|
Table of Content - Volume 13 Issue 3 -March 2020
Comparison of efficacy of ondansetron and granisetron for the control of postoperative nausea and vomiting in patients undergoing surgery under general anaesthesia
Supriya Biradar1, Manohar Mane2*, Jyotsna S Paranjpe3
1Junior Resident II, 2Professor,3Professor & HOD, Department of Anaesthesiology, Bharati Vidyapeeth (Deemed To Be University), Medical College And Hospital, Sangli. 416414, INDIA.
Abstract Background: Post operative Nausea Vomiting (PONV) is the most frequent complaint patients report following surgery under anesthesia and is the leading cause of unanticipated hospital admission following outpatient surgery. PONV increases patient discomfort, adds to hospital expenditure, and complications related to vomiting. Aims and Objectives: To compare the efficacy of ondansetron and granisetron for control of postoperative nausea and vomiting in patients undergoing surgery under General Anaesthesia and to study and compare adverse effects caused by these drugs. Material and Methods: Sixty ASA I and II patients, aged 18-60 years, scheduled for surgery under General Anaesthesia were studied after randomization into two groups. Group A received inj ondansetron 4mg intravenously and Group B patients rerceived inj.Granisetron 2mg intravenously. Anesthesia techniques were standardized in all the patients. The postoperative nausea and vomiting scoring was started immediate post-extubation. The patients were monitored in the recovery unit for the initial two hours. During that period the incidence of nausea and vomiting were recorded every 15 minutes. The nausea and vomiting scoring was continued sixth hourly for the next 24 hours. Result : It was observed that in Group A( n=30) receiving inj Ondansetron,9 patients (30%) developed nausea, out of which 4 patients had nausea at extubation which gradually decreased to 3 patients having nausea at 30 min, 1 patient had nausea at 90 min and 1 at 6 hour and 6 patients (20%) developed vomiting. In Group B (n=30) receiving inj Granisetron,6 patients (20%) developed nausea, out of which 2 patients had nausea at extubation, 2 at 6o min and 1 patient had nausea at 45 min and 1 at 120 min and 2 patients (6.6%) developed vomiting. Conclusion: Inj.granisetron is more effective in comparison to inj.ondansetron in prevention of PONV in patients undergoing surgery under general anesthesia Key words – Postoperative nausea vomiting, ondansetron and granisetron.
INTRODUCTION Along with pain, PONV is the most frequent complaint patients report following surgery under anesthesia and is the leading cause of unanticipated hospital admission following day care surgery. A patient who experiences nausea or has emesis within 24 hours of a surgical procedure that required anesthesia meets the criteria for the diagnosis of PONV. Nausea occurs in up to 40% of patients who undergo general anesthesia but can be as high as 80% in high-risk patients1. PONV is thought to be multifactoral, involving anaesthetic, surgical, and individual risk factors.1 The risk factors for PONV are female gender, non smoking status, history of motion sickness or PONV, use of opiod analgesics and volatile anaesthetics is well established1,2,3.The sequence of events that occur during emesis are controlled by the vomiting “center,” which lies in the medulla oblongata and consists of the nucleus of the tractus solitarius and parts of the reticular formation. The chemoreceptor trigger zone (CTZ), in area prostrema detects chemicals in the bloodstream, sends signals via neural networks, which activate the vomiting center. The area prostrema of the brain is rich in dopamine, opioid, and serotonin or 5-hydroxytryptamine (5HT3) receptors4. Four major neuro transmitter systems appear to play important roles in mediating the emetic response viz. dopaminergic, histaminic (H1), cholinergic, muscarinic and 5HT3[4]. 5-hydroxytryptamine-3 receptor antagonists (5HT3RA) are popular drugs because of their similar efficacy to droperidol or dexamethasone and minimal side-effect profile5. The 5HT3 receptor antagonists produce no sedation, extrapyramidal reactions ,adverse effects on vital signs or laboratory tests or drug interactions with other anaesthetic medications6. Other antiemetics like dopamine antagonists produce extrapyramidal effects, sedation, hypotension, negative inotropy, anticholinergic drugs produce sedation, central anticholinergic syndrome and antihistamines cause tachycardia, drowsiness, blurred vision and pain on injection as side effect7. A large number of drugs are available for prevention of PONV, of which 5-HT3 receptor antagonists have occupied an important position because of their better efficacy minimal side effects. The commonly used drug is ondansetron, 4 mg intravenously is the effective dose to prevent PONV8. Recently introduced another 5HT3 receptor antagonist granisetron has more potent and longer acting activity than ondansetron9 This study was done to compare the efficacy of ondansetron and granisetron for the prevention of post operative nausea and vomiting.
