|
Table of Content - Volume 18 Issue 3 - June 2021
Effect of vasopressors on fetal umbilical arterial blood after spinal anaesthesia during caesarean section
Divya V1*, Mopuru Pradeep2, Radhika K3
1Assistant Professor, Department of Anaesthesiology, SUT Academy of Medical Sciences, Thiruvananthapuram, Kerala, INDIA. 2Civil Assistant Surgeon, Department of Anaesthesiology, District Government Hospital, Kadapa, Andhra Pradesh, INDIA. 3Professor and HOD, Department of Critical Care Medicine, GG Hospital, Trivandrum, INDIA. Email: divyadoc87@gmail.com
Abstract Background: Hypotension is commonly seen with spinal anaesthesia which can have damaging effects on the mother and foetus. The present study aimed to evaluate the effect of vasopressors on foetal umbilical arterial blood after spinal anaesthesia during caesarean section. Materials and Methods: The study was done in the Department of Anaesthesiology, Sree Gokulam Medical College, Trivandrum, Kerala. A total of 50 patients were included in the study on the basis of inclusion and exclusion criteria. G-I received Phenylephrine (100µg/ml) and G-II received Ephedrine (5 mg/ml). All the patients’ age, weight, SBP, HR, APGAR score, pH, PCO2, PO2, HCO-3, nausea and vomiting were recorded. The data was analysed by SPSS (20.0) version. Results: Comparison of age, weight, SBP, APGAR score, PO2 and HCO-3 not showed any significant difference between the groups. HR at 3 min, pH and PCO2 showed significant difference between the groups. 3 patients in group-I and 8 in group-II had nausea and vomiting. Conclusion: The study results conclude that phenylephrine showed less fetal side effects compared to ephedrine. Keywords: APGAR score, Ephedrine, Heart rate, Arterial blood gases, pH, Phenylephrine.
INTRODUCTION Spinal anaesthesia is the common method used for caesarean delivery as it avoids the risks of general anaesthesia related to difficult intubation and aspiration of gastric contents. Hypotension is commonly seen with spinal anaesthesia, which can have damaging effects on the mother and neonate like nausea, vomiting and dizziness in the mother, also decreased utero-placental blood flow which can cause impaired fetal oxygenation and fetal acidosis. Maternal effects -In spinal anaesthesia for obstetric patients hypotension is regarded as the most common complication1. It is estimated to occur in approximately 30-90% of the patients2. There is decrease in systemic vascular resistance due to sympathetic blockade and also an exaggerated neuro blockade because of a contracted subarachnoid space and aortocaval compression, all of them which can cause hypotension3. Hypotension can cause cerebral hypo-perfusion and brainstem ischemia, leading to activation of the vomiting center4. Maternal hypotension may result in unpleasant symptoms such as nausea, vomiting and light-headedness. Besides that when severe and sustained hypotension can impair uterine and inter-villous blood flow which can ultimately result in fetal acidosis and neonatal depression. For the maternal safety, comfort and fetal wellbeing, hypotension during spinal anaesthesia for caesarean delivery should be minimized. It is usually considered that aortocaval compression predisposes the mother to reduced venous return and so cardiac output and blood pressure are also decreased during spinal anaesthesia for caesarean delivery. However, many measures are advocated to improve venous return, including lateral tilt and numerous fluid administration regimens, but all have failed to eliminate hypotension5. Fetal effects- Spinal anaesthesia induced hypotension along with utero-placental ischemia and inter-villous hypoxemia, which are hallmarks of severe preeclampsia may trigger chronic hypoxic feto-placental vasoconstriction and can lead to feto-placental hypertension and “cor placentale.”6. Stress-induced catecholamine release can decrease uterine blood flow and provokes fetal asphyxia. Exogenous epinephrine and norepinephrine impairs fetal oxygenation.Any accidental or deliberate intravenous (IV) epinephrine administration can adversely affect human uterine blood flow. Anxiety and epinephrine levels can also influence the duration of labor and the fetal heart rate pattern. When spinal anaesthesia induced hypotension and aortocaval compression coexist, fetal acidosis is more severe7. Drugs which are used to treat hypotension may theoretically enhance or interfere with placental hypoxemic feto-placental vasoconstriction. Hypoxic feto-placental vasoconstriction is a physiologic response similar to pulmonary hypoxic vasoconstriction. It compensates for ventilation/perfusion (V/Q) inequalities in the lungs. It is thought to do the same for placental maternal/fetal (Qm/Qf) circulatory matching8. Spinal anaesthesia-induced hypotension and consequent uteroplacental insufficiency and intervillous hypoxemia may likely trigger hypoxic feto-placental vasoconstriction9. Ephedrine which has a strong β-adrenergic and a weaker α-adrenergic effects has been recommended commonly, but its use has been in debate because of potential complications like supra-ventricular tachycardia, tachyphylaxis and most importantly fetal acidosis. It can increase nitric oxide (NO) expression in uterine arteries. NO in turn increases maternal cyclic nucleotide concentrations, a biological pathway which is thought to enhance uterine blood flow11. Phenylephrine and α-adrenergic agonist can also be used for prevention and treatment of maternal hypotension. Moreover, it may reduce the incidence of nausea and vomiting and also fetal acidosis, but it might cause maternal bradycardia. The exact dose for administration of phenylephrine is undetermined and the current practice includes both phenylephrine infusion and intermittent bolus administration. The effects on baroreceptor sensitivity have been studied but not on their effect on maternal cardiac output or their success in maintaining maternal blood pressure at baseline during caeserean delivery under spinal anaesthesia. However, studies over the last two decades have indicated that fetal acid-base status might be improved if phenylephrine or other adrenergic agonists are used during caesarean delivery instead of ephedrine. Consequently the use of phenylephrine for arterial blood pressure management during caeserean delivery under spinal anaesthesia has been increased. The present study is done to compare the effect of vasopressors phenylephrine and ephedrine on fetal umbilical arterial blood after spinal anaesthesia during caeserean section.
