|
Table of Content - Volume 14 Issue 1 - April 2020
Intra operative allowable blood loss: Estimation made easy
Kulkarni Vandana Sharashchandra1, Sajjan Prashant Shivaraj2*
1,2Associate Professor, Department of Anaesthesiology, Aarupadai Veedu Medical College, Kirumampakkam, Puducherry INDIA.
Abstract Background: Estimation of blood loss during surgery is not accurate due to lack of practical means and methods. This leads to either underestimation or over estimation of blood loss which leads to wrong decision regarding blood transfusion in many cases. Method - It is a prospective study conducted in 100 patients undergoing surgeries. Here patient’s allowable blood loss was calculated based on their weight and preoperative hematocrit. Calculated number of mops were given during the surgery based on the absorption capacity of mops and allowable blood loss. When all the mops were fully soaked and used by the surgeon then it was assumed that the patient lost allowable blood loss. If further mops were used then decision was taken regarding the need of blood transfusion. Result: In 47 patients all the mops were used but transfusion was not required. In 17 patients extra mops were used and blood transfusion was initiated. In 36 patients all mops were not used. Post operative hematocrit (after 48 hours) was compared with preoperative hemoglobin. The result (p<0.05) was significant. Conclusion: Use of Calculated number of intra-operative mops usage based on allowable blood loss will help in alerting the operating team regarding the blood loss and need for blood transfusion. Key Words - Allowable Blood loss (ABL),Blood Volume, Hematocrit.
INTRODUCTION Assessment of blood loss during surgery is an integral part of anaesthesia practice. However no accurate and practical methods or tests are available for measuring blood loss during surgery. In intra operative period the decision to transfuse blood is taken either once the hemodynamic of the patients gets compromised or based on individual judgment of the surgeon or the anaesthesiologist1 Many times the decision to transfuse blood is taken at the end of the surgery by counting the mops and pads. In many cases the actual blood loss is not calculated only. Blood is transfused depending on the visual blood loss or clinical condition of the patient which many times lead to unnecessary transfusion or delayed decision in transfusion2-3. Accurate methods are not economical and fast. In many hospital set up the other measures of calculating blood loss are not available due to financial issues and they mainly have to rely on rough visual estimation of blood loss3. Many a times because of the denial of significant blood loss by the operating team and/or delay in recognition of the significant blood loss there are potential chances of patient increase morbidity and mortality 4-6.This in time assessment also prevents the time wastage in procuring blood from the blood bank. This article is an attempt to prevent unnecessary blood transfusion and at the same time alerting the operating team when they have crossed the allowable blood loss limit.
METHOD It is a prospective study in which 100 adult patients of either gender undergoing major surgeries were included. The operating anaesthesiologist was provided the details of the study. The anaesthesiologist was provided the details like age, sex, weight and initial hematocrit of the patient along with the proforma before the surgery. Based on the details allowable blood loss was calculated for the patient pre-operatively. Based on the allowable blood loss, calculated number of mops and gauzes were made available to scrub nurse for use during the surgery. The scrub nurse was instructed to take calculated number of mops and gauzes and inform when all the given mops and gauzes are soaked fully with blood before taking new sets of mops and gauzes. The floor nurse was asked to release new set of mops and gauzes only after informing the anaesthesiologist. To maintain uniformity same size of mop and gauze by a single company were used for all patients. Comparison of pre-operative and post operative hematocrit (after 48 hrs) was done to know whether the correlation between the blood loss and hematocrit is correct. Inclusion Criteria
Exclusion Criteria
Special Instructions The scrub nurse was given instructions not to squeeze, reuse or discard the mops and gauze allotted for the surgery. The new lot of mops or gauze were given to the scrub nurse after informing the anaesthesiologist.
RESULTS In our study for 36 patients all the mops were not used or the surgery was completed within the allotted mops and there were few mops or gauze left unused after surgery. For 47 patients all the allotted mops and gauzes were used but, they did not require blood transfusion. 17 patients not only utilized the allotted mops but also required new set of mops. These 17 patients were transfused blood as the allowable blood loss was crossed. In these 17 patients blood loss was discussed and it was agreed by both operating surgeon and anaesthesiologist regarding the amount of blood loss and decision of blood transfusion. Table 1: Number of Mops used and Blood transfusion
Picture 1: Fully soaked Mops Picture 2: Size 30 X 30 cm
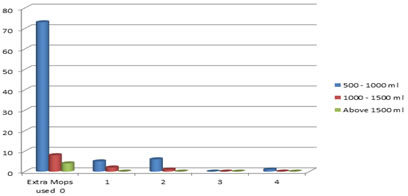
Table 2: Blood loss and Extra Mops used
Chart 1: Blood loss and Extra Mops used
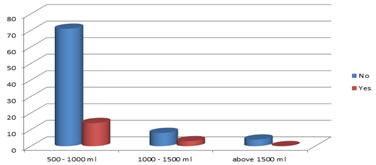
Table 3: Blood loss and Blood transfusion
Chart 2: Blood loss and Blood transfusion In our study pre-operative mean hematocrit is 34.514 (SD 1.93) and post-operative hematocrit is 31.35 (SD 1.68) with p value 0.005, which is significant. Table 4: Comparison of Hematocrit
In 47 patients even though all the mops were used blood transfusion was not done as the allowable blood loss was not exceeded. In all the 17 patients where blood loss exceeded allowable blood loss operative team was alerted as soon as last mop was used, which helped in initiation of blood transfusion within time. Thus it helped both the surgeon and anaesthesiologist in taking the decision regarding the blood loss and blood transfusion.