MATERIAL AND METHODS After obtaining institutional ethical committee approval (IEC-316/19, dated 14/11/19) and written and informed consent for surgeries under general anaesthesia, all ASA I /II patients of age group 18 years to 60 years undergoing surgery in stipulated time of 6 months under General Anesthesia were enrolled for this study. Patients who refused to get enrolled in the study were excluded from the study. Patients admitted for surgery were nil per orally for 8-10 hours. At the pre anaesthetic interview the patients were familiarized with a postoperative questionnaire . On arrival in the operating room, routine monitoring devices were placed, and baseline blood pressure, heart rate and pulse oximetry values were recorded. Patients were randomly divided in two groups by lottery method. Group A received 2 ml (4 mg) inj ondansetron i.v. and Group B received 2 ml (2 mg) inj granisetron i.v. 2 minutes before induction . Anesthesia was induced with inj. Fentanyl 2mcg/kg, inj. propofol 2mg/kg and inj scoline 2mg/kg was given to facilitate endotracheal intubation. Anesthesia was maintained with 50% nitrous oxide, 50% oxygen and sevoflurane 2%. Supplements of inj.Vecuronium 1mg given i.v as needed. Patients ventilated on volume control mode and end-tidal CO2 maintained between 30-40 mmHg. After surgery, the patients were reversed with inj Neostigmine 0.05 mg/kg and inj Glycopyrrolate 0.01mg/kg and extubated. PONV scoring done immediately post-extubation. The patients were monitored in the recovery unit by a blinded observer for the initial two hours. During that period the incidence of nausea and vomiting was recorded every 15 minutes. The nausea and vomiting scoring was continued sixth hourly for the next 24 hours. Retching was also considered under vomiting. Incidence of emetic episodes were compared in different study groups. The patients who had even single episode of vomiting or retching anytime during the observation period were treated with a rescue antiemetic Injection metoclopramide 10 mg intravenously. Definitions10 Nausea: It is an unpleasant sensation referred to as a desire to vomit, not associated with expulsive muscular movement. Retching: When no stomach contents are expelled even with expulsive muscular efforts. Vomiting: It is the forceful expulsion of even a small amount of upper gastrointestinal contents through the mouth or nose
STATISTICAL ANALYSIS The data entered in Microsoft Excel data sheet and analyzed using SPSS 22 version software. The results were expressed as Mean±Standard Deviation (S.D.).Unpaired t test was used to compare continuous data between two groups. Chi-square test was used to compare frequencies between the two groups. Statistical significance was fixed at P value < 0.05.
