|
Table of Content - Volume 18 Issue 3 - June 2021
Evaluation of intranasal dexmedetomidine as a premedicant in attenuating hemodynamic stress response to laryngoscopy and intubation
Nagesh Panditrao Jambure1*, Ajita Suhrid Annachhatre2, Yogesh Belapurkar3, Suhrid Annachhatre4
{1,2Assistant Professor, Department of Anaesthesia} {3,4Consultant Cardiac surgeon, Department of CVTS} MGM Medical College and Hospital, Aurangabad, INDIA. Email: sannachhatre@gmail.com
Abstract Background: Hemodynamic changes that occur during the cardiac surgery may lead to myocardial ischemia. Laryngoscopy and endotracheal intubation contribute significantly to hemodynamic changes. These reflexes can be modified by reducing the sensory receptor stimulation (technical or pharmacological) or the efferent responses (parenteral agents). Aim: To evaluate the efficacy of intranasal dexmedetomidine with oral midazolam and IV lignocaine 2% as a premedication and for attenuation of haemodynamic response to laryngoscopy and intubation. To note side effects of dexmedetomidine, if any. Methods: The study was conducted on 60 patients undergone elective CABG under general anaesthesia. These patients were divided in two groups of 30 patients each. The patients were received premedication randomly and in double blinded manner. The hemodynamic parameters namely heart rate, systolic, diastolic, mean blood pressure, SPO2 and ECG changes were monitored. Conclusion: Intranasal dexmedetomidine in the dose of 2 µg/kg reduces the haemodynamic response to tracheal intubation and can maintain stable haemodynamics. Oral midazolam with Inj Lignocaine on the other hand was found to be insufficient to reduce pressure response to intubation and produces tachycardia and increase in blood pressure. keywords: Dexmedetomidine, midazolam, Lignocaine, Hemodynamic, Laryngoscopy, Endotracheal intubation.
INTRODUCTION Preanaesthetic medication forms an integral part of anaesthetic management and some form of premedication is universally administered before general anaesthesia. Laryngoscopy and intubation are the most crucial steps during cardiac surgery as it leads to short lived vague unpredictable haemodynamic stress response. This stress if not attenuated may endanger life of patients with cardiovascular diseases.1, 2, 3, 4 Various methods have been tried to attenuate this transient pressor response e.g. Deep anaesthesia, LMA, drugs like beta blockers, calcium channel blockers, IV Lignocaine, opioids, MgSO4 etc.5,6 Our study was conducted to compare heamodynamic effects of Ketamine and Propofol versus Thiopentone during induction and maintenance of general anaesthesia for minor surgical procedures. The purpose of our study is to evaluate the efficacy of Intranasal Dexmedetodine and IV Lignocaine 2% as a premedication and for attenuation of haemodynamic response to laryngoscopy and intubation.
MATERIAL AND METHOD Our study was conducted after approval from Ethical Committee. Written informed consent was obtained by the attending anaesthesiologist on the morning of surgery. Inclusion Criteria: 1. Patients undergoing elective surgical procedures 2. ASA physical status grade ш 3. Patients between ages 18 to 60 years of either sex. 4. Patient with good ejection fraction. 5. Weight of patient should be between 30-80 kgs. Exclusion Criteria: 1.Psychiatric patients. 2. Patients suffering from renal or hepatic disorder, central nervous system diseases, endocrinal disturbances. 3. Any patients requiring a second attempt of laryngoscopy and intubation or patients in whom duration of laryngoscopy was more than 30 seconds. 4. Patients with anticipated difficult intubation. 5. Patients allergic to study drugs. The study was conducted on 60 patients undergone elective CABG under general anaesthesia. These patients were divided in two groups of 30 patients each which were randomised to receive,
On the day of surgery all the patients were premedicated 90 minutes prior to induction and intubation according to their group allocated. All the patients were monitored and observed with respective parameters after 90 minutes of premedication and just before intubation. All the patients were induced on Inj. fentanyl 4-5 mg/kg b.w. and inj propofol10 to 20 mg I.V in an anaesthetic dose followed by Inj. Succinylcholine 2 mg/kg b.w. Then under direct laryngoscopic vision intubation was done, all intubations were smooth and gentle and were done with Macintoch blade within 30 seconds. All the observations like heart rate, systolic, diastolic blood pressure, MAP, RPP, the Sedation score, Anxiety score, and dose of Fentanyl required for induction, post operative shivering, post operative nausea and vomiting, respiratory rate, status of tongue (normal, dry or moist) and other undesirable effects were also noted. Statistical analysis: Percentage distribution of age group, gender and operative procedure was compared in between the groups using non parametric (Pearson Chi-Square test) statistical test. Statistical analysis was performed using SPSS (statistical package for social science) software for windows version 17 (SPSS inc., Chicago, illinois, USA).
RESULT
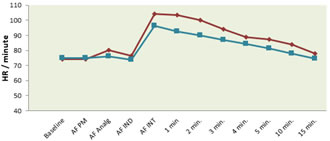
Graph 1: Heart rate during induction Mean heart rate of Lignocaine group was significantly (p<0.01) higher than dexmedetomidine group throughout the procedure. Compared to baseline value mean heart rate rise in Lignocaine patients were more than that dexmedetomidine group.