Calculation of allowable blood loss and Mop/ Gauze count It is imperative to know the normal hematocrit and blood volume to calculate the allowable blood loss. There are few methods for calculation of blood loss like gravimetry, photometry and serial Hb measurement. These methods have limited use in practice because of unavailability and time consumption5,7. Hence visual observation is the most commonly used method for estimating blood loss. Normal Values: Hematocrit: Healthy Adult Male – 42 – 52 % Healthy Adult Female – 37 – 47 % Blood Volume: It varies with age, gender and weight of the person .Table 5: Normal Blood volume based on age and gender8-11
Transfusion trigger 12-15 The commonest indication for blood transfusion is based on “10/30”rule which stipulates that patients Hb should be maintained at or above 10 g/dl or hematocrit at or above 30 %. Calculation of Allowable blood loss16-21 Allowable blood loss (ABL) = EBV X Hi (Initial hematocrit) – Hf (Final hematocrit) Hi (Initial hematocrit) Step 1: Calculate the Estimated Blood Volume (EBV) EBV = Weight (kg) X Blood volume (age and gender) Step 2: Decide the tolerated decrease in hematocrit from initial hematocrit by the patient.
Estimating Blood loss22-24 One of the commonest methods of blood loss estimation is by its absorption into the mops, pads or gauzes used during the surgery. The dry mops / pads used during surgery absorb blood depending on their sizes. 4 X 4 cm = 10 ml 30 X 30 cm = 100 ml So, based on this if we calculate and know the amount of blood loss that can be allowed for the patient for particular surgery we can calculate and take the precise number of mops, pads and/ or gauze. Let’s understand this with an example 50 kg female with pre-operative hematocrit of 45% How much is the allowable blood loss for the final or the targeted hematocrit of 30%? What is the number of mops / gauzes to be used intra-operatively? Step 1. EBV = 50 (weight in Kg) X 65 (Blood volume in females) EBV = 3250 ml. Step 2. Allowable blood loss (ABL) = EBV X (Hi – Hf) Hi ABL = 3250 X (45 – 30) 45 ABL = 1083 ml Here the allowable blood loss is 1083 ml, round figure 1100 ml. Number of mops that can be taken by operating team 11 mops of (30 X 30) cm = 1100ml or Combinations – 10 mops of (30 X 30) cm = 1000ml + 10 Gauze of (4 X 4) cm = 100 ml and so on depending on the surgery and surgeons requirement. When all the calculated mops and gauzes are blood soaked the patient has lost 1100ml blood and team can decide regarding the blood transfusion. Even based on the surgery and surgeons requirement the sizes of mops and gauzes can be used in combination to reach 1100 ml.
DISCUSSION In any major surgery blood loss is a common factor. It is the responsibility of the operating team to identify the blood loss, prevent further bleeding and replace the blood volume as soon as possible. In order to make a decision of blood transfusion one can calculate the allowable blood loss preoperatively and based on that, calculated number of mops or combination of mops and gauzes can be taken by the operating team. When all the calculated mops or combination of mops and gauzes are used and are soaked with blood it means that the target allowable blood loss has reached. Whenever surgeon asks for next set of mops or gauzes it will alert the operating team and proper decision regarding the transfusion can be taken. This is an effective, easy and practical method of estimating the blood loss during the surgery. The calculated mops or combination of mops and gauzes can be taken by the operating team. When all are blood soaked and used, it will alert the operating team regarding the blood loss. The decision of blood transfusion can be taken on table, immediately, and without waiting for the lab confirmation or clinical signs and symptoms. In some institutes where getting blood takes considerable amount of time. This simple alert will help them to get blood within time thus preventing morbidity and mortality of patients. If the operating team has not used all the calculated mops and gauzes then patient has not lost enough blood to be considered for blood transfusion. This also prevents the unnecessary blood transfusion to the patient. However this method is not accurate as soakage of mops is subjective. Mixing of fluid, secretions and irrigation fluids with blood will erroneously give the feeling of mops soaked with blood. Blood collected in the suction apparatus and bloods soaked into the drapes are not calculated. All these may lead to the misinterpretation of blood loss. Nevertheless, the above method if used vigilantly can help the operating team to make decision regarding the blood transfusion well in time. It will also help to avoid unnecessary blood transfusions and hazards associated with it.
CONCLUSION Use of pre calculated number of mops based on the allowable blood loss will help to alert the operating team regarding the blood loss and help in the decision making regarding blood transfusion.
REFERENCE Ganesan Ganesan, Ram , Perumal, Suresh , Phagal, Varthi, Vijayaraghavan ; Surgeons often underestimate the amount of blood loss in replacement surgeries; Chinese Journal of Traumatology Volume 17, Issue 4, August 2014, Pages 225-228.
Policy for Articles with Open Access Authors who publish with MedPulse International Journal of Anesthesiology (Print ISSN:2579-0900) (Online ISSN: 2636-4654) agree to the following terms: Authors retain copyright and grant the journal right of first publication with the work simultaneously licensed under a Creative Commons Attribution License that allows others to share the work with an acknowledgement of the work's authorship and initial publication in this journal. Authors are permitted and encouraged to post links to their work online (e.g., in institutional repositories or on their website) prior to and during the submission process, as it can lead to productive exchanges, as well as earlier and greater citation of published work.
|
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
 Home
Home