OBSERVATION AND RESULTS Table 1: Demographic data
Demographic data was comparable with respect to age,sex and ASA grading in both groups
Table 2:Postoperative Monitoring
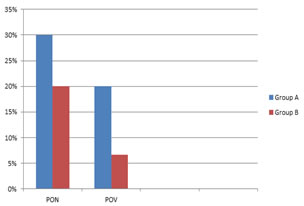
On overall comparision it was found that 9/30(30%) had nausea in ondansetron group compared to 6/30 (20%) in granisetron group and 6/30 (20%) had vomiting in ondansetron group compared to 2/30 (6.6%) in granisetron group. Table 3: Rescue Antiemetic
2/30 patients required rescue antiemetic in ondansetron group compared to 1/30 in granisetron group PON-Postoperative Nausea, POV-Postoperative Vomiting Table 4: Adverse Effects
It was observed that 3 patients in ondansetron group had headache compared to 1 patient in granisetron group.1 patient had diarrhea,1 had dizziness and 2 patients developed hiccups in ondansetron group compared to nil in granisetron group All patients in the two groups were comparable according to age and ASA grade. Incidences of nausea were 30% in ondansetron group compared to 20% in granisetron group and emetic episodes were 20% in ondansetron group (group-A), 6.6% in granisetron group (group-B). The result was both clinically and statistically significant (p<0.05)
DISCUSSION In our study we studied the effects of inj.ondansetron 4mg and inj granisetron 2mg on control of post operative nausea and vomiting in patients undergoing surgery under General Anesthesia. The patients in each group were comparable with respect to demographics, operative management, patient related factors, ASA grade and anesthetic regime. It was observed that the incidence of post operative nausea was 30% in ondansetron group and 20% in granisetron group and Incidence of postoperative vomiting was 20% in ondansetron group and 6.6% in granisetron group. This observation was statistically significant in our study. Kiran Savant, Rakshit Vijay Sinai et al.11. who compared the effects of ondansetron and granisetron for antiemetic prophylaxis in maxillofacial surgery patients observed that granisetron at an i.v. dose of 2mg to be safe, well tolerated and more effective than 4mg i.v. ondansetron for antiemetic prophylaxis in maxillofacial surgery patients receiving general anesthesia. Our results are comparable with their study. Dipasri Bhattaccharya, Arnab Banerjee12, studied the effects of granisetron 2mg iv vs ondansetron 4mg iv administered at induction of anaesthesia in patients who were to undergo laparoscopic tubal ligation under general anaesthesia and observed that the incidence of PONV was 50% with placebo, 20% with ondansetron and 7% with granisetron within 6 hours post-operatively in patients undergoing daycare gynaecological laparoscopy. So from their study they concluded that granisetron is much more effective than ondansetron to prevent PONV following daycare gynaecological laparoscopy. The results of our study are comparable with their study.P Blower, M Aapro13 in their study to compare duration of 5HT3 receptor blockade by granisetron and ondansetron, concluded that granisetron demonstrates superior efficacy to ondansetron primarily due to longer duration of action of granisetron compared with ondansetrton. Our results were comparable to their study. In our study both drugs were relatively well-tolerated and had minimal side effects. 3 of 30 patients (10%) in ondansetron group had headache where as 1 patient (3.3%) in granisetron group had headache. This was statistically insignificant. Our results were in line with studies by Figueredo and Canosa14 that showed a 7.05% incidence of headache with ondansetron. Bestas A, Onal SA et al.15 in their study on effects of ondansetron and granisetron on postoperative nausea and vomiting observed and concluded that there were no significant differences between the treatment groups in the prevalence of PONV. In their study anesthesia was induced with inj thiopental 5mg/kg and maintained with O2 (50%), N2O (50%) and isoflurane 1-3% where as in our study induction was done with inj propofol 2mg/kg and anesthesia maintained with O2(50%), N2O (50%) and sevoflurane 2%. A.Ramya Parameswari, Sivakumar Gopalswamy16 the efficacy of ondansetron vs granisetron for control of PONV in patients undergoing laparoscopic cholecystectomy and observed ondansetron (80mcg/kg) is as efficacious as granisetron (20mcg/kg) for control of PONV. In their study lower dose of granisetron (20mcg/kg) was used as compared to 2mg in our study. In their study incidence of PONV was more in patients of ondansetron group as compared to granisetron but the observation was statistically non-significant.
CONCLUSION Based on our study, we conclude that inj.Granisetron is more effective and well tolerated than inj.ondansetron in prevention of post operative nausea and vomiting in patients undergoing surgery under general anesthesia.
REFERENCES
Policy for Articles with Open Access
|
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
 Home
Home