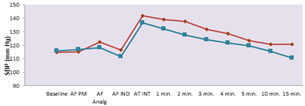
Graph 2: Systolic blood pressure during induction Graph 3:Diastolic blood pressure during induction There was fall in systolic blood pressure after dexmedetomidine which was significant (p<0.05)than Lignocaine induction up to the first 5 minutes. Compared to baseline, SBP fall in dexmedetomidine induced patients was more than that of Lignocaine induction group. The diastolic blood pressure upto first 5 min of dexmedetomidine group was significantly (p<0.01) lower than that of the Lignocaine induced group.
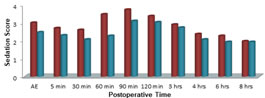
Graph 4: Postoperative sedation score
Table 1
DISCUSSION Sympathoadrenal activation associated with laryngoscopy and endotracheal intubation causes rise in arterial blood pressure and tachycardia. The satisfactory role of preoperative DEX for attenuation of laryngoscopic stress responses is well established. Nowadays besides IV route, use of IN DEX as premedication is becoming popular, especially in paediatric population.7 Prevention of tachycardia in response to laryngoscopy and intubation and the slowing of the heart rate induced by alpha2 agonist share a complex underlying mechanism. It consists of at least three different components, centrally the activation of alpha-2 adrenoceptors causes both a reduction in peripheral sympathetic tone and an increase of vagally induced reflex bradycardia, peripherally stimulation of presynaptic alpha adrenoceptors leads to diminished release of norepinephrine from the nerve endings towards the vasculature and to a reduction in peripheral sympathetic tone towards the heart.8 It is found that 60 minutes after premedication there is significant difference in heart rate, systolic, diastolic and mean arterial pressure. In Dexmedetomidine group there is significant decrease in heart rate, systolic, diastolic and mean arterial blood pressure after premedication than the other group (P<0.001). At the same time In Lignocaine group, there was significant rise in the heart rate and systolic blood pressure. Also after laryngoscopy and intubation there is highly significant difference in the groups regarding heart rate, systolic, diastolic, MAP and rate. Fifteen minutes after intubation in patients of Dexmedetomidine group heart rate and blood pressure returned back to the baseline but had remained above the baseline in patients of Lignocaine group. Sedation scores at induction in both groups were not significantly different, but when assessed after extubation, the score was significantly higher with Dexmedetomidine group patients. In postoperative period, patients of both the groups remained sedated, but patients of Dexmedetomidine group had deeper sedation for longer time than patients of lignocaine group. Zanaty and El Metainy9 compared nebulised dexmedetomidine, nebulised ketamine and their combination. They concluded that the combination resulted in better sedation, smoother induction and more rapid recovery. Another study by Abdel-Ghaffar HS et al.10 comparing nebulised dexmedetomidine, ketamine and midazolam found that nebulised dexmedetomidine provided more satisfactory sedation with shorter recovery time. But most of these studies were done in the paediatric population. The Dexmedetomidine group had least increase in heart rate, systolic, diastolic, MAP and rate pressure product than other groups (P<0.001) and at the same time it never rose above the baseline. In case of Lignocaine group there is highly significant increase in heart rate, systolic, diastolic, MAP and rate pressure product even at the end of 5 minutes after laryngoscopy and intubation. Comparatively Dexmedetomidine is more efficient regarding attenuation of stress response to laryngoscopy (P0<0.001). Wang SS et al. concluded that IN DEX (1 μg/kg) provides considerable effect to attenuate the increase in MAP caused by intubation response. Changes in HR and BIS also demonstrate that this kind of premedication provides effective attenuation of intubation responses.11 Again the Dexmedetomidine group required significantly less dose of Fentanyl for induction than other group (P<0.001). Also Dexmedetomidine group had significantly low incidence of post operative nausea, vomiting and shivering along with significant antisialogogue action (P<0.001). Rashmi and Komala et al. evaluated the effect of intravenous dexmedetomidine on hemodynamic responses to laryngoscopy and intubation. In these three studies, HR, DBR, SBP, and MAP reduced in the dexmedetomidine group, indicating its effectiveness in attenuating hemodynamic response to laryngoscopy and intubation.12
CONCLUSION It was concluded that intranasal Dexmedetomidine in the dose of 2 µg/kg reduces the haemodynamic response to tracheal intubation and can maintain stable haemodynamics. Dexmedetomidine also provides adequate and longer postoperative analgesia compared to Lignocaine.
REFERENCES
Policy for Articles with Open Access: Authors who publish with MedPulse International Journal of Pediatrics (Print ISSN: 2579-0897) (Online ISSN: 2636-4662) agree to the following terms: Authors retain copyright and grant the journal right of first publication with the work simultaneously licensed under a Creative Commons Attribution License that allows others to share the work with an acknowledgement of the work's authorship and initial publication in this journal. Authors are permitted and encouraged to post links to their work online (e.g., in institutional repositories or on their website) prior to and during the submission process, as it can lead to productive exchanges, as well as earlier and greater citation of published work.
|
|
 Home
Home