|
Table of Content - Volume 14 Issue 1 - April 2020
Anaesthetic management and challenges in a case of left ventricular free wall rupture
Nanjappa S N1*, Naveen Singh2, Apoorva Gupta3, Madhuprakash S C4, Priyanka M S5
1Assistant Professor, 2Associate Professor, Department of Anesthesiology, Srijayadeva Institute of Cardiovascular Sciences, Mysuru and Bengaluru, INDIA. 3Assistant Professor, Department of Anesthesiology Oxford Medical College, Bengaluru, INDIA. 4Consultant in CTVS, SriJayadeva Institute of Cardiovascular Sciences and Cauvery Hospital, Mysuru, Bengaluru, Karnataka, INDIA. 5Junior Resident, Department of Anesthesiology, KIMS, Bengaluru, Karnataka, INDIA. Email: drnanj@gmail.com
Abstract Rupture of the free wall of the Left Ventricle (LV) following acute myocardial infarction is a most dreaded complication with an estimated incidence of2-4%. However, it is associated with high mortality of which inpatient mortality accounts for 51% and the remaining 49% were out of the hospital mortality. This case report discusses the challenges during peri-operative management of LV free wall rupture. Key Words: Acute myocardialinfarction, Left ventricular free wall rupture, Cardiac tamponade.
INTRODUCTION Rupture of the free wall of the Left Ventricle(LV)is a rare and most dreaded complication following an acute myocardial infarction (AMI) which accounts to 2-4% of the patients ¹. It is associated with 51% in hospital mortality and 49% out of hospitalmortality2.
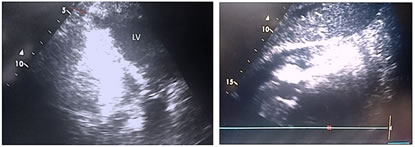
CASE HISTORY A 70-year-old hypertensive female, presented with sudden onset of chest pain and vomiting. Her ECG revealed ST segment elevation in V1-V4 with left bundle branch block. Transthoracicecho cardiogram showed rupture of LV anterior free wall with ejection fraction of a round 30% and akineticanterior segments(Fig 1 and 2). Coronary angiography revealed double vessel disease with100% ostial Left anterior descending artery occlusion and ostial obtuse marginal lesion of 80%. Diagnosed to have recent anterior wall ST segment elevation MI, severe LV dysfunction with LV clot. During her stay in the hospital, shed eveloped sudden hypotension and tachycardia, neck vein distension, puls usparadoxus, quiet heart sounds, elevated CVP with steep X descent on the third day of AMI. Transthoracic echocardiography revealed LVFW rupture, blow out variety, severe LV dysfunction, ejection fraction of 30%, kineticapico-anterior, apico inferior, mid and distal septum with cardiac tamponade. She was intubated emergently after administration of 50 mc gfentanyl, 0.5mg midazolam, 50mg ketamine, and 50 mgrocuronium. Injection dobutamine10mcg/kg/min and injNTG0.5 mcg/kg/min infusion were initiated. She was shifted to Operation Theater for emergency Dors procedure. Un fractionated heparin was administered to achieve an Activated clotting time > 480 seconds and the patient was subjected to Cardiopulmonary bypass (CPB)(Fig 3). LVF Wrepair with LAD revascularization was performed with 158 minutes of CPB duration (Fig 4).
Figure 1 Figure 2 Figure 3 Figure 4 Figure 1: Transthoracic echocardiography apical four chamber view showing rent in anterior wall; Figure 2: Transthoracic echocardiography subcostal view showing significant pericardial effusion; Figure 3: Surgical image showing anterior LV free wall rupture; Figure 4: Diagram depicting surgical patch closure of LV free wall rupture
Initial attempt to wean from CPB was unsuccessful prompting the team to insert IABP before attempting to wean from CPB. Patient was weaned from CPB successfully with IABP and in otropesinj. Adrenaline 0.08 mcg/kg/min and inj. Dobutamine 10 mcg/kg/min. Protamine was administered to neutralize heparin and hemostasis was achieved. Post-operative transthoracic echocardiography revealed an ejection fraction of 35% with no significant pericardial collection. Patient was extubated36 hours after shifting to recovery ICU. IABP was weaned on second post-operative day and eventually inotropes were also weaned.
