|
Table of Content - Volume 13 Issue 3 -March 2020
A study of Airtraq versus Macintosh laryngoscope with respect to ease of intubation at tertiary health care centre
Ramakant G Alapure1, Sonal Anil Chaudhari2*, Nilesh Badukale3
1,2Associate Professor, Department of Anaesthesiology, Government Medical College And Cancer Hospital, Aurangabad, Maharashtra. 3Speciality Medical Officer, Amravati, Maharashtra, INDIA. Email: sonal.pachore@rediffmail.com
Abstract Background: Endotracheal intubation of patients undergoing surgical procedure is an effective method for controlling airway. However conventional laryngoscopy using Macintosh laryngoscope for endotracheal intubation is not easy in every case. The anesthesiologist must be familiar with various other new techniques for endotracheal intubation. Airtraq is one of the new technique for endotracheal intubation. In our study, the main objective is to compare the ease of intubation by using Airtraq versus Macintosh laryngoscope for endotracheal intubation. Materials and methods: Prospective, randomized study of Airtraq vs. Macintosh laryngoscopy in tracheal intubation under general anaesthesia. Study was approved by the institutional medical ethics committee and written informed consent was obtained from all patients participating in the study. 80 patients of either sex aged between 18-70 years of ASA grade I, II and III undergoing surgery under general anaesthesia with Monitored Anaesthesia Care were enrolled in the study. Results: A single-centre, prospective, comparative, parallel-group, interventional, randomized study was done. 80 patients of either sex aged 18-70 years were allocated randomly by chit block method in two groups containing 40 patients each to study Airtraq vs. Macintosh laryngoscopy in tracheal Intubation under general anaesthesia. In Airtraq group, Intubation was Easy in 29(72.5%) of patients, Satisfactory in 11(27.5%) of patients And Difficult in 00 (0%) of patients. in Macintosh group Intubation was Easy in 27 (67.5 %) of Patients, Satisfactory in 09(22.5%) of patients And Difficult in 04 (10%) of patients. P value was 0.06 and that is >0.05 so it was not statistically significant Conclusion: We conclude that Airtraq laryngoscope requires less optimization maneuvers as compared to Macintosh laryngoscope. Ease of intubation increased by Airtraq laryngoscope as compared to Macintosh laryngoscope. Procedure related complications were less in Airtraq laryngoscope than Macintosh laryngoscope. Key Words: Endotracheal intubation, Macintosh laryngoscopy, Airtraq laryngoscope
INTRODUCTION Endotracheal intubation of patients undergoing surgical procedure is an effective method for controlling airway. However conventional laryngoscopy using Macintosh laryngoscope for endotracheal intubation is not easy in every case. Tracheal intubation is a potentially lifesaving procedure in many clinical situations failure to successful tracheal intubation is a leading cause of morbidity and mortality.3 Various tools has been used to examine vocal cords since the mid-1700s. These tools were continuously modified, which allowed for many advances in laryngoscopy and eventually played a pivotal role in anaesthesiology.4The Macintosh laryngoscope is the most commonly used device for intubation. It is considered to be the standard for endotracheal intubation and it is against this device that the various airway devices are evaluated. Failure to intubate may result in dental damage, laryngeal spasm, bronchospasm, bleeding from the upper airway, hypoxia, hypecarbia, regurgitation/vomiting, various dysrrhythmias, cardiac arrest, brain damage or even fatalities. It has always been a challenge for the anaesthesiologist; therefore, he should be forearmed for such situations. In pursuit of this, it became necessary to have certain tools or access to advanced airway instrumentation for better visualization of the larynx. This led to the invention of the lighted stylet and a number of indirect fiber optic laryngoscopes such as flexible fiber scope, Bullard scope, Usher scope and the Wu scope. The Airtraq is now new intubation device design to provide a view of the glottis without requiring alignment of the oral, pharyngeal and tracheal axes. The blade of Airtraq consists of two side by side channels. The Airtraq has been reported to limit cervical spine movement. In our study, the main objective is to compare the ease of intubation by using Airtraq versus Macintosh laryngoscope for endotracheal intubation.
AIMS AND OBJECTIVES Primary outcome To compare the airtraq versus macintosh laryngoscope with respect to ease of intubation in terms of
Secondary outcome To compare Post operative complications in Airtraq Vs Macintosh laryngoscopy technique.
