|
Table of Content - Volume 15 Issue 3 - September 2020
Comparative study of general anaesthesia and spinal anaesthesia in severe pre-eclampsia patients undergoing emergency caesarean section in tertiary care centre
Shailendra A Satpute1, Ganesh K Nikam2, Shailendra D Chauhan3, Abhimanyu Tarkase4, Sudhir Deshmukh5
{1Junior Resident 3,2Associate Professor,3Professor 4Associate Professor, Department of Anaesthesia} {5Professor, Department of Surgery} SRTR Medical College Ambajogai, Beed- 431517 Maharashtra, INDIA
Abstract Background:Both spinal (SA) and general anaesthesia (GA) are commonly used for operative management of pre-eclampsia parturients. The present study was undertaken to compare the effect of GA versus SA on severe pre-eclamptic parturient undergoing emergency caesarean section. Method: A total of 100 patients were enrolled and divided into two equal groups. Group S received SA with 0.5% bupivacaine heavy and group G received GA with inj. Thiopentone 3- 5mg/kg and Inj. Succinylcholine 1.5-2mg/kg. The clinical findings, socio-demographic factors were noted, all relevant investigations were done. The data collected was analyzed to compare the effect of GA versus SA. Results: The demographic data excluding weight, airway parameters, gestational age, speed of onset and oxygen saturation were comparable between two groups, (P > 0.05).The mean baseline haemodynamic parameters of all mothers were high, although in the acceptable range for preeclampsia (p>0.05) while the mean blood pressure (SBP, DBP and MAP) of mothers in group G was higher than group S throughout the intraoperative period, (p<0.05). The mean birth weight of neonate in group S was 2.65±0.25 kg and in group G was 2.58±0.25kg, (p=0.16). The difference in APGAR score was statistically significant (p=<0.05). Patients in group S were awake throughout procedure and 100% patients from group S did not have pain. Overall difference in maternal and neonatal complication was not significant, (p=0.7).Only 1 maternal death observed in group G. Conclusion: From the results of present study, it can be concluded that the SA is far better than GA in severe pre eclamptic mothers. Key Words: Pre-eclampsia,Parturients, Bupivacaine, Thiopentone, Succinylcholine, Thyromental distance, Mallampatti grade, Haemodynamics
INTRODUCTION Pre-eclampsia is disorder of pregnancy characterized by onset of high blood pressure and often significant amount of protein in the urine. The condition begins after 20 weeks of pregnancy. Severe features of preeclampsia include any of the following findings: Systolic blood pressure (SBP) of 160mm Hg or higher, and/or diastolic blood pressure (DBP) of 110mm Hg higher on 2 occasions at least 4 hours apart on bed rest1. Women with severe pre-eclampsia have an increased rate of caesarean section consequent upon high incidence of IUGR, fatal distress and prematurity and anaesthesia remains a challenge as parturients may present to labour and delivery unit with or without a prior diagnosis of preeclampsia2. Recently, spinal anaesthesia (SA) has been recognized to have a place in operative management in pre-eclampsia parturients because it is more practical, has faster onset, minimizing polypharmacy and with fewer complications [3]. A concern is raised that SA is unsuitable for pre-eclamptic patients as there is potential for profound hypotension that could further deteriorate an already potentially compromised newborn and worsen neonatal outcome whereas, there are reports that states that patients with the severe pre-eclampsia experiences less hypotension during SA than healthy parturients4. Minimal hemodynamic effects from the SA in healthy pregnant females is demonstrated by using appropriate dose of bupivacaine (10 mg bupivacaine) but this has not been sufficiently investigated in pre-eclamptic toxaemia5. General anaesthesia with rapid sequence intubation is considered over RA when there is an immediate threat to the mother or fetus3. In pre-eclamptic females GA is problematic due to difficultly in airway and hemodynamic consequences of the laryngoscopy and the tracheal intubation6. The use of GA for CS has declined while that of spinal techniques has increased. Moreover, GA is the quickest anaesthesia method in an emergency; it may be indicated when the woman refuses regional techniques,in failed regional attempts or when regional is contraindicated such as in coagulopathy or spinal abnormalities7. Despite the paradigm shift toward SA, GA is still commonly administered in our facility for some specific indications.Therefore present study was aimed to evaluate and compare the safety and the maternal and neonatal outcomes in patients who had emergency CS under SA compared with those who had GA.