DISCUSSION: Free wall rupture of LV is the third leading complication and second most common cause of death after myocardial infarction3. Following AMI, Cardiogenic shock and LVFWR are the major causes of death, resulting in 66% of deaths due to AMI.4 The most feared complication of myocardialin farctionis that of cardiac rupture accounting for up to 20% of deaths associated within farction.4 Free wall rupture may occur from few minutes to few months most commonly appears on the 4th or 5th day after AMI. Risk factors include females, hyper tensives without hypertrophied ventricle, insufficient collateral network and with delayed thrombolysis.2 Anterior wall ruptures are relatively more common as the anterior infarcts are frequent, but recent studies indicate that the rupture of lateral or posterior wall are not uncommon.2 There are various classifications for free ventricular wall rupture. O Rourkes classified as acute, sub-acute and chronic with pseudo-aneurysm. Depending on the type of cardiac rupture post AMI, it is classified as stuttering ruptures and blow out variety2. Further, LVFW rupture is also classified as early and late occurring 48 hours before and after acute MI respectively 5. Sudden bradycardia with hypotension and loss of consciousness should alert the clinician, an impending rupture 6. In a patient with persistent chest discomfort following AMI and signs of pericardial tamponade like hemodynamic instability ,raised jugular venous pressure, pulses paradoxus, muffled heart sounds, diastolic equalization of CVP, PAP and LAP, CVP trace shows steep X and blunted Y descent and EMD should rouse a suspicion of Ventricular free wall rupture5,6,7,8. Severity of disease can be depicted by ECG findings. Electro mechanical dissociation and bradycardia constitute the characterization of acute rupture, ST elevation of at least 1mm in affected leads. It is difficult to differentiate between rupture and rein farction with ECG changes and cardiac enzymesalone2. Hence ECHO plays a pivital role in differentiating this diagnostic dilemma, as management of these conditions differ. The most common echo finding in patients with sub acute ventricular wall rupture is pericardial effusion2. Reports shows subacute LVFWR treated successfully with medical management. Percutaneous Intra-pericardial Fibrin-glue inj. Therapy (PIFIT)has been tried as a part of medical therapy and found to be quite effective 9. Surgical procedure still remains the definitive approach for LVFW rupture 5. Treatment strategy varies in case of LVFW rupture based on the hemodynamics of the patient. Hemodynamically unstable patients may require IABP (intraaorticballoon pump), inotropic support, pericardiocentesis. However stable patients have to under gocoronary angiography. Striking the right balance of LV preload, afterload and LV contractility is challenging in maintaining hemodynamics of the patient as increased contractility and or volume could causetension on the sutures of the LV wall. Percutaneously IABP inserted into descending aortaupto just distal to left sub clavian artery via femoral artery. Ballooninflation is during diastolic period, which increases coronary blood flow thus increases perfusion pressure in coronary artery. Balloon deflation abruptly, before the next systolic ejection from the heart decreases the after load by offering no resistance to aotic valve opening. This results in dual benefits of improving coronary perfusion pressure by increasing coronary blood flow and decreasing afterload to the LV. Cardiac output can increase by 20% to 30% and decreases the after load by 15% with ideally functioning IABP 10
CONCLUSION Recognition of LVFW rupture with cardiac tamponade requires meticulous and continuous monitoring. Timely intubation, mechanical ventilation, inotropic support and immediate surgery, IABP usage plays a pivotal role for the favorable outcome of the patient. Transthoracicecho cardiography is a useful tool perioperatively for survival benefit.
REFERENCES
Policy for Articles with Open Access Authors who publish with MedPulse International Journal of Anesthesiology (Print ISSN:2579-0900) (Online ISSN: 2636-4654) agree to the following terms: Authors retain copyright and grant the journal right of first publication with the work simultaneously licensed under a Creative Commons Attribution License that allows others to share the work with an acknowledgement of the work's authorship and initial publication in this journal. Authors are permitted and encouraged to post links to their work online (e.g., in institutional repositories or on their website) prior to and during the submission process, as it can lead to productive exchanges, as well as earlier and greater citation of published work.
|
|
 Home
Home