MATERIALS AND METHODS Study settings: The comparative study was done in the Department of Anaesthesiology, Sree Gokulam Medical College and Research Foundation, Trivandrum, Kerala. The study duration is one year (January 2014-15). Inclusion criteria: Age above 18 years. ASA grade-I. Willing to sign on informed consent form Exclusion criteria: Contraindication to spinal block. Allergy to local anaesthetics. Pre-existing systemic disease. Known fetal abnormalities. On medication of diuretics, steroids. Groups Group-I: Phenylephrine (100µg/ml/iv) Group-II: Ephedrine (5 mg/ml/iv) Procedure The study included 50 patients based on the inclusion and exclusion criteria. They were divided randomly into two groups. All the patients were explained about the study procedure and informed consent was obtained. Both the groups were administered respective drugs whenever there is reduction in the systolic blood pressure. All the patients age, weight, SBP, HR, APGAR score, pH, PCO2, PO2, HCO-3, nausea and vomiting were recorded and analysed. Statistical analysis The data was expressed in number, percentage, mean and standard deviation. Statistical Package for Social Sciences (SPSS 20.0) version used for analysis. Unpaired t test and Chi square test applied to find the statistical significance between the groups. P value less than 0.05 (p<0.05) considered statistically significant at 95% confidence interval.
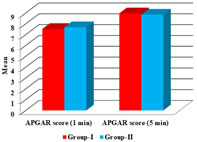
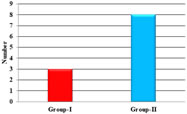
RESULTS Total 50 patients were included in the study and divided into two groups each of 25. Comparison of mean age, weight, systolic blood pressure (Baseline, 1min and 3 min) and heart rate at 1 min not showed any significant difference between group-I and II. There is significant (p<0.001) difference observed in heart rate at 3 min between the group-I and II (Table-1). APGAR score at 1 and 5 min compared between the group-I and II not showed any significant difference (Graph-1). pH and PCO2 showed significant difference between group-I and II with p value less than 0.001. PO2 and HCO-3 not showed significant difference between the groups (Table-2). 3 patients in group-I and 8 patients in group-II showed nausea and vomiting (Graph-2). Table-1: Comparison of mean age, weight, systolic blood pressure (SBP) and heart rate (HR) between the group-I and II
(*p<0.05 significant compared group-I with group-II)
Graph 1: Comparison mean APGAR score between the group-I and II (p>0.05 no significant difference compared between group-I and II)
Table 2: Comparison of mean arterial blood gases between the group-I and II
(*p<0.05 significant compared group-I with group-II)
Graph 2: Comparison of incidence of nausea and vomiting between the group-I and II (p>0.05 no significant difference compared between group-I and II)
DISCUSSION Spinal anaesthesia for elective caeserean delivery has been associated with a higher incidence of fetal acidosis at delivery than epidural or general anaesthesia. The increased incidence of fetal acidosis associated with spinal anaesthesia is likely to be secondary to maternal hypotension or to be a side effect of drugs used in the prevention or treatment of hypotension. This study was conducted in 50 patients, who were of the American Society of Anaesthesiologists (ASA) class-I admitted for elective caesarean section in Sree Gokulam Medical College and Research Foundation. They were allocated into two equal groups of 25 each based on the use of vasopressor. Group-I received a bolus of Phenylephrine (100 μg/ml) and Group-II received boluses of Ephedrine (5 mg/ml). There was not much of difference in age between both the groups. The mean age of group-I was 24.28 and that of group-II was 24.76 and the mean weight of group-I was 71.44 and that of group-II was 69.72. There is no consensus to the optimal mode of management in prevention and treatment of maternal hypotension due to spinal anaesthesia. α- adrenergic agonists such as ephedrine or phenylephrine can be given safely for prevention or treatment of hypotension due to spinal anaesthesia for caesarean section. In my study both the drugs were effective in managing hypotension. The present study results were further supported by Simin A et al., who found that both were effective in managing hypotension after spinal anaesthesia in caesarean patients. Mean of both the groups was statistically similar. Adequate pre loading and aggressive pharmacological interventions showed better results in managing hypotension as shown by previous studies. Despite its high efficiency in increasing blood pressure, phenylephrine causes reflex bradycardia which may lead to decrease in cardiac output. It causes more reduction of utero-placental blood flow. On the contrary tachycardia is seen with ephedrine, because of its actions on the beta receptors in the heart. Ngan Kee et al., studied the combination of phenylephrine and ephedrine in different ratios given as infusion to minimise the cardiac effects of the vasopressors. They concluded that the combination of vasopressors has no added advantage compared with any vasopressor alone11. This study was even supported