Official Journals By StatPerson Publication
|
Table of Content Volume 6 Issue 3 - June 2018
Comparison of the ultrasound guided technique versus the traditional blind anatomical landmark technique for the placement of central venous catheter in the internal jugular vein
Original Research Article
A Ganesh1, D Ashok Kumar2*, R Kanthimathy3
1Sr. Assistant Professor, 2,3Associate Professor, Department of Anaesthesiology, Rajiv Gandhi Government General Hospital, Madras Medical College, Chennai, Tamil Nadu, INDIA. Email: drganesh78@gmail.com, ashokpainclinic@gmail.com
Abstract Background: Internal jugular venous access is an essential part of patient management in many clinical settings. In the traditional technique, rates of major and minor complications can be as high as 10%. Ultrasound guided central venous access is a useful application of real-time ultrasound technology in the field of Anaesthesiology and Critical care that can decrease complication rate and improve quality of patient care. Aim: The aim of this study is to compare the ultrasound guided technique with the traditional blind anatomical landmark technique for internal jugular vein cannulation in terms of speed of cannulation, success rate, failure rate, and the complication rate. Materials and Methods: This is a prospective randomized double-blinded study in which 40 patients of either sex posted for elective major surgeries of the age group 20 – 70 years were allocated into two groups Group A- Ultrasound guided technique and Group B-Traditional blind anatomical landmark technique. Time taken to locate and complete cannulation, number of attempts taken, failure and complications were recorded. Results: The time duration taken to locate the vein with the pilot needle and total access time significantly faster in group A. The group A had 100% success rate of cannulation with maximum of first attempt itself without any failure and complications. Conclusion: Ultrasound guidance for internal jugular vein cannulation technique is Quicker and Safer when compared with the traditional blind anatomical landmark technique and helps in improving quality of patient care. Key Words: Ultrasound, internal jugular vein cannulation, central venous access.
INTRODUCTION Central venous catheters are commonly used for haemodynamic monitoring, giving vasopressors, cytotoxic drugs, sampling blood, fluid resuscitation, massive transfusion and parenteral nutrition. Internal jugular venous access is usually achieved by the traditional blind anatomic landmark technique. In the traditional technique, rates of major and minor complications can be as high as 10%. They depend on the experience of the operator, the technique followed, the access site chosen, and the condition of the patient. Ultrasound guided central venous access is a useful application of real-time ultrasound technology in the field of Critical care and Anaesthesiology with better outcome.
MATERIALS AND METHODS A prospective randomized double blinded study was conducted at the Institute of Anaesthesiology and Critical care, Rajiv Gandhi Govt. General Hospital, Chennai in the patients posted for elective major surgeries. Institutional ethical committee approval was obtained prior to the initiation of the study. Written informed consent was obtained from all the patients included in the study.40 patients of either sex posted for elective major surgeries of the age group 20 – 70 years were randomly allocated into two groups (A and B – 20 patients each )
Selection of cases: Elective patients posted for major surgeries requiring invasive monitoring and need inotropic support or massive blood transfusion Exclusion Criteria: Patients not included were previous Coagulopathy, previous subclavian vein cannulation, iv drug abuse cases, vascular thrombosis, Obvious neck and chest deformities Procedure: Central venous cannulation planned as preinduction period. Routine Standard monitoring for patients connected inside the operating room.Patient explained about the procedure in the preoperative period,iv access with 18 G venflon achieved.After Premedication with iv Inj. Midazolam 0.05mg/kg, Inj. Fentanyl 1mcg/kg, Position – 15 * Trendelenburg position with a small bed roll between the shoulder blades, head turned to the contralateral side, arms kept to the side. Right neck region exposed, cleaned and draped.1% lignocaine infiltration 3ml at the appropriate site of skin puncture. Two persons were required. One was the Operator who did the cannulation and probe adjustments. Second was the Observer who was recording the parameters and helped in holding the probe during cannulation. The Operator underwent basic ultrasound training for 2weeks in the radiology department. Ultrasound guided technique: USG machine- Sonoray portable machine with colour and PW Doppler, with 10 MHz Linear probe. Probe covered with a sterile cover drape, a sterile gel pack is used. USG Image orientation determined Points to differentiate between artery and vein. Internal jugular vein is
