|
Table of Content - Volume 15 Issue 3 - September 2020
Hemlata Kamat1, Vaibhavi Hajariwala2*, Smiral Desai3
1Professor, 2Associate Professor, 3Resident, Department of Anesthesiology, Pramukhswami Medical College, Shree Krishna Hospital, Karamsad, Anand, Gujarat, INDIA. Email: vaibhavih35@gmail.com
Abstract Background: Deposition of local anesthetics at the intersection of the subclavian artery and first rib (corner pocket) injection technique under ultrasound guidance results in a higher efficacy. Aim of the study is to evaluate the efficacy of block in terms of time taken to perform block, onset and duration of sensory block and motor block, quality of muscle relaxation and surgeon and patients’ satisfaction. Method and Materials: Prospective observational study was performed in Shri Krishna Hospital Pramukhswami Medical College, Anand, Gujarat. 40 patients with ASA I-III, ages from 18-70 years with BMI between 18-30 kg/m2 posted for surgery distal to mid humerus. The brachial plexus was located by using ultrasound 7-10 MHz linear probe. Brachial plexus was blocked by using two-point injection technique. First injection was given in corner pocket formed by the subclavian artery and the 1st rib (7 O’clock position in relation to subclavian artery) and the second injection was given in superior pocket (11 O’clock position in relation to subclavian artery) by using in plane technique. The onset of sensory and motor block was assessed using pin prick method and modified Bromage scale. Total procedural time, duration of sensory and motor block and surgeon and patient satisfaction were also noted. Results: The mean performance time for procedure was 14.60±2.74 minutes. The mean onset time for sensory and motor block was 11.09±2.47 minutes and 17.69±3.40 minutes respectively. The mean duration of motor and sensory block was 196.95±40.15 minutes and 279.63±102.90 minutes respectively. Out of the 40 patients there were 5 failures out of which 3 were given general anaesthesia and other 2 required supplementation of block by axillary route. Conclusion: The result of our study suggested that under sonographic guidance with two point injection technique the onset time for motor and sensory block is reduced but total procedure time is prolonged with a good success rate in view of patient and surgeon satisfaction. Key Word: Supraclavicular brachial plexus block.
INTRODUCTION Supraclavicular brachial plexus block is nicknamed as “spinal anaesthesia” of the arm because block is dense due to tight arrangement of nerves here.[8] A real milestone in regional anaesthesia was the introduction of ultrasonography with accurate nerve and needle position. It should be possible to avoid direct injury to nerves and vascular structures. There have been various ultrasound-guided approaches described for supraclavicular brachial plexus block.13,15,16 In 2009 Fredrickson MJ et al.13 described corner pocket at the inferior lateral aspect of the subclavian artery. Most of the time this territory is spared and resulting in ulnar sparing with peripheral nerve stimulator guided block. Tran DQ et al.17 proved in their study that injection of local anesthetic in the corner pockets with the help of USG (ultrasonography) results in more successful supraclavicular block. We have studied effectiveness of two point injection technique around subclavian artery in coronal plane with in line approach from lateral to medial direction in order to avoid pneumothorax.9
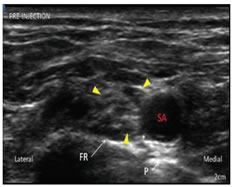
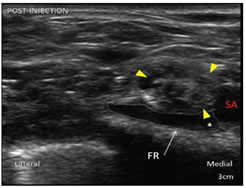
MATERIALS AND METHODS This prospective descriptive study was approved by institutional ethical committee. Informed written consent was obtained from all the patients. A total of 40 patients of ASA grade I-III, ages from 18-70 years with BMI between 18-30 kg/m2 posted for surgery distal to mid humerus, with the surgical duration ≥ 1 hour were included in study. Patient who were uncooperative, have history of coagulopathies, have known allergy to local anesthetics, have neuropathies, cardiac and respiratory ailments were excluded from the study. All patients underwent thorough preoperative examinations and were instructed about the methods of anaesthesia and the methods of eliciting sensory and motor blockade. Patients were kept nil per-oral according to ASA guidelines. In preoperative room base line vitals were recorded. Intravenous line was secured on non-operating arm and injection Ringer lactate was started. In operating room patient was placed supine and standard monitors were applied (ECG, NIBP, SpO2). All patients were premedicated with IV Ranitidine 1mg/kg and injection midazolam 0.5 mg. Oxygen was administered by face mask. All essential equipments and materials were arranged on a sterile trolley. For performing the block, the ultrasound machine and sterile trolley were arranged on the side to be blocked. Optimization of USG variables like scanning mode, depth of field and gain were adjusted before the start of the procedure. Patients were positioned supine with head end elevated , head turned towards the opposite side and the arm to be blocked was kept adducted by the side of patient. Sterile painting and draping were done. USG linear probe of 7-10 MHz was used to locate the brachial plexus. After applying sterile jelly the probe was moved from cephalic to caudal direction to bring subclavian artery in the center of the screen to a point where nerve plexus was situated lateral to artery (Figure 6). A 20G 100mm Quinckie spinal needle was inserted from lateral to medial direction by using in plane technique so that needle remains visible at any point of time and injury to pleura can be prevented. Combination of Inj. Bupivacaine 0.5 % and Inj. Lidocaine 2 % was used. Total 25 ml of local anaesthetic solution was taken (15 ml of Inj. Bupivacaine and 10 ml of Inj. Lidocaine). Once the needle was between brachial plexus and artery, half of the solution of local anesthetic was injected first in corner pocket, i.e. at 7’O clock position of subclavian artery and remaining half of the local anesthetic solution was injected in the superior pocket i.e. 11’O clock position of the subclavian artery after redirecting the needle (Figure 7). Sensory block was assessed by loss of pin prick sensation. 0 is no loss of sensation and 1 is complete loss of sensation in the arm. Motor blockade was assessed by modified Bromage scale.
