Official Journals By StatPerson Publication
|
Table of Content Volume 6 Issue 3 - June 2018
Comparative study of the analgesic efficacy of rectal tramadol versus intravenous tramadol for inguinal hernia repair surgery
Original Research Article
Yogesh Padol1, Shilpa Gaikwad2*, Jyotsna Paranjpe3
1JR3, 2Associate Professor, 3Professor and HOD, Department of Anaesthesiology, Bharati Vidyapeeth University Medical College and Hospital, Sangli, Maharashtra, INDIA. Email: sunshineshilpa@gmail.com
Abstract Background: Pain in the perioperative setting plays a significant role in delaying an otherwise successful recovery. Tramadol is an atypical opioid having central as well as peripheral analgesic action. We compare the effects of tramadol given by two different routes, intravenous and rectal, in terms of analgesic efficacy and duration as well as its side effects in inguinal hernia repair surgeries. Material and Methods: Sixty adult male patients of ASA grade I and II posted for inguinal hernia repair surgeries were randomized to receive either rectal tramadol (2 mg/kg) (n=30) Group A or intravenous tramadol (2 mg/kg), maximum 100 mg (n=30), Group B, after the induction of anesthesia and half hour before the end of surgery. Post operative Pain measurement was performed using visual analogue scale. Rescue analgesia was given when the VAS was ≥4 in the postoperative period. Complaint of nausea/vomiting was recorded during the same period. Results: Duration of postoperative analgesia was prolonged with the rectal route compared to intravenous administration of tramadol (240± 40 min vs 180 ± 60min). Side effects like nausea and vomiting were lower with the rectal route as compared to intravenous route. Conclusion: Efficacy and safety with rectal route of tramadol was morecompared to the intravenous route of Tramadol for the inguinal hernia repair surgery. Key Words: Analgesia, Inguinal hernia, Intravenous, Rectal, Tramadol.
INTRODUCTION Most patients who undergo surgical procedures experience acute postoperative pain. Many preoperative, intraoperative, and postoperative interventions and management strategies are available for reducing and managing postoperative pain.. Inadequately controlled pain negatively affects quality of life, function, and functional recovery, the risk of post-surgical complications, and the risk of persistent postsurgical pain. The World Health Organization and International Association for the Study of Pain have recognized pain relief as a human right. Uncontrolled acute pain may be associated with the development of chronic pain with reduction in quality of life. The main advantages of effective postoperative pain management include patient comfort and therefore satisfaction, earlier mobilization, fewer pulmonary and cardiac complications, a reduced risk of deep vein thrombosis, faster recovery with less likelihood of the development of neuropathic pain. For decreasing postoperative pain different methods and medicines are used. Tramadol is atypical opioid that have moderate affinity for mu receptor and weak kappa and delta opioid receptor affinity. In addition mu opioid agonist effect, tramadol enhances the function of spinal descending inhibitory pathway by inhibition of neuronal reuptake of nor epinephrine and serotonin as well as pre-synaptic stimulation of serotonin release. Tramadol is available in all formulations i.e. oral, injectable (intramuscular, intravenous, intrathecal) and rectal. Tramadol used by different routes such as intravenous, intramuscular, rectal or local infiltration etc. have analgesic efficacy with different duration and variable incidence of side effects. We attempted to compare rectal tramadol 100mg versus intravenous tramadol 100mg for postoperative analgesia for inguinal hernia repair surgeries.
AIM AND OBJECTIVES We aimed our study with following aims and objectives Primary aim: To evaluate the analgesic efficacy of single dose of intravenous tramadol 2 mg/kg versus rectal tramadolin the form of suppositories for post operative analgesia in inguinal hernia surgery. Secondary aim: To compare both the routes of drugs with respect to their hemodynamic effects and adverse effects.
MATERIAL AND METHODS After obtaining approval from Ethical Committee and Written informed consent from the patients, the prospective randomized clinical study was carried out on 60 male patients admitted to a tertiary health care center to undergo inguinal hernia repair surgeries from July 2016 to Jan 2107. Inclusion Criteria: Age group of 20 to 50 years, elective surgery, ASA I or II physical status male patients. Exclusion Criteria: Patient refusal, ASA grade III/IV, Renal dysfunction, Liver dysfunction Bleeding disorder. With complete preoperatively evaluation and all routine investigations, patients were randomly divided by lottery method into two groups of 30 each as group A or group B. Group A includes patients receiving 100 mg Tramadol rectal suppository and Group B includes patients receiving 100 mg Tramadol intravenously. Also preoperatively patients were explained about visual analogue scale (VAS), a 10 cm line with 0 cm equaling no pain and 10 cm worst pain ever felt. After confirmation of fasting period before anaesthesia, patients were taken in operating room and catheterized for urineand then all standard monitors like Pulse oximeter, Non invasive blood pressure, E.C.G were attached and all parameters noted. Patients were premedicated with standard dosages of inj Ondansetron 0.1mg/kg, 30 minutes prior to surgery. Patients were given sub arachnoid block with injection bupivacaine ( hyperbaric )0.5% 3.2cc at L4-L5 level using 25 G needle to achieve appropriate level of anesthesia up to T8 -T6.After receiving sub arachnoid block, group A patients received rectal tramadol in the form of suppository and group B patient received intravenous tramadol 100 mg intravenously and slowly. After the completion of surgery patients were shifted to Post Anaesthesia Care Unit and all parameters noted. Post operatively time of first onset of pain noted. Also VAS score noted at 1, 2, 4, 6, 8, 10 and 12 hour. At VAS score of 4 or more rescue analgesic had given with injection Diclofenac 75 mg intramuscularly. During post operative period vital parameters like pulse, blood pressure, respiration and side effects like nausea, vomiting, heart burn, local rectal site burning or discomfort noted in both group of patients. Statistical Analysis: The data entered in Microsoft Excel data sheet and analysed using SPSS 22 version software. Categorical data represented in the form of frequencies and proportions. Chi -square used to analyse qualitative data. Continous data reprensented as mean and standard deviation. Paried T test was the test of significance for paired data. p value < 0.05 was considered as stastically significant. OBSERVATION AND RESULTS
Table 1: Demographic parameters
ASA: American society of anaesthesiologist, SD: Standard Deviation The demographic parameters like age, weight, ASA and duration of surgery were comparable in both groups.
Table 2: Intraoperative and postoperative haemodynamic monitoring in group a and group b patients monitoring of heart rate
GROUP-A Rectal Tramadol, GROUP-B Intravenous Tramadol, NS: Not Significant
Table 2a: Monitoring of MAP
Table 2b: Monitoring of Respiratory rate
P.R – Pulse Rate, MAP- Mean Arterial Pressure, R.R – Respiratory Rate
Table 3: Comparison of VAS score between Rectal tramadol versus intravenous tramadol
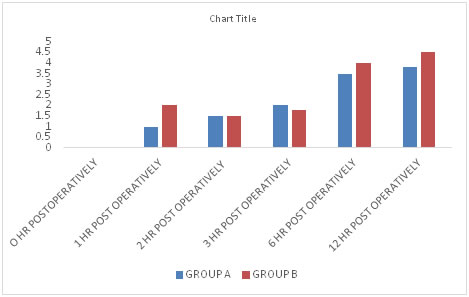
Figure 1:
VAS scores in both the groups was < 3 till 3 hrs in postoperative period indicating effective analgesia produced by both the study drugs. While on intergroup comparison, we found that Mean VAS score was