|
Table of Content - Volume 13 Issue 3 -March 2020
Natasha Gupta1*, B Sanjeevkumar2, Madiha Shadab3, Umesh Kumar Badani4
1Attending Consultant, Department of Anesthesia, Paras Hospital, Patna, Bihar, INDIA. 2Indira Gandhi Medical College and Research Institute, Pondicherry, INDIA. 3Senior Resident, Department of Anesthesia, Patna Medical College and Hospital, Patna, INDIA. 4Professor & HOD, Department of Anesthesia, All India Institute of Medical Sciences, Patna, Bihar, INDIA. Email: gupta.natasha2010@gmail.com
Abstract Background: Foreign body aspiration is one of the leading causes of mortality in children and for removal of the same in children there is no substitute for rigid bronchoscope. But the question is that whether to use spontaneous or controlled ventilation during the removal of foreign body with least complications. Methods: This prospective comparative study was conducted among children who required foreign body removal using rigid bronchoscopy under general anesthesia with either spontaneous or controlled ventilation in AIIMS, Patna during month of January 2018 to April 2019. Sixty two children between age group of 1-12 years, who aspirated foreign body that lodged into the respiratory tract, were included in the study. Among them thirty two participants received controlled ventilation and thirty participants received spontaneous ventilation. Statistical analysis was done using SPSS version 17. Results: Age, weight, type and location of foreign body of the participants in both the groups were similar. Complications like intra operative coughing and buckling, laryngospasm, post operative laryngeal edema, post operative severe cough was noted in 3.1%,3.1%,9.4% and 6.3% of the controlled ventilation group and 23.3%, 6.7%, 13.3%, 6.7%, and 3.3% of the spontaneous ventilation group children respectively. Proportion of overall complications in controlled group and spontaneous ventilation group was found to be 21.9% and 53.3% respectively and also the difference between the two groups was found to be statistically significant. (p=0.0112) Conclusion: In order to maintain an adequate depth of anesthesia, controlled ventilation is comparatively better than spontaneous respiration as the proportion of intraoperative coughing and bucking was significantly reduced. Key words: Spontaneous, controlled ventilation, foreign body, children, bronchoscopy
INTRODUCTION Foreign body aspiration and lodging into the respiratory tract is a life threatening condition commonly occurs in infants between one to three years old, with a peak incidence in the second year of life1-3. Among the substances inhaled organic substances especially food ranks the top1-3. Foreign body aspiration is one of the leading causes of mortality in children 1–3 years old4 and most deaths occur at the time of aspiration, itself. Also several studies, reported the mortality as zero for patients who reach the hospital alive1,2,4. Some foreign bodies lodge in the trachea, but the majority are found in the proximal airways which usually based on the size and shape of the inhaled foreign body. At times, small, sharp objects can lodge in the subglottic area, where they can be difficult to diagnose5. Usually child will presents with a history of a choking episode at the time of aspiration where as fever and the symptoms and signs of a chest infection are typical presenting symptoms in those who are first seen more than 24 h after aspiration6,7. A plain chest X-ray may rarely show an inhaled foreign body or foreign body may be suspected by comparing inspiratory and expiratory films that may reveal an area of hyperinflation because of gas trapping and/or mediastinal shift. For the removal of aspirated foreign bodies in children there is no substitute for a rigid ventilating bronchoscope. It provides a much better quality of visualization and larger channels for instrumentation. During the procedure of rigid bronchoscopy it is very difficult to maintain adequate oxygenation and ventilation in children as pulmonary gas exchange is already deranged8. The controversy is than whether spontaneous or controlled ventilation is the best choice for removal of foreign body using rigid bronchoscopy. Arguments in favor of spontaneous ventilation include the lower risk compared with controlled ventilation that the foreign body may move more distally, which would increase the difficulty of removal and possibly lead to ball-valve obstruction of the airway8. In addition, spontaneous ventilation allows for continued ventilation during removal of the foreign body and rapid assessment of the adequacy of the airway after removal of the foreign body. At the same time, an important complication that occurs with spontaneous ventilation is that reduction in depth of anesthesia when compared to controlled ventilation but advantage in case of controlled ventilation is that use of balanced anesthesia. Hence in order to get much clearer picture on this view, this study was conducted to assess the clinical profile and complications of spontaneous and controlled ventilation which is used for children undergoing foreign body removal using rigid bronchoscopy.