MATERIALS AND METHODS This study was conducted in operation theatres of Medical College and Hospital. It was designed as a prospective, comparative, observational, randomised trial. Following Human Research and Ethics Committee approval, informed consent was obtained from 80 ASA I, II and III patients, aged between 18 and 70 years, belonging to either gender with Mallampati classification I and II, undergoing elective surgery requiring general anaesthesia with oral endotracheal intubation and patients willing to participate in the study to give consent. Patients refusal to participate in the study, Mallampati class III and IV, interincisor distance < 2 cm, gastroesophageal reflux disease, hiatus Hernia, Pregnancy, Patient requiring regional anaesthesia, History of difficult Intubation, Intraoral mass, Face and Neck deformity, were excluded from the study. The sample size for our study was calculated According to the rule of normal distribution statistical parameters for all the groups like mean, standard deviation and coefficient of variation will be calculated for the quantitative data.from S. K. Lwanga, S. Lemeshow. Sample Size Determination in Health Studies. A Practical Manual. World Health Organization Geneva 1991. Forty adult patients who were undergoing elective surgery under general anaesthesia with intubation using Airtraq, was included in Group A. Another forty adult patients who were undergoing elective surgery under general anaesthesia with intubation using Macintosh laryngoscope was included in Group M. All patients received a standardized general anaesthesia with controlled ventilation technique. Standard monitoring, including electrocardiography, non-invasive blood pressure, oxygen saturation measured by pulse oximetry and end-tidal carbon dioxide level measurement by capnometry were used in all patients.All Patients Preoxygenated with 100% oxygen for 3 mins. All patients were premedicated with Inj. ondansetron 0.08 mg/kg, inj. midazolam (0.02mg/kg) and inj.fentanyl (2μg/kg) intravenously. A sleep dose of propofol (2 mg/kg) was titrated to induce anaesthesia. After checking bagmask ventilation patient relaxed with. Inj. Succinylcholine 2mg./kg. After ventilation of patient laryngoscopy was done with Airtraq or Macintosh laryngoscope and intubated with appropriate size tube by an anaesthesiologist with either of two blades and placement of endotacheal tube was confirmed by equal chest movement, equal air entry, and capnography. Patient was mechanically ventilated during procedure after confirmation of intubation. Anaesthesia was maintained with intermittent positive pressure ventilation with oxygen and nitrous oxide, muscle relaxation with inj. vecuronium 0.08mg/kg and inhalational agent sevoflurane. For patients in group A, laryngoscopy was done using Airtraq with premounted endotracheal tube. For female patient small adult size (green) Airtraq was used with premounted number 7 portex cuffed endotracheal tube. For male patient large adult size (blue) Airtraq with premounted number 8.5 portex cuffed endotracheal tube was used. After visualisation of vocal cords through Airtraq, endotracheal tube was advanced through cords under vision. For patients in group M, laryngoscopy was done using Macintosh laryngoscope. Patients were intubated with appropriate size endotracheal tube under direct laryngoscopic vision. After intubation in both groups, tracheal cuff was inflated and anaesthesia breathing circuit was connected to start positive pressure ventilation. Time for appearance of first square waveform of ETCO2 was noted. Hemodynamic parameters were observed during laryngoscopy, intubation and after intubation at the following points of time 0 min, 1min. 2 mins, and 3 mins. During this period, patient was maintained on oxygen, nitrous oxide (40:60) and one minimum alveolar concentration (MAC) of sevoflurane with balanced anaesthesia technique and no surgical stimulus in the form of incision were given. Hemodynamic parameters monitoring, POGO score, successful intubation, successful intubation time, optimization manoeuvres required, ease of intubation andairway trauma during procedure were recorded. Total intubation time was taken as summation of duration of laryngoscopy and intubation. It was calculated from the time, the facemask is taken off patient’s face to appearance of first square waveform on capnograph. Complications like trauma, sore throat, hoarseness of voice etc. were noted immediately after intubation and 24 hours postoperatively. In case of failure to intubate any of the patients in two attempts, it was managed by in charge anesthesiologist as per difficult intubation protocol. MONITORING PARAMETERS:
I) POGO score -percentage of glottic opening during direct laryngoscopy -100%-entire glottic structures visible -33%-only lower third of vocal and arytenoid visible -0%- no glottic structure visible II) Optimization manoeuvre required was assessed on a score of 0 to 2 o- No maneuvers required 1-External laryngeal pressure 2-Use of style III)Ease of intubation score Grade 1-Extrinsic manipulation of larynx not required Grade 2- Extrinsic manipulation of larynx required Grade 3-Intubation possible with stylet guided Grade 4-Failed intubation RESULTS A single-centre, prospective, comparative, parallel-group, interventional, randomized study was done. 80 patients of either sex aged 18-70 years were allocated randomly by chit block method in two groups containing 40 patients each to study Airtraq vs. Macintosh laryngoscopy in tracheal Intubation under general anaesthesia. The observation and results of the comparative study of the two groups was as follows.