MATERIALS AND METHODS This observational study was carried out in the Department of Anaesthesia at Tertiary Care Hospital from December 2017 to October 2019. A total of 100 pregnant females with severe pre-eclampsia (BP>160/110 mmHg, proteinuria>3+), gestational age >34 weeks, ASA grades 2 and 3, age 20-40 years, weight > 40 kg and < 80 kg and platelet count > 75000 were included in the study. Patients were randomly divided in two groups, Group S for spinal anaesthesia and Group G for general anaesthesia having 50 patients in each group. Before starting the study Institutional Ethical Committee approval was obtained and written informed consent was taken from all the patients. Patient’s refusal, patients with coagulopathy, peripheral neuropathy, history of drug allergy, severe anaemia of < 6gm%, patients with diabetes, thyroid disorder, seizure disorders, renal impairments and co-morbidities (cardiac disease, pulmonary disease, neurological deficits) were excluded from the study.Data was collected by using a pre designed questionnaire which consisted of standard questions related to clinical condition, socio-demographic factors, addiction among family members were interviewed. In addition, questions related to past and present medical history and health seeking behaviour were also studied. Clinical examination, diagnosis, investigations details of previous operative procedure was done.All patients received IV infusion of 500 ml of lactated Ringer’s solution prior to procedure. The volume of fluids administered to patients with severe preeclampsia was not decreased because of expected intravascular volume contraction. During caesarean section, all patients were in the supine and 15°–20° left uterine displacement position. In Group S, Spinal anaesthesia (n=50) was administered in sitting position using 23 Quincke needle. A hyperbaric solution of 0.5% Bupivacaine heavy (10 mg) was injected intrathecally (L2-3 or L3-4). The upper sensory level was checked using loss of cold sensation, motor level of spinal anaesthesia is checked with Bromage scale. In Group G, for General Anaesthesia (n=50), a standardized induction of general anaesthesia was performed (5 mg/kg inj. Thiopentone and 2 mg/kg succinylcholine for rapid-sequence intubation). Maintenance of anaesthesia was with 50% nitrous oxide in oxygen and 1-2% end-tidal sevoflurane. Patients were ventilated to a target end-tidal carbon dioxide concentration of 30–40 mmHg, using a circle system with fresh gas flows of 5 L/min until delivery. Neuromuscular blockade was maintained with vecuronium 0.08 mg/kg. Oxytocin 5 IU intravenously administered after the delivery of baby. Thereafter, a continuous infusion of oxytocin was administered (10 IU/l, at 60– 100 ml /h). Blood pressure for all enrolled patients was recorded 15 times, starting from the time zero [3 min before induction (GA) or before puncture (SA)], until 60 minutes after induction/puncture. During the procedure (caesarean section), maternal BP and HR were recorded after the induction/puncture as follow: at 2.5 min intervals from the spinal injection for the first 10 min and then at 5 min intervals until the end of the surgery.The data was collected in terms of demographic profile (age , weight, ASA Grade), airway parameters (Mallampatti grade, thyromental distance, cervical and neck stability), post-operative sedation with Ramsey Sedation Score (RSS),visual analogue scale (VAS), oxygen saturation, maternal haemodynamic changes and complications, birth weights of neonates and neonatal complications along with APGAR score at 1 min and 5 min.
Statistical analysis Results of continuous (quantitative data) measurement were presented on Mean ± SD (min-max) and result on categorical (qualitative data) measurements was presented in percentage and proportions (%). Comparison of qualitative variable was analyzed by chi-square test. Wherever necessary between groups, comparison of quantitative variables was analyzed by independent student t test according to distribution. A p value of 0.05 was taken as level of significance. Data analysis was done open epi version 2.3.1.
RESULTS A total of 100 severe pre-eclamptic parturient were studied during a period from December 2017 to October 2019. The demographic data (except weight) were comparable and found no significant difference between two groups, (>0.05) as shown in table 1. Table 1: Demographic profile of the study population
Airway (Mallampatti grade, thyromental distance) and obstetric parameters (Gestational age, speed of onset, oxygen saturation) were comparable among two groups. There was no significant difference with p value >0.05 in all parameters as depicted in table 2. Table 2: Comparison of airway and obstetric parameters between two groups
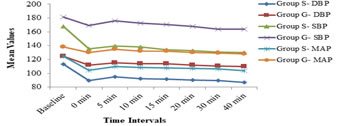
The mean baseline haemodynamic parameters of all mothers were high, although in the acceptable range for preeclampsia and found no statistically significant differences (p>0.05) while the mean haemodynamic parameters of mothers in group G was higher than group S throughout the intraoperative period. Changes in maternal haemodynamic in patients studied under group S and group G shows statistically significant difference (p<0.05), (Figure 1).