MATERIALS AND METHODS This prospective comparative study was conducted among children who required foreign body removal using rigid bronchoscopy under general anesthesia with either spontaneous or controlled ventilation in AIIMS, Patna during month of January 2018 to April 2019. Sixty two children between age group of 1-12 years, who aspirated foreign body that lodged into the respiratory tract, were included in the study. Children with signs of lower respiratory tract infection, known case of bronchial asthma and primary complex were excluded from the study. The study was approved by the ethical committee of this institution. Informed consent was obtained from the child’s parents, before starting the study. The study patients were divided into two groups with thirty two participants in controlled ventilation group and thirty participants in spontaneous ventilation group. All the patients were pre medicated with atropine (20mcg/kg) and dexamethasone (0.6mg/kg), they were induced with propofol (2mg/kg). Children were allotted to spontaneous and controlled ventilation based on computer generated random numbers. After induction only children receiving controlled ventilation were administered with depolarising muscle relaxant, succinylcholine (2mg/kg) to facilitate introduction of rigid bronchocope into the trachea. Maintenance of the airway and controlled ventilation was administered using 100% oxygen with 3% sevoflurane and intermittent boluses of propofol in the dose of 0.5mg/kg. This helps in obtunding the airway reflexes and controlling the ventilation by connecting jackson rees’ circuit to the ventilating port of the rigid bronchoscope. No sedative premedication or narcotic analgesics were used to enable early return of airway reflexes and to avoid respiratory depression after retrieval of the foreign body. Nitrous oxide was avoided to prevent desaturation and potential pulmonary inflation and rupture. With intermittent boluses of propofol and administration of 3% sevoflurane, patients did not require the need for non-depolarising muscle relaxants for ease of ventilation. Patients were well relaxed and no airway resistance was encountered during controlled ventilation using jackson rees’ circuit. Effective airway management without the need for non-depolarising muscle relaxants for spontaneous ventilation and avoidance of airway complications such as intraoperative and postoperative bronchospasm and pneumothorax due to administration of adequate airway pressures using jacson rees’s circuit was achieved using this technique. In the absence of the use of non-depolarising muscle relaxants, return of spontaneous ventilation during the procedure can be encouraged if patients cannot be adequately ventilated during the procedure. All children were monitored continuously for heart rate (HR), electrocardiography (ECG), pulse oximetry (SpO2), and endtidal carbon dioxide (PECO2) and noninvasive blood pressure (NIBP) continuously throughout the procedure and during immediate post operative period. Detailed history and the observations were documented in a proforma by the principal investigator. Data was entered in Microsoft excel and data analysis was done using statistical tests like chisquare test, two proportion Z test and independent sample t test, wherever appropriate in Statistical Package for Social Sciences (SPSS) version 17.
OBSERVATIONS AND RESULTS This study on foreign body removal among children, in controlled ventilation group 65.6% of the participant were under 1 year of age, followed by 18.8% of the participants were 2-3 years old and 15.6% participants were above 3 years of age. In spontaneous ventilation group 63.3% of the participants were infants, 13.3% of the participants were between 2-3 years of age and 23.3% participants were above the age of three. In controlled ventilation group 59.4% of the participants were male children and in spontaneous ventilation group 70% of the participants were male children. Female participants were 40.6% and 30% in Controlled ventilation group and Spontaneous ventilation group respectively. Participants below 10 kg were noted to be 37.5% in controlled ventilation group and 46.7% in spontaneous ventilation group for foreign body removal. Between the ranges, 11 to 20 kgs there were 59.4% and 46.7% participants in controlled and spontaneous ventilation group respectively. Participants above 20 kgs were 3.1% in controlled ventilation group and 6.7% in spontaneous ventilation group respectively. There was no statistical weight difference in both the groups. Table 1: Characteristics of the study participants in both groups
In this study Organic foreign body was found to be most common in 81.3% and 83.3% of the toddlers in controlled and spontaneous ventilation group respectively. Foreign body location was in right main bronchus for 59.4% and 60% of the children in controlled and spontaneous ventilation group accordingly and the difference was not statistically significant. Foreign body retention time period was more than 3 days in 37.5% of the children in controlled ventilation group and 46.7% of the children in spontaneous ventilation group, which shows no statistical difference in foreign body retention time between the two groups. (p > 0.05)
Table 2: Type, location and duration of foreign body in both groups