Table 1: Comparison of groups demographic characteristics
(P Value: Not significant > 0.05, Significant< 0.05, highly significant < 0.001); *P value not significant if p >0.05; Demographic data was not statistically significant. Table 2: Comparison of groups according to ASA and MPC Grade
(P Value: Not significant > 0.05, Significant< 0.05, highly significant < 0.001); Pearson chi-square test applied. *P value not significant if p >0.05 ASA and MPC grade were not statistically significant in both groups. Heart rate: Above data shows that there was rise in heart rate in both the group but significant rise was seen in patient in M-group as compared to patient in A- group. P value at o minutes was 0.80,at one minute was 0.02,at two minutes 0.02, and at three minutes was 0.05. P value was <0.05 and it was statistically significant.
Table 3: Comparison of groups according to heart rate at various interval (Beats per min)
(P Value: Not significant > 0.05, significant< 0.05, highly significant < 0.001)
Mean BP: Above data shows that there was rise in mean BP in both the group but significant rise was seen in patient in M-group as compared to patient in A- group. P value at o minutes was 0.07,at one minute was 0.17,at two minutes 0.06 , and at three minutes was 0.10. P value was >0.05 and it was not statistically significant Table 4: Comparison of groups according to mean BP at various interval
(P Value: Not significant > 0.05, significant< 0.05, highly significant < 0.001) SPO2: Above data shows that P value at o minutes was 0.83,at one minute was 0.84,at two minutes 0.29 , and at three minutes was 0.22. P value was >0.05 and it was not statistically significant. Table 5: Comparison of groups According to SPO2 at Various Interval
(P Value: Not significant > 0.05, Significant< 0.05, highly significant < 0.001)
ETCO2: Above data shows that P value at o minutes was 0.30, at one minute was 0.49, at two minutes 0.9, and at three minutes was 0.98. P value was >0.05 and it was not statistically significant. Table 6: Comparison of groups According to ETCO2 at Various Interval
(P Value: Not significant > 0.05, Significant< 0.05, highly significant < 0.001)
POGO score: In Airtraq group, POGO score is 1 in all 40(100%) patients while in Macintosh group POGO score is 1 in 27 (67.5%), POGO score is 2 in 11(27.5%) and POGO score is 3 in 02 (5%) Patients Required External Laryngeal Pressure And 04 (10 %) Patients. P value was 0.065. It was >0.05 so not statistically significant Table 7: Comparison of groups according to POGO score
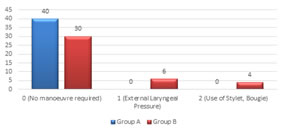
(P Value: Not significant > 0.05, Significant< 0.05, highly significant < 0.001) Optimization manoeuvres: In Airtraq group, No patient Required any optimization Manoeuvre. and in Macintosh group 06 (15 %) Patients Required External Laryngeal Pressure And 04 (10 %) Patients Required Use of Stylet, Bougie for Intubation. P value was 0.065.* P value was >0.05 and it was not statistically significant Table 8: Comparison of groups according to optimization manoeuvres
(P Value: Not significant > 0.05, Significant< 0.05, highly significant < 0.001)
Graph 1: Comparison of groups according to optimization manoeuvres
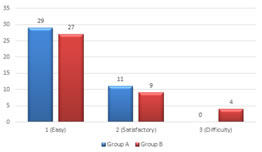
Ease of Intubation: In Airtraq group,Intubation was Easy in 29(72.5%) of patients , Satisfactory in 11(27.5%) of patients And Difficult in 00 (0%) of patients. in Macintosh group Intubation was Easy in 27 (67.5 %) of Patients, Satisfactory in 09(22.5%) of patients And Difficult in 04 (10%) of patients. P value was 0.06.* P value is >0.05 and it was not statistically significant. Table 9: Comparison of groups according to Ease of Intubation
(P Value: Not significant > 0.05, Significant< 0.05, highly significant < 0.001)
Graph 2: Comparison of groups according to ease of intubation Side Effects: Above data shows that P value for Sore throat was 0.146, for injury to airway was was 0.216,and for hoarsness was 0.09. P value was >0.05 and it was not statistically significant. Table 10: Comparison of groups According to Side Effects
