 insufflation (p<0.05). After CO2 insufflation both the groups showed increase in pulse rate (Table-2). All patients in Group C showed controlled rise in pulse rate throughout the procedure as compared to patients in Group P. There was no statistically significant difference between pulse rate in both the groups at 10 min after CO2 release and at extubation (p>0.05). Table 3: Comparison of Systolic Blood Pressure(mmHg)
Figure 2: Systolic Blood Pressure(mmHg) The systolic blood pressure in both groups at baseline was comparable (p>0.05) as shown in table 3. The systolic blood pressure before induction in group C and group P was 110.5+7.592 and 126+12.312 respectively(p<0.05). SBP at intubation was 112.5+7.164 in group C and 130+11.459 in group P(p<0.05), at 10 min after CO2 insufflation 117.5+7.164 in group C and 134.5+11.459 in group P(p<0.05), at 30 min after CO2 insufflation 118.5+5.871 in group C and 138+9.515 in group P(p<0.05), at 60 min after CO2 insufflation 120+8.231 in group C and 140.5+8.870 in group P(p<0.05) .At 10 min after CO2 release SBP in group C was 122+8.231 and in group P was 132.5+10.507(p>0.05). At extubation SBP was 124.5+9.445 in group C and 135+8.712 in group P (p>0.05) which was not statistically significant. Table 4: Comparison of Diastolic blood pressure(mmHg)
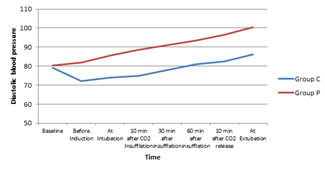
Figure3: Diastolic Blood Pressure(mmHg)
The diastolic blood pressure in both groups at baseline was comparable (p>0.05) as shown in table 4. The diastolic blood pressure before induction in group C and group P was 72+9.515 and 82+5.459 respectively(p<0.05). DBP at intubation was 74+8.608 in group C and 85.5+5.263 in group P(p<0.05), at 10 min after CO2 insufflation 75+8.885 in group C and 88.5+4.871 in group P(p<0.05), at 30 min after CO2 insufflation 78+4.678 in group C and 91+7.707 in group P(p<0.05), at 60 min after CO2 insufflation 81+4.472 in group C and 93.5+7.452 in group P(p<0.05) .At 10 min after CO2 release DBP in group C was 82.5+5.501 and in group P was 96.5+4.894(p>0.05). At extubation DBP was 86+9.403 in group C and 100.5+6.048 in group P which was not statistically significant (p>0.05).
Table 5: Comparison of Mean blood pressure(mmHg)
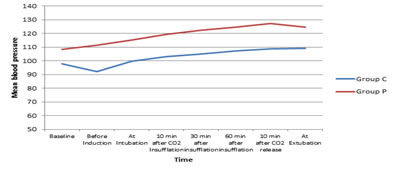
Figure 4: Mean Blood Pressure(mmHg) The Mean blood pressure in both groups at baseline was comparable (p>0.05) as shown in table 5. The mean blood pressure before induction in group C and group P was 92+8.611 and 111.3+10.111 respectively(p<0.05). MBP at intubation was 99.7+6 in group C and 115.2+9.580 in group P(p<0.05), at 10 min after CO2 insufflation 103.3+5.335 in group C and 119.2+9.040 in group P(p<0.05), at 30 min after CO2 insufflation 105+4.674 in group C and 122.3+7.881 in group P(p<0.05), at 60 min after CO2 insufflation 107.3+4.271 in group C and 124.8+7.373 in group P(p<0.05) .At 10 min after CO2 release MBP in group C was 108.8+4.748 and in group P was 127.2+6.238(p>0.05). At extubation MBP was 109+7.422 in group C and 124.8+6.390 in group P which was not statistically significant (p>0.05). Table 6: Comparison of ETCO2
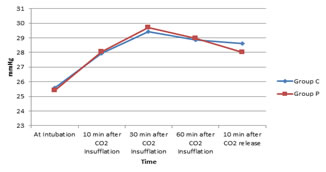
Figure 5: ETCO2 No significant changes in ETCO2 were observed in any patients in both the groups at any stage of surgery (p>0.05) table 6. Table 7: Side effects
Bradycardia was seen in 3 patients and hypotension was seen in 2 patients of group C which did not require inj Atropine (table 7). Hypotension was corrected by fast intravenous normal saline.
