Official Journals By StatPerson Publication
|
Table of Content Volume 6 Issue 3 - June 2018
Comparative evaluation of the effect of intrathecal ketamine and fentanyl added to bupivacaine in elective hernia repair surgeries
Original Research Article
T Murugan1, N Sathyan2*, Anju Daniel Prasath3, Subha4
1Professor, Department of Anaesthesiology, Government Kilpauk Medical College and Hospital, Kilpauk, Chennai–10, Tamil Nadu, INDIA. 2Associate Professor, Department of Anaesthesiology, Government Thiruvarur Medical College, Thiruvarur-610004, Tamil Nadu, INDIA. 3,4Jr. Resident, Government Kilpauk Medical College, Chennai- 10, Tamil Nadu, INDIA. Email: drsathyan76@gmail.com
Abstract Background: Addition of adjuvants in spinal anaesthesia spares the local anaesthetic dose and produces good postoperative analgesia. Aim: To compare the duration of prolongation of postoperative analgesia between Ketamine and Fentanyl when added to hyperbaric bupivacaine for elective inguinal hernia surgeries. Material and Methods: This is a non randomised prospective triple arm single blind comparative study including 90 patients undergoing elective inguinal hernia repair surgery. Patients satisfying inclusion criteria, with written consent were divided into three groups : Group B receiving a spinal drug volume of 3ml hyperbaric 0.5 % bupivacaine with 0.5 ml normal saline, Group F receiving a spinal drug volume 3ml hyperbaric 0.5 % bupivacaine with 25 mcg fentanyl (0.5ml), Group K received a spinal volume 3ml hyperbaric 0.5% bupivacaine with 25 mg preservative free Ketamine (0.5ml). The time of onset of sensory and motor blockade, duration of sensory and motor blockade, time of requirement of first dose analgesic, total analgesic requirement were recorded apart from the vital hemodynamic and saturation monitoring. Requirement for ephedrine and incidence of adverse effects were also recorded. Results: Addition of Ketamine and Fentanyl to Bupivacaine prolongs the onset of sensory and motor blockade; prolongation is greater with fentanyl than with ketamine. Ketamine and Fentanyl when added to hyperbaric bupivacaine prolongs the duration of motor and sensory blockade; prolongation being greater with ketamine than fentanyl. The total ephedrine requirement and the total analgesic requirement in the first 24 hours period was significantly lower in the Ketamine group compared to Fentanyl or control group. Conclusion: Intrathecal Ketamine is a better adjuvant to hyperbaric bupivacaine than intrathecal fentanyl in prolonging the duration of blockade and postoperative analgesia in patients undergoing inguinal hernia repair under spinal anaesthesia. Key Words: Spinal anaesthesia, Ketamine, Fentanyl, Onset, Duration of block, Analgesia.
INTRODUCTION Spinal anaesthesia, till date, remains the most preferable technique of choice for all infraumbilical surgeries, by most anaesthesiologists. The only disadvantage being the profound motor blockade that remains after the procedure. Reducing the dose of hyperbaric bupivacaine results in rapid recovery, but inadequate surgical anaesthesia.1 Addition of adjuvants like opioids, alpha 2 agonists, ketamine, neostigmine and vasoconstrictors help enhance the analgesia, with a lowered side effect profile.2,3,4,5,6 Till date, opioids are the most commonly used adjuncts in spinal anaesthesia, but its use is often associated with side effects.7 The use of opioids may result in a reduction in the pain threshold, causing a delayed hyperalgesia.8 Ketamine is an N-methyl D-aspartate receptor (NMDA) antagonist with good analgesic and local anaesthetic properties. In addition to NMDA receptors, it also interacts with opiate, cholinergic, adrenergic and serotonin receptors.9,10,11,12,13 It has been proved that single or multiple doses of preservative free racemic ketamine has no adverse neurological effects, but instead may also have neuroprotective effects.14,15,16
MATERIALS AND METHODS 90 patients posted for inguinal hernia surgeries at Government Kilpauk Medical College Hospital and Government Royapettah hospital from August 2017 to February 2018 were assessed for the inclusion and exclusion criteria and were included in the study after obtaining written informed consent. Sample Size: 90, calculated using the OPENEPI software (The confidence level was estimated at 95%, Power of study at 80%,minimum sample size required for the study was calculated to be 90.n=30 in Group K, n= 30 in Group F and n=30 in Group B arm) Study Design: A prospective, Non–Randomized, Triple Arm, Single-Blind, Controlled study Inclusion Criteria
Patients who have given valid informed consent Exclusion Criteria