After centering the vein on the screen.16 G needle with 5cc syringe, loaded with heparin saline kept under the middle of the probe. Ascertain the point of entry and the trajectory of the needle. The needle is introduced under guidance of USG 2-dimensional image. The anterior wall of the vein is seen compressed as the needle advances. Venipuncture-Needle tip seen in the middle of the IJV lumen-Free aspiration of dark venous blood confirmed. Guide wire cannulation done without displacing the needle tip from the middle of the lumen Position of the guide wire inside the IJV is seen in the longitudinal axis by adjusting the probe. Routine steps of Seldinger technique followed for Catheter insertion. Traditional blind anatomical landmark technique: Surface marking – At the apex of the triangle formed by the two heads of sternocleidomastoid muscle. A 22 G, 2- inch pilot needle mounted on a 5 cc syringe filled with heparin saline was introduced with the needle bevel up. The path of the needle was towards the ipsilateral nipple. The needle was advanced during expiration with gentle aspiration. After venipuncture, the depth and direction of the pilot needle assessed. A 16 G needle mounted on a 5 cc syringe filled with heparin saline was introduced in the same direction Seldinger’s technique of guidewire insertion and cannulation done. Parameters observed and recorded:
Statistical Analysis: Mean and standard deviation were estimated for the various parameters in each group. The mean values were compared by student’s independent ‘t’ test. Proportion and variables from each study group were compared by Pearson’s Chi-square test and Fischer’s exact test. In this study, ‘p’ value < 0.05 was considered as level of significance. RESULTS The time taken to locate the internal jugular vein by pilot needle in Group B was significantly longer than by using the ultrasound probe in Group A. The average time taken with the 16 G needle to hit the vein was only 8.5 sec in Group A when compared to 14.05 sec in Group B. The total access time thereby was relatively quick in the Group A. Group A: USG Group B: Landmark Table 1: Time duration to locate the IJV with pilot needle, 18G needle, and total access time
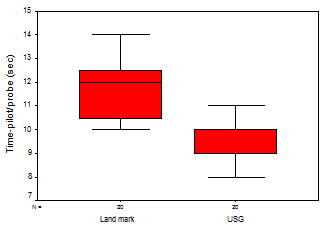
Figure 1: Time duration for Pilot needle / probe to locate IJV
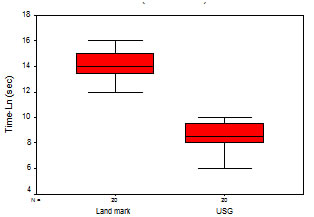
Figure 2: Time duration to locate the IJV with 16G needle
The time was noted from the point of skin contact of the 16 G needle till the free aspiration of dark venous blood confirmed the location of IJV during the final attempt that resulted in successful cannulation. Denys et al (40) – In this study, the average skin to vein time was 9.8 sec (2 to 68 sec) by the Ultrasound approach and 44.5 sec (2 to 1,000 sec) by the Landmark approach (p < 0.001). In our study the results were in concurrence with the above study, the Ultrasound group required considerably less time ( 8.50 +/- 1.19 sec ) to locate the IJV with the 16 G needle when compared to the Landmark group ( 14.05 +/- 1.05 sec ) and this was found to be statistically significant (p= 0.001 )
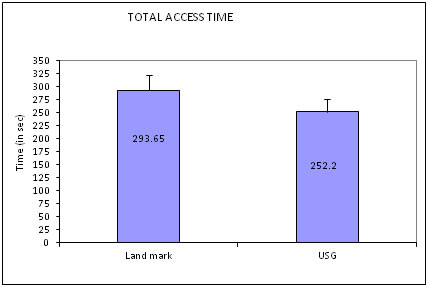
Figure 3: Total access time
The total time taken to successfully cannulate the IJV was recorded from the point of skin contact of the 18 G needle till the successful insertion of triple-lumen catheter was confirmed by the free aspiration of dark venous blood. Troianos et al (48) – In this study, there was significant reduction in the time taken for cannulation in the Ultrasound group 61 sec ( 15-180 sec) when compared to the Landmark group 117 sec (8-400 sec) Gratz et al (47) – In this study, there was significant reduction in the time taken for cannulation in the Ultrasound group 109 sec (6-470 sec) when compared to the Landmark group 226 sec (5-1200 sec) In our study also, the Ultrasound group required less time for central venous access ( 252.2 +/- 60.97 sec) When compared to the Landmark group ( 293.65 +/- 65.25 sec ). There was considerable delay in the Landmark group due to various factors like inadvertent artery puncture, compression of artery puncture, haematoma obscuring anatomy, missed attempts, difficulty in cannulation, failure of cannulation. The difference in the total access time of the two groups was found to be statistically significant. But the difference in the values when compared to the previous studies was probably due to the difference in definitions for total access time in the protocol and the differences due to the operator’s experience in the various studies. Number of attempts: Out of 20 patients in Group B, only 10 were cannulated in the first attempt.All the 20 patients in Group B had successful cannulation at first attempt itself. In Group B, one case was taken as failure since it was cannulated at 4th attempt.