Complications like intra operative coughing and buckling, laryngospasm, post operative laryngeal edema, post operative severe cough was noted in 3.1%,3.1%,9.4% and 6.3% of the controlled ventilation group and 23.3%, 6.7%, 13.3%, 6.7%, and 3.3% of the spontaneous ventilation group children respectively. Reintubation was done for a single child under spontaneous ventilation group. The p value was found to be statistically significant for intra operative coughing and buckling (p=0.0186), which shows there is difference between controlled ventilation group and spontaneous ventilation group. The p value for laryngospasm (p=0.5127), post operative laryngeal edema (p=0.6305) and post operative severe cough (p=0.9495) was found to be not statistically significant. Proportion of overall complications in controlled group and spontaneous ventilation group was found to be 21.9% and 53.3% respectively and also the difference between the two groups was found to be statistically significant. (p=0.0112) Table 3: Proportion of complications in each group
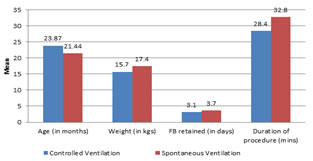
*Significant Mean age (in years) of the participants in controlled group and spontaneous group was found to be 23.87±19.6 and 21.44±18.34, respectively. Similarly mean weight (in kgs) of the participants in controlled group and spontaneous group was found to be 15.7±8.9 and 17.4±9.1, respectively. Duration of foreign body retained (in days) in controlled group and spontaneous group was found to be 3.1±2.4 and 3.7±2.9, respectively. Duration of procedure (in mins) in controlled group and spontaneous group was found to be 28.4±11.5 and 32.8±10.7, respectively. There was no statistical significance in the mean age, weight of the child, foreign body retention time period, duration of procedure. Foreign body removal percentage was 93.8% in controlled ventilation group 86.7% in spontaneous ventilation group, but the difference was not found to be statistically significant in this study.
Figure 1: Comparison of clinical profile between two groups DISCUSSION In this study it was found that foreign body inhalation was more common among males children than females children and also it was found to be more with organic substances than inorganic substances. Foreign bodies were more commonly lodged in the right bronchus than the left bronchus. These results were similar to the reports published in various epidemiologic and demographic studies conducted by Hui et al 9 and Jose et al 10. This study recorded few adverse events notably intraoperative coughing with bucking followed by post operative laryngeal edema, severe cough and laryngospasm. One case in the spontaneous ventilation group required reintubation. The overall complication rate was comparable with that reported in the studies conducted by Jose et al10, Pinzoni et al 11 and Hasdiraz et al12. Ahmed et al13 reported that all children who underwent foreign body removal with rigid bronchoscopy had suffered from some respiratory embarrassment intraoperatively and Perrin et al14 found that they had to assist respiration in spontaneously breathing patients undergoing rigid bronchoscopy because of prolonged apnea or oxygen desaturation. Litman et al15 reported that spontaneous ventilation was not sufficient to maintain normoxia or paralysis was required because patients were moving and hence change in ventilatory technique from spontaneous or assisted to controlled ventilation was needed and not vice versa. Woods et al16, Kim et al 17 and Ahmed et al13 stated that the possible complication of forcing the foreign body further into the bronchial tree, as the reason for not avoiding controlled ventilation. Pawar et al 18 has given an account of four cases in which the foreign body was dislodged fourteen times during removal in both spontaneous as well as controlled ventilation, but there was no incidence of the foreign body being pushed distally. In our study there was no incidence of the foreign body being pushed down the bronchial tree during removal in either of the groups. Several complications were reported by Fearson et al19, Chatterji et al20, Baraka et al21, Kosloske et al22 and Blazer et al23 with the use of rigid bronchoscopy includes coughing and bucking, pneumothorax, mediastinal and subcutaneous emphysema, laryngospasm, laryngeal edema, cardiac arrhythmia, cardiac arrest, convulsions and death19-23. These could be due to many reasons such as inadequate ventilation, hypoxia, vagal stimulation and inadequate depth of anesthesia. In our study the complications in both the groups shows no statistical difference except for intraoperative coughing and bucking, which was worse in spontaneous ventilation patients probably because of inadequate depth of anesthesia. In this study, proportion of overall complications in spontaneous ventilation group was found to be higher than controlled group and the difference was found to be statistically significant.
CONCLUSION From this study, we conclude that in order to maintain an adequate depth of anesthesia, controlled ventilation is comparatively better than spontaneous respiration as the proportion of intraoperative coughing and bucking were significantly reduced, during rigid bronchoscopy for removal of inhaled foreign body in children.
ACKNOWLEDGEMENT I would like to thank all, who has guided me by extending their knowledge and experience right from the inception to the completion of the work. Also, I would like to acknowledge the medical superintendent and all the staffs, for their support during the study period. Last but not least I am thankful to my study participants, without whom, this study would not have been possible. Declarations Funding: No funding source Conflict of interest: None declared Ethical approval: This study was registered with Institutional Human Ethical Committee.
REFERENCES
Policy for Articles with Open Access
|
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
 Home
Home