Following parameters were recorded Tp-Time to perform block. T1- Time of real time imaging of subclavian artery. T2- Time of deposition of drug at 11’0clock position. Tp = T2-T1 Ts- Time to achieve sensory block. T3- Time to deposit drug at 7'0clock position. T4- Complete loss of pin prick sensation. Ts = T4-T3 Tm- Time to achieve motor block. T7- Time at which Bromage scale was 2 Tm=T7-T3 Duration of motor blockade and sensory block was noted; patient and surgeon satisfaction levels were also noted. Successful block was defined in which patient allowed surgeon to do the surgery. If patient still experienced pain or showed discomfort after 20 minutes of block, supplementation by axillary route was done and volume of local anaesthetic drug required were noted. Total failure of the block was considered, when there was no satisfactory effect of the block even after 20 minutes of supplementation by axillary route such patients were given general anesthesia. Patient and surgeon satisfaction level were noted as excellent, satisfactory and unsatisfactory. The patients were followed post operatively and vital parameters were observed till first dose of analgesic required (VAS score = 4). All the cases were performed by the same anesthesiologist. All the data were recorded and obtained by the personnel other than performer of the block.
STATISTICAL ANALYSIS It was done by descriptive analysis using SSPS version and mean time of onset of sensory and motor blockade, mean duration of motor and sensory block with standard deviation (SD) were calculated.RESULTS Out of 40 patients, 25 patients were Male and 15 were female (Table I).
Table I: Physical characteristics of Patients
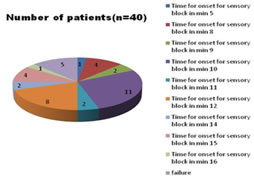
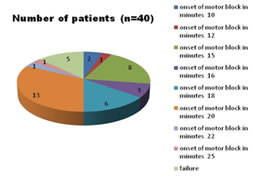
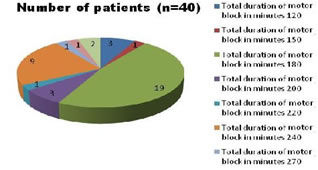
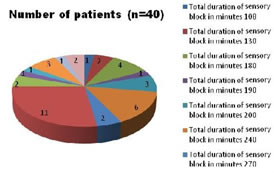
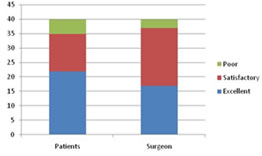
The mean performance time for procedure in our study was 14.60±2.74 minutes. Maximum time to perform the block was 20 minutes in one case and minimum time to perform the block was 10 minutes in 2 cases. The mean onset time for sensory block was 11.09±2.47 minutes and mean onset time for motor block was 17.69±3.40 minutes (Figures 1 and 2). The mean duration of Motor block was 196.95±40.15 minutes. Mean duration of Sensory block was 279.63±102.90 minutes (Figures 3and 4). Quality of block was graded by patient and surgeon (Figure 5). Figure 1 Figure 2
Figure 3 Figure 4 Figure 1: A Pie Chart showing frequency distribution for time of onset of sensory block; Figure 2: A Pie Chart showing frequency distribution for time of onset of motor block; Figure 3: A Pie Chart showing frequency distribution for time of total duration of Motor block; Figure 4: Pie chart showing frequency distribution for time of total duration of Sensory block Figure 5: A Bar Diagram showing proportion for patient and surgeon satisfaction Figure 6 Figure 7 Figure 6: View on the USG screen before injection of local anesthetic drug; Figure 7: Postanesthetic injection: Right supraclavicular brachial plexus (yellow arrows) Brachial plexus = yellow arrows. FR = first rib, SA = subclavian artery, P = pleura, * = corner pocket. Local anesthetic (dashed lines) had been deposited in corner pocket (*). Note the nerves now appeared to be floating on the injected anesthetic drug. FR = first rib, SA = subclavian artery.