(P Value: Not significant > 0.05, Significant< 0.05, highly significant < 0.001) DISCUSSION Observing the glottis during intubation is a reliable method for correct placement of ETT. Direct vision avoids trauma while negotiating the tube into trachea. Multiple attempts to endotracheal intubation increase the morbidity related to the airway management. Difficult airway and poor glottis view are associated with airway manipulation and several attempts at laryngoscopy.6 Our study design consist of 80 patients of either sex aged between 18-70 years of ASA grade I ,II And III undergoing surgery under general anaesthesia with Monitored Anaesthesia Care were enrolled in the study. They were randomly divided into two groups of 40 patients in each group. Group M patients were intubated with Macintosh laryngoscope and group A patients were intubated with Airtraq laryngoscope. Standard general anaesthesia was given with inj midazolam, inj fentanyl, inj propofol, and inj vecuronium. Post operative complications were observed after intubation , after extubation and after 24 hrs of completion of operative procedure. Thus distribution of patients according to age, sex ,weight, height, BMI , Interincissor distance, ASA and MPC was comparable and statistically not significant (P>0.05) In our study group A patients did not required any optimization manoeuvre. and in group M 06 (15 %) Patients required external laryngeal pressure and 04 (10 %) patients required use of stylet, bougie for intubation. P value was 0.065. P value was >0.05 and it was not statistically significant, though it was not statistically significant it was clinically significant. Similar results were reported by Maharaj CH, O' Croinin D et al. ( 2006)4 and Geeta Bhandari, K. S. Shahi et al. (2013)14 POGO score was also better in the Airtraq group.it was of grade I in100% of patients in Airtraq group versus 67% (27) in the Macintosh group,p<0.001.In Macintosh group , the POGO score was 2 in 27%(11) and grade 3 in 5%(2). It was similar to the observations of Koh et al. In our study ease of intubation score was also better in the Airtraq group. In group A, intubation was easy in 29(72.5%) of patients , satisfactory in 11(27.5%) of patients and difficult in 00 (0%) of patients while in group M intubation was easy in 27 (67.5 %) of patients, satisfactory in 09(22.5%) of patients and difficult in 04 (10%) of patients. P value was 0.06 and it was not statistically significant, though it was clinically significant. Similar studies conducted byWaleed Riad, Ashraf Moussa, David T. Wong et al.(2012)12 and Geeta Bhandari, K. S. Shahi et al. (2013)14 and found that ease of intubation was better in the Airtraq group. In our study there was rise in heart rate and mean blood pressure in both the group but significant rise was seen in patient in M-group as compared to patient in A- group. Similar results were seen by Marwa A, Tolon et al. (2012)11 and Waleed Riad, Ashraf Moussa,David T. Wong et al.(2012)12.There was no statistical significant difference in SPO2 and ETCO2 in both groups The postoperative complications were comparable in both the groups. The incidence of sore throat was less in the Airtraq group than in the Macintosh group. laryngospasm and hoarseness were not observed in any patient in both the groups. There was no incidence of lip trauma, dental trauma, and blood tinged secretions over the laryngoscope blade and ETT in any case in both the groups.These results were Similar with studies conducted by Geeta Bhandari, K. S. Shahi et al. (2013)14.
CONCLUSION We conclude that Ease of intubation increased by Airtraq laryngoscope requiring less optimization maneuvers and more haemodynamic stability as compared to Macintosh laryngoscope during endotracheal intubation. Procedure related complications were less in Airtraq laryngoscope than Macintosh laryngoscope. This can be ensured by including Airtraq laryngoscope in the training of anesthesiologists followed by large multicentre trials providing more definite results.
REFERENCES
Policy for Articles with Open Access
|
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
 Home
Home