Figure 1: Maternal hemodynamic parameters
Patients in group S were awake throughout procedure (ramsey sedation scale 1) while patients in group G had varying degree of sedation in postoperative period. It was observed that, 40% patients from group G did not have pain (visual analogue scale 1) compared to 100% patients from group S with no pain as shown in table 3. Table 3: Comparison of RSS and VAS between two groups
The difference was not statistically significant (p=0.16) with mean birth weight in group S was 2.65±0.25 kg and in group G was 2.58±0.25kg. The difference in APGAR score was statistically significant (p=<0.05) with mean APGAR score at 1 min and 5 min in both the groups as shown in table 4. Table 4: Comparison of various neonatal parameters between two groups
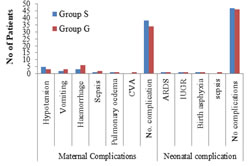
The difference in maternal (p=0.7) and neonatal complications (p=0.9) was not significant as depicted in figure 2. Total ICU admissions in group G were 13 (26%) patients and in group S 3 (6%) patients and difference was statistically significant (p=0.003). There was no death in group S and only 1 death in group G. No neonatal mortality was noted among both the groups. Figure 2: Comparison of maternal and neonatal complications
DISCUSSION Pre-eclampsia is a major cause of maternal mortality and morbidity, and fetal loss worldwide, but particularly in the third world. Anaesthetists may be required to assist with pain management in labor, to provide anesthesia for Cesarean section and to assist in the Intensive Care Management of life-threatening complications which may arise from this condition8. In the present study, total 100 patients with severe preeclampsia underwent their caesarean section either under spinal anaesthesia or general anaesthesia. The mean age of patients were comparable between two groups (Group G= 24.78 ± 5.54 vs Group S= 23.5 ± 4.95) which is similar to study done by Adugna et al.9. However, there was no significant difference in the demographic characteristics of the patients studied except for the mean maternal weight. The characteristics of the women (gestational age, speed of onset, oxygen saturation) and airway examination parameters (Mallampatti grading and thyromental distance, cervical and neck stability) in the two groups were fairly matched and there was no significant difference (P > 0.05). This is comparable with the study done by Dyer et al.3 and Obi et al.10. Among both groups all patients had normal cervical and neck stability. The mean baseline systolic, diastolic BP and MAP of all mothers were high, although in the acceptable range for preeclampsia and found no statistically significant differences (p>0.05). The mean blood pressure of mothers who underwent CS under GA was higher than the mothers who underwent CS under SA throughout the intraoperative period and difference between two groups in regards to intraoperative mean was statistically significant. This finding is in line with previous studies conducted in different regions of the world [9, 11, and12.Present study showed that among group S all cases had Ramsay Sedation Scale 1 and among group G majority 26% had scale 1, 20% had scale 3, 20% had scale 4, 14% had scale 2, 10% had scale 5, 8% had scale 6 and 2% had scale 7. However, in group S all cases had Visual Analogue Scale 1 and in group G majority 40% had scale 1, 22% had scale 2, 22% had scale 3, and 16% had scale 4. Thus, there was no statistically significant difference between two groups, (p>0.05). No study was found comparing RSS and VAS score between spinal and general anaesthesia for severe preeclampsia parturients. Among group S majority 94% had no ICU admission only 6% mothers were admitted in ICU while among group G majority 74% had no ICU admission only 26% mothers were admitted in ICU (p value 0.003). This finding is correlated with the previous studies 2, 13, and 14. In group S, majority 76% had no maternal complication, 10% cases had hypotension, 4% had vomiting, 6% had haemorrhage, 2% had sepsis and 2% had pulmonary edema. Among group G majority 68% had no maternal complication, 6% cases had hypotension, 6% had vomiting, 12% had haemorrhage, 4% had sepsis, 2% had pulmonary edema and 2% had CVA. Thus, maternal complications were more in GA as compared to SA, whereas only hypotension was more seen in spinal anaesthesia but the difference between two groups was not significant, (P=0.7). Similar results are reported in earlier studies2, 13-16.It is likely that, there are many influences on neonatal outcome after caesarean delivery in pre-eclampsia. These including severity of maternal and fetal condition, anaesthesia and surgical management. Fetal development is related to gestational age and to chronic uteroplacental insufficiency, which results in intrauterine growth restriction. In addition any acute maternal deterioration may impact unfavorably on fetal outcome2, 3. In current study, among group S majority 60% had birth weight of neonate more than 2.5 kgs and 40% had less than 2.5 kgs with mean birth weight for was 2.65 +0.25. While among group G 50% had birth weight of neonate more than 2.5 kgs and 50% had less than 2.5 kgs with mean birth weight was 2.58+0.25.These results are in accordance with the studies done by other authors 2, 17 Neonates who were delivered under SA were less likely to have APGAR score of ≤5 at the 1st min of life (6%). This finding had been reported in others studies3, 18, 19.Among group G majority 92% had APGAR at 1 min score more than 5 and 8% had less than 5. And majority 90% had APGAR at 5 min less than 7 and 10% more than 7. Hence, APGAR score noted was good in spinal anaesthesia as compared to general anaesthesia and difference was statistical significance. Conversely, Imtiaz et al.20 and Prakash et al.21 did not demonstrate any difference in the APGAR score in either group. Factors that may affect the neonatal 1st‑min APGAR score was more likely to the related to the indication for the surgery rather than the type of anaesthesia22. Not withstanding, a prolonged induction to delivery time for GA may result in lower APGAR scores for the neonates. More so, a uterine incision to delivery time over 3 min had been reported to be associated with a low APGAR score regardless of anaesthesia technique used23, 24. In both the groups, majority had no neonatal complication; in group S 6% and in group G 8% had complications (ARDS, IUGR, birth asphyxia, sepsis).
CONCLUSION The present study concluded that preeclampsia needs an optimal management; spinal anaesthesia is superior to general anaesthesia for pre-eclamptic mothers in terms of haemodynamic stability in the intraoperative period and a better outcome for the newborns. We found that some of the data that was studied in present study was statistically not significant which may need to be studied on a larger study population
REFERENCES
Policy for Articles with Open Access
|
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
 Home
Home