Materials
Methodology: Patients satisfying the above inclusion criteria were counselled about the purpose, risks and benefits of the procedure and study.. After getting consent, patients willing to be included in the study were enrolled and analyzed. A total of 90 patients were included in the study. Patients were divided into three groups of 30 in each based on computerized random number into group B, group F and group K. GROUP B received a spinal drug volume of 3cc of hyperbaric 0.5 % bupivacaine with 0.5cc of normal saline GROUP F received a spinal drug volume of 3cc of hyperbaric 0.5% bupivacaine with 25 mcg of fentanyl (0.5ml) GROUP K received a spinal drug volume of 3cc of hyperbaric 0.5% bupivacaine with 25mg of preservative free ketamine (0.5ml) This study was designed as a prospective, comparative study. Patients were preoperatively evaluated, clinically examined and proper investigations were done prior to the assessment. Procedures were explained in detail and written consent was obtained. All patients were kept nil per oral for atleast 6 hours before the procedure. Patients were shifted inside the operation theatre half an hour before the scheduled procedure. All patients were pre-medicated with intramuscular injection glycopyrollate 0.2mg. Baseline vitals such as pulse rate, non-invasive blood pressure, saturation in room air, respiratory rate, ECG pattern were recorded. Intravenous access was obtained with 18G IV cannula and IV fluid started. All patients were preloaded with 5-7 ml/kg lactated Ringer’s solution before administering spinal anesthesia. Using all aseptic precautions, a 25-gauge Quincke needle was inserted intrathecally via a midline approach into the L4-5 interspaces while the patient was in sitting position.
Data Analysis: Descriptive statistics was done for all data and were reported in terms of mean values and percentages. Suitable statistical tests of comparison were done. Continuous variables were analyzed with the unpaired t test. Categorical variables were analyzed with the Chi-Square Test and Fisher Exact Test. Statistical significance was taken as P < 0.05. The data was analyzed using SPSS version 16 and Microsoft Excel 2007
Table 1: Null hypothesis
OBSERVATIONS AND RESULTS
Table 2: Age
Table 3:
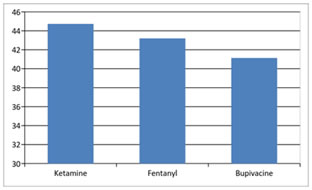
Figure 1: Among the patients undergoing spinal anaesthesia for inguinal hernia surgeries, there was no statistical difference in relation to age distribution between the three groups with a p value >0.05 as per the unpaired t test. Therefore we fail to reject the null hypothesis that there is no age difference between the intervention groups.
Table 4: Onset time of sensory blockade
Figure 2: Table 5:
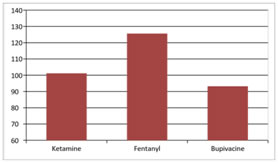
Among the three groups of patients undergoing spinal anaesthesia for inguinal hernia surgeries, there was a statistically significant difference in the onset of sensory blockade in the ketamine and fentanyl groups compared to the control group, with p value <0.05 as per the ANOVA test. Therefore, we reject the null hypothesis that there is no difference in the onset time of sensory blockade in the three groups. The onset time of sensory block was longest in Group F (125.60±2.53 sec) compared to Group K (101.20± 1.48 sec), with a p value of 0.0001 as per t test. Onset of Motor Blockade
Table 6:
Table 7:
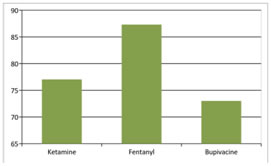
Figure 3: Among the three groups of patients undergoing spinal anaesthesia for inguinal hernia surgeries, there was a statistically significant difference in the onset of motor blockade in the ketamine and fentanyl groups compared to the control group, with p value <0.05 as per the ANOVA test. Therefore, we reject the null hypothesis that there is no difference in the onset time of motor blockade in the three groups. The onset time of motor block was longest in Group F (87.30±1.06 sec) compared to Group K (77.03± 0.61 sec), with a p value of 0.0001 as per t test.
Table 8: Duration of sensory block
Table 9:
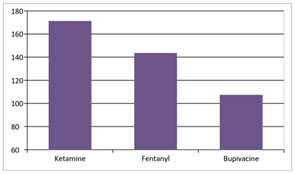
Figure 4: Among the three groups of patients undergoing spinal anaesthesia for inguinal hernia surgeries, there was a statistically significant difference in the duration of sensory blockade in the ketamine and fentanyl groups compared to the control group, with p value <0.05 as per the ANOVA test. Therefore, we reject the null hypothesis that there is no difference in the duration of sensory blockade in the three groups. The duration of sensory blockade was longest in Group K (171.33±3.73 min) compared to Group F (143.67± 1.50 min), with a p value of 0.0001 as per t test.