by Loughrey et al., in which they have concluded that the combination of two vasopressors were not superior to ephedrine alone12. Although phenylephrine caused bradycardia, that was not of much significance in my study as none of the patients required a supplement dose of atropine or glycopyrrolate for treating bradycardia. The bolus doses of phenylephrine (100 μg/ml) and ephedrine (5 mg/ml) used in my study was determined empirically. Bases on the study conducted by Prakash et al., in which they compared the efficacy of phenylephrine 100μg and ephedrine 6 mg in the treatment of maternal hypotension13. Saravanon et al., demonstrated a potency ratio of 80:1 (100 μg phenylephrine ~10 mg ephedrine) for equivalence between phenylephrine and ephedrine as infusion in prevention of hypotension induced spinal anaesthesia14. Maternal nausea and vomiting is a significant problem during spinal anaesthesia for caeserean delivery. In this study 8 patients of the ephedrine group and 3 of phenylephrine group had nausea and vomiting. It may be due to the magnitude of hypotension and may be related to the faster response time to the vasopressors. In the present study, there was no significant difference in this regard between the two groups. Nausea and vomiting may have been secondary to an absolute or relative increase in vagal tone. There is evidence for a vagal mechanism causing nausea during spinal anaesthesia15. There was decrease in pH in group-II who received ephedrine as bolus dose for hypotension which might be because of reduced uteroplacental perfusion from decreased maternal artery pressure, reduced uteroplacental perfusion from ephedrine induced uteroplacental vasoconstriction or by a direct fetal effect of ephedrine. Although mild acidosis was seen in the ephedrine group, true acidosis was not found in any of them. This may be because the amount of drug required to treat hypotension is much lower than the previous studies. Uteroplacental resistance or flow were not measured directly but there is indirect evidence which suggests that reduced uteroplacental perfusion was not the main mechanism for the increased incidence of acidosis in the ephedrine. Eisler et al., studied that by giving a beta-2 adrenergic stimulant to the mother 2 hrs prior to delivery of the fetus by elective caesarean section can cause fetal metabolic acidemia16. Ephedrine induced beta adrenergic stimulation of the fetus is a possible mechanism for fetal acidemia that does not involve the uteroplacental or fetoplacental circulations. This was further supported by a study conducted by Gournay et al., in which beta adrenergic stimulation of the fetal lamb with isoproterenol produced an initial increase in oxygen consumption, and an increase in glucose and lactic acid17. Wright et al., gave ephedrine to the mother and found that it has fetal effects. It can be reflected by an increase fetal heart rate and fetal catecholamine levels. The umbilical artery PCO2 was higher in the ephedrine group than in the phenylephrine group which may be due to increased CO2 production by the fetus, supporting an increase in fetal metabolic rate in the ephedrine group18. In this study the increase in fetal metabolic rate secondary to ephedrine induced beta adrenergic stimulation, may be the most likely mechanism for the increased incidence of fetal acidosis in the ephedrine group. Current evidence supports APGAR scores as a better predictor of neonatal outcome than measurement of umbilical artery pH. Casey BM et al., concluded that APGAR scoring system as a relevant predictor of neonatal survival. The present study APGAR scores were good for all new born infants and none required tracheal intubation and ventilation or admission to the special care baby unit in the immediate post delivery period. All the new born had a 5 min score of 8-10. There may even be benefitted from fetal catecholamine stimulation before delivery. Maternal administration of a beta-2 adrenergic agonist prior to delivery by elective caeserean section can increase dynamic lung compliance, decrease airway resistance and decrease respiratory rate and reduce the risk of hypoglycemia in the newborn infant.
CONCLUSION Phenylephrine proves to be a better option in managing hypotension with minimal effects on fetus. Ephedrine caused fetal acidosis by decreasing umbilical arterial pH as compared to phenylephrine.
REFERENCES
Policy for Articles with Open Access: Authors who publish with MedPulse International Journal of Pediatrics (Print ISSN: 2579-0897) (Online ISSN: 2636-4662) agree to the following terms: Authors retain copyright and grant the journal right of first publication with the work simultaneously licensed under a Creative Commons Attribution License that allows others to share the work with an acknowledgement of the work's authorship and initial publication in this journal. Authors are permitted and encouraged to post links to their work online (e.g., in institutional repositories or on their website) prior to and during the submission process, as it can lead to productive exchanges, as well as earlier and greater citation of published work.
|
|
 Home
Home