DISCUSSION Many studies have been done that compares ultrasonography (USG) with peripheral nerve stimulator (PNS) technique for supraclavicular brachial plexus block in upper limb surgeries and in conclusion ultrasonography technique is well versed as compared to PNS technique.21Efficacy, safety and patient as well as surgeons’ satisfaction level are enhanced by using USG technique for Supraclavicular block and the same was concluded by K.Gammo et al. in their study.22 Use of high frequency USG probe along with in plane needle insertion and two-point injection of local anaesthetic solution significantly improves the efficacy of the block and provides much needed safety by reducing the chances of pneumothorax and vascular injuries. The latest description of USG guided supraclavicular block by Tran DQ et al.17 aims to deposit local anesthetic into corner pocket i.e. at the inter section of subclavian artery and first rib. This results in higher efficacy and higher success rate. In order to bring more effectiveness and improve the safety and success rate of the block we inject local anesthetic into corner pockets as shown by Chan VW et al.3 and Tran DQ et al.17 in their studies. With this technique of depositing local anesthetic into corner pocket, it seems reasonable to expect successful block with lower volume of anesthetic. In 2009 O’Donnell BD et al.6 estimate the minimum effective volume of 2% lidocaine in USG guided brachial plexus block. We have used 25 mL of local anesthetic containing mixture of injection bupivacaine 0.5% and injection lidocaine 2%. We were successful in achieving satisfactory block without ulnar sparing with low volume of drug. The mean onset time for sensory block as per our study was 11.09 minutes with standard deviation of 2.47 minutes. The maximum observed onset time was 16 minutes and the minimum observed onset time was five minutes. The mean onset time for motor block was 17.69 minutes with a standard deviation of 3.40 minutes. The maximum observed onset time was 25 minutes and minimum was 10 minutes. Tran DQ17 concluded that onset time for sensory blockade was shorter in their studies with two point injection technique. Amr M.A. Sayed et al.15 did not found any difference in onset of sensory and motor blockade between two point and single point injection. The quality of imaging can be quite variable among patients with much indistinct anatomy seen on USG screen and it is challenging as it is always an assumption that the individual performing the block is able to maintain perfect alignment of the needle with the probe. But it is not so in each and every case. In our study we have to redirect the needle to inject the local anesthetics at 11 O’clock position around the subclavian artery, which requires time and precision. Ultrasound visibility of needle is a critically important factor for success of the block, so we used 20 gauze, 100mm spinal needle for the supraclavicular brachial plexus block. Schafhalter-Zoppoth I et al.19 compared the visibility of 17G-22G Quinckie spinal needle on USG screen. In our study the tip of the needle was continuously under sonographic view, vascular puncture or nerve injury were preventable in spite of sharp and bevelled tip. Out of 40 patients 35 patients did not require any supplementation of local anesthetics or any sedation. Two patients required supplementation of total 10 ml of local anaesthetic via axillary route. 2 patients required general anesthesia as there was no loss of sensations even after 20 minutes of performing the block. In this study we have also observed the total duration of sensory and motor blockade and requirement of the rescue analgesics. The mean duration of Motor block was 196.95 ±40.15 minutes and mean duration of sensory block was 279.63 ± 102.9 minutes. The surgeon graded the block as excellent in 17 cases, satisfactory in 20 cases and unsatisfactory in 3 cases. In our study success rate of block was 92.5%, however in spite of ultrasound guidance the rate of success is not hundred percent. The procedural time for performing the block was 14.6 minutes with standard deviation of 2.74 minutes. Arab, Samer A et al.16 compare sensory block success rate of single injection versus triple injection, they found that the multiple injection has faster onset but time to perform the block increases. As per patient’s satisfaction, out of 40 patients 22 patients opined the experience with the block as excellent, 13 patients opined this experience as satisfactory and 5 patients were not satisfied with the block. We did not encounter any other potential complications like pneumothorax9, horner syndrome, phrenic nerve block12, nerve injury or puncture of the blood vessels. Use of Colour Doppler to identify the vessels, real-time imaging on USG screen as well as in plane needle insertion technique helped us to prevent such complications.
Table 2: Comparison of different studies :
LIMITATION OF THE STUDY Though ultrasound is an excellent learning tool it cannot guarantee hundred percent success rate of block, but one can learn and continuously improve their technical skill which is necessary for ultrasound guided regional anaesthesia. This study aimed for learning of the post-graduate students and performed by them only under the guidance of skilled anaesthetist. Therefore, the success rate of the block in our study was slightly less than other studies and results may or may not be generalized.15,16,17,23 Even though the block was performed by the post- graduate student the incidence of complications were nil due to the précised needle insertion technique.
CONCLUSION The supraclavicular brachial plexus block is an extremely comprehensive anaesthesia for the upper limb surgeries. The relatively common and severe complication of this technique had resulted in transient decrease in its popularity. This study was undertaken on the basis that injecting local anaesthetic drug at two corner pockets of subclavian artery under sonographic guidance affects the quality and success rate of the block. This could have implications for daycare upper limb surgery allowing more scope for regional anaesthesia and assuring the maximum success rate with the use of lesser volume of local anesthetics resulting in minimizing the rate of complications related to the procedure and drugs.
REFERENCES
Policy for Articles with Open Access
|
|
 Home
Home