Table 2: Total number of attempts
c2=13.3 P=0.004 significant The total number of attempts required to successfully cannulate the IJV including the missed attempts were recorded. Troianos et al (48) – In this trial, the mean number of attempts required in the Ultrasound group was less 1.4 ( +/- 0.7 ) and more in the Landmark group 2.8 ( +/- 3.0 ) Gratz et al (47) – In this trial, the mean number of attempts required in the Ultrasound group was less 1.35 (1-4) and more in the Landmark group 2.8 (1-10). Verghese et al (54) – In this trial, the mean number of attempts required in the Ultrasound group was less 1.3 (+/- 0.6) and more in the Landmark group 3.3 (+/- 2.8). In our study it was found that in the Ultrasound group, cannulation was successful at first attempt in all the 20 patients. In the Landmark group, only 10 patients were cannulated at first attempt, 8 patients required 2 attempts, 1 patient required 3 attempts, 1patient required 4 attempts (which was a case of failure to cannulate). The number of attempts included the missed attempts, attempts in which inadvertent artery puncture occurred and the attempts in which IJV was hit but cannulation could not be done because of needle tip displacement. The difference was statistically significant (p= 0.003). The more number of attempts with the 16 G needle significantly increased the risk of complications in the Landmark group.
Table 3: Failure of IJV cannulation
c2=1.02 P=0.31 not significant The failure was defined in various terms in the different studies. Hind et al (57) – The rate of failed catheter placement was less in the Ultrasound group (1.7%) when compared to that oof Landmark group (22%) NICE Study 2002 UK (56) – It was found that Ultrasound guidance was associated with reduced risks of failed catheter placements (56% reduction in the risk, 95% CI, 67% to 94%, p < 0.001) Failure was defined as procedure during which venipuncture was unsuccessful or cannulation was unsuccessful after 3 consecutive attempts with the 18 G needle or if the operator was unable to cannulate for more than 30min or the development of significant haematoma (> 2cm in any dimension ) due to artery punctue. Failure was followed by attempt to cannulate the left IJV by Central approach. In our study, the Landmark group had a siqnificant failure rate of 5% when compared to the Ultrasound group 0% (c2Fisher exact test P=0.05 significant). Complication: In this study, acute complications of central venous cannulation were recorded. There were incidence of Subclavian artery puncture in 4 patients. Group A patients had no complications.
Table 4: Complications during the cannulation
Fisher’s exact test =c2Fisher=4.44 P=0.04 significant
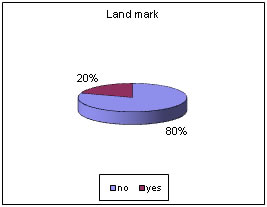
Figure 4: Complication rate
Complications were probably due to the existence of normal anatomic variations, positioning errors and increased number of attempts with the 18 G needle. Troianos et al (48) – In this study, there was reduced incidence of carotid artery punctures in the Ultrasound group (1.4%) when compared to the Landmark group (8.43%). Hind et al (57) - In this study, the relative risk of complications using the Ultrasound was 43% less than the risk of using the Landmark technique. Verghese et al (54) – In this study, the carotid artery puncture rate was 0% in the Ultrasound group when compared to 25 % in the Landmark group. In our study, the major complication we came across was the carotid artery puncture. The Artery puncture rate was 0/20= (0%) in the Ultrasound group when compared to 4/20 = (20%) in the Landmark group. All the inadvertent artery punctures (with the 18 G needle) involved the Carotid artery in the Landmark group and there were no artery punctures during the Ultrasound guided cannulation. This complication was found to be statistically significant group (c2=4.73 P=0.01 significant). The second major complication was Haematoma formation due the artery puncture. The Haematoma rate was 0/20= (0%) in the Ultrasound group when compared to 4/20 =(20%) in the Landmark group. Resulted in haematoma formation obscuring the anatomy inspite of the compression given and led to cannulation of the Left IJV (defined as Failure ).But the incidence of haematoma was not statistically significant ( c2Fisher exact test P=0.11 not significant )
DISCUSSION Ultrasonography clarifies the relative position of the needle, the vein and it’s sorrounding structures. USG allows the user to predict variant anatomy and to assess the patency of the target vein.. Ultrasound guided technique takes less time to locate the SCV, less number of attempts to cannulate SCV facilitates speedy cannulation, with significantly less number of complications and 100% success rate. The discomfort to the patient resulting from multiple attempts and switching sites because of unsuccessful cannulations is avoided in the USG technique. The advantages of ultrasound guidance for central venous cannulation is making it more difficult to justify not using this technique in all patients, when the facility is available. Ultrasound assistance is a potential useful backup technique after failed attempts of blind cannulation and for patients in whom cannulation is likely to be difficult and complications could be serious.
CONCLUSION This study concluded that Ultrasound guidance for internal jugular vein cannulation technique is Quicker and Safer when compared with the traditional blind anatomical landmark technique and helps in improving quality of patient care.
REFERENCES
|
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
 Home
Home