DISCUSSION Laparoscopic surgery has replaced many conventional open surgeries. Pneumoperitoneum, increase in intra abdominal pressure and pressure transmitted to thorax, effect of patient positioning in trendelenburg, reverse trendelenburg and lateral position during laparoscopic surgeries causes significant haemodynamic changes. There will be increase in systemic vascular resistance, mean arterial pressure and fall in cardiac index. Increased level of catecholamies and prostaglandins will enhance these effects (2). Clonidine is centrally acting α-2 receptor agonist. It attenuates stress response to surgery and anaesthesia. Clonidine is rapidly absorbed by oral route. The peak plasma concentration is achieved within 60-90 minutes and half life is 12-33 hours. The present study was conducted to evaluate effect of oral clonidine premedication given before 90 minutes of surgery in patients undergoing laparoscopic surgeries under general anaesthesia. Forty patients were divided in to two groups of twenty each. Group C received tab clonidine 150 µg and group P received placebo (tab vit. C) 90 minutes before surgery. In our study, the demographic profile in both the groups in terms of age, sex, weight, ASA status and duration of surgery were comparable(p>0.05). Baseline pulse rate, systolic blood pressure, diastolic blood pressure and mean arterial pressure were comparable in both the groups.(p>0.05). Pulse rate, systolic blood pressure, diastolic blood pressure and mean blood pressure before induction were significantly lower in patients premedicated with oral clonidine than placebo (p<0.05). At intubation, 10 minutes after pneumoperitonem and 30 and 60 minutes after that pulse rate, systolic blood pressure, diastolic blood pressure and mean arterial pressure were significantly increased in group P as compared to group C in which the haemodynamic parameters remained close to baseline (p<0.05).This shows the significant and consistent attenuation of haemodynamic stress response by clonidine compared to placebo group. At 10 minutes after CO2 release and at extubation pulse rate, systolic blood pressure, diastolic blood pressure and mean blood pressure remained on lower side than placebo group but the difference was not statistically significant (p>0.05). Pressure required to maintain pnuemoperitoneum was kept between 12-15 mmHg throughout the surgery. There was no statistically significant difference in ETCO2 in both the groups (p>0.005). In a randomized controlled study of 60 patients done by Mrunalini Patel and Neelam Parmar, 30 patients were given tab clonidine 3ug/kg (group CL) and 30 patients(group C) were not given any oral premedication. They observed pulse rate, systolic Blood pressure and diastolic blood pressure before premedication, before induction, before intubation, after intubation, before pneumoperitoneum, 15 min after pneumoperitoneum, 30 min after pneumoperitoneum, 10 min after CO2 release and after extubation. They found that pulse rate, systolic blood pressure and diastolic blood pressure were comparable at the baseline. Pulse rate, Systolic blood pressure and diastolic blood pressure remained low and steady throughout the surgery in CL (clonidine) group as compared to group C (placebo) in which pulse rate, systolic blood pressure and diastolic blood pressure were increased after induction and throughout the surgery. The difference was statistically significant (p<0.05). In our study we also found the similar results. Shivinder singh et al., Sunita Goel et al., C.B Shridhar et al. and Anshu Mali et al. also did similar study and found that oral clonidine gives better hemodynamic control during laparoscopic surgery with minimal adverse effects like nausea or vomiting. Similar results were found in our study.
CONCLUSION Oral clonidine in a dose of 150µg 90 min before induction in patients undergoing laparoscopic surgery is very effective, easy to administer and cost effective. It gives good hemodynamic stability during surgery, attenuates stress response due to intubation, pneumoperitoneum and surgery. REFERENCES
Policy for Articles with Open Access
|
|
 Home
Home