Table 10: Duration of motor blockade
Table 11:
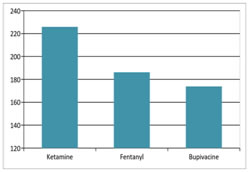
Figure 12: Among the three groups of patients undergoing spinal anaesthesia for inguinal hernia surgeries, there was a statistically significant difference in the duration of motor blockade in the ketamine and fentanyl groups compared to the control group, with p value <0.05 as per the ANOVA test. Therefore, we reject the null hypothesis that there is no difference in the duration of motor blockade in the three groups. The duration of motor blockade was longest in Group K (225.83±2.26 min) compared to Group F (186.17± 1.90 min), with a p value of 0.0001 as per t test.
Table 12: Request for first analgesic
Table 13:
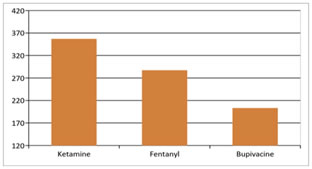
Figure 13: Among the three groups of patients undergoing spinal anaesthesia for inguinal hernia surgeries, there was a statistically significant difference in the request for first analgesic in the ketamine and fentanyl groups compared to the control group, with p value <0.05 as per the ANOVA test. Therefore, we reject the null hypothesis that there is no difference in the time for request for first analgesic in the three groups. The time for request for first analgesic was longest in Group K (357.00±7.17 min) compared to Group F (287.33± 3.53 min), with a p value of 0.0001 as per t test.
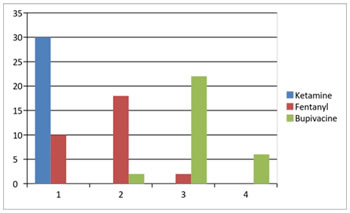
Table 13: Total analgesic requirement
Figure 14: Among the three groups of patients undergoing spinal anaesthesia for inguinal hernia surgeries, there was a statistically significant difference in the total analgesic requirement in the ketamine group compared to the fentanyl and control group, with p value <0.05 as per the Chi-square test. Therefore, we reject the null hypothesis that there is no difference in the total analgesic requirement in the three groups.
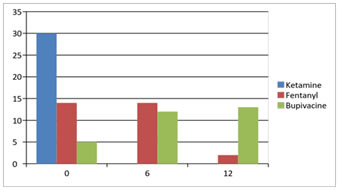
Table 14: Total ephedrine requirement
Figure 15:
Among the three groups of patients undergoing spinal anaesthesia for inguinal hernia surgeries, there was a statistically significant difference in the total ephedrine requirement in the ketamine group compared to the fentanyl and control group, with p value <0.05 as per the Chi-square test. Therefore, we reject the null hypothesis that there is no difference in the total ephedrine requirement in the three groups.
Table 15: Post operative adverse effects
Table 16:
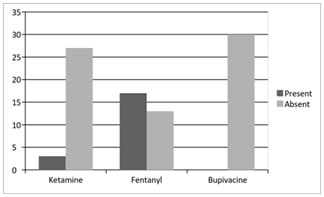
Figure 16: Among the three groups of patients undergoing spinal anaesthesia for inguinal hernia surgeries, there was a statistically significant difference in the total incidence of post- operative adverse effects in the ketamine and fentanyl group compared to the control group, with p value <0.05 as per the Chi-square test. Therefore, we reject the null hypothesis that there is no difference in the incidence of post- operative adverse effects in the three groups.
DISCUSSION Spinal anaesthesia or sub arachnoid block till date remains the most favoured mode of anaesthesia for most infraumbilical surgeries, unless otherwise contraindicated. It offers several advantages over general anaesthesia, the major ones being-reduction in the stress response to surgery, reduction in the blood loss and better post-operative pain relief. The main disadvantage of spinal anaesthesia is the profound motor blockade that remains after surgery. Reducing the dose of local anaesthetic used for spinal anaesthesia may help overcome this problem, but results in inadequate pain relief. Addition of adjuvants to intrathecal bupivacaine helps in prolonging the duration of spinal anaesthesia, along with reducing the density of motor blockade. Various adjuvants are being used- like opioids, alpha 2 agonists, neostigmine, the most common being opioids. However, opioids are known for a number of adverse effects, the most dreadful being respiratory depression. In addition, repeated use of opioids can reduce the threshold of pain perception, and results in a hyperalgesic response. Ketamine is an N-methyl D-aspartate receptor antagonist, which has analgesic and local anaesthetic properties. It also interacts with opioid, cholinergic and adrenergic receptors. Recent studies have proved that preservative free ketamine does not cause any neurotoxicity; but instead may have neuroprotective effects. In this prospective study, the effect of adding ketamine to intrathecal bupivacaine on the duration of postoperative analgesia was compared with that of fentanyl. 90 patients satisfying the inclusion criteria were chosen and divided into three groups. Group K received 3cc of 0.5% hyperbaric bupivacaine with 0.5mg/kg of preservative free ketamine; Group F received 3cc of 0.5% hyperbaric bupivacaine with 25mcg of fentanyl citrate; Group B received 3cc of 0.5% hyperbaric bupivacaine with 0.5cc of normal saline. The mean age was 44.73±2.16 in Group K; 43.20±1.60 in Group F and 41.13±2.04 in Group B. Hence all the three groups were comparable with respect to age as the P value was greater than 0.05. The time for onset of sensory blockade which was assessed by the absence of sensation to pin prick at the T10 dermatome was 101.20±1.48 seconds in Group K; 125.60 ±2.53 in Group F and 93.23±0.69 seconds in Group B. This implies that the addition of ketamine or fentanyl to bupivacaine prolongs the onset of sensory blockade. There was a statistical difference between Group K and F in the onset of sensory blockade implied by the T test value of -8.326 and a P value of 0.0001; the prolongation of onset of sensory blockade is greater with fentanyl than with ketamine. The time for onset of motor blockade which was assessed by the modified Bromage score was 77.03±0.61 seconds in Group K; 87.30 ±1.06 in Group F and 73.00±0.98 seconds in Group B. This implies that the addition of ketamine or fentanyl to bupivacaine prolongs the onset of motor blockade. There was a statistical difference between Group K and F in the onset of motor blockade implied by the T test value of -8.401 and a P value of 0.0001; the prolongation of onset of motor blockade is greater with fentanyl than with ketamine. The total duration of sensory blockade after spinal anaesthesia was 171.33±3.73 minutes in Group K; 143.67 ±1.50 in Group F and 107.50±1.45 minutes in Group B. This implies that the addition of ketamine or fentanyl to bupivacaine prolongs the duration of sensory blockade. There was a statistical difference between Group K and F in the duration of sensory blockade implied by the T test value of 7.499 and a P value of 0.0001; the prolongation of sensory blockade is greater with ketamine than with fentanyl. The total duration of motor blockade after spinal anaesthesia was 225.83±2.26 minutes in Group K; 186.17 ±1.90 in Group F and 173.83±1.53 minutes in Group B. This implies that the addition of ketamine or fentanyl to bupivacaine prolongs the duration of motor blockade. There was a statistical difference between Group K and F in the duration of motor blockade implied by the T test value of 13.431 and a P value of 0.0001; the prolongation of motor blockade is greater with ketamine than with fentanyl. The first request for analgesia after spinal anaesthesia was made after 357.00±7.17 minutes in Group K; 287.33±3.53 in Group F and 203.33±2.16 minutes in Group B. This implies that the addition of ketamine or fentanyl to bupivacaine prolongs the duration of spinal analgesia. There was a statistical difference between Group K and F in the request for first analgesic after spinal anaesthesia implied by the T test value of 8.713 and a P value of 0.0001; the prolongation of the duration of spinal analgesia is greater with ketamine than with fentanyl. The total analgesic requirement in the first 24 hour period after spinal anaesthesia was significantly lower in the ketamine group when compared to the fentanyl or control group. In Group K, all the thirty patients had made an analgesic request only once in the first 24 hours. In Group F, 10 patients had made an analgesic request once; 18 patients twice and 2 patients thrice in the first 24 hours. In Group B, 2 patients had made an analgesic request twice, 22 patients thrice and 6 patients had made an analgesic request four times in the first 24 hours. Thus, the values were statistically significant as implied by the Chi-square test value of 113.20 and a P value of 0.0001. The total ephedrine requirement after spinal anaesthesia was significantly lower in the ketamine group when compared to the fentanyl or control group. In Group K, ephedrine was not required in any of the thirty patients. In Group F, 6 mg of ephedrine was used in 14 patients; 12 mg ephedrine was used in 2 patients. In Group B, 6 mg ephedrine was used in 12 patients; 12 mg ephedrine was used in 13 patients. Thus, the values were statistically significant as implied by the Chi-square test value of 52.463 and a P value of 0.0001. The incidence of adverse effects was statistically significant in the fentanyl and ketamine group when compared to the control group. In Group K, 2 patients had complained of drowsiness; while one patient complained of nausea. In Group F, 14 patients complained of pruritus; 2 patients complained of drowsiness; while one patient complained of urinary retention. SUMMARY It was interpreted from the study that,
CONCLUSION It is concluded that intrathecal ketamine is a better adjuvant to bupivacaine than intrathecal fentanyl in prolonging the duration of postoperative analgesia after spinal anaesthesia in patients undergoing inguinal hernia repair.
REFERENCES
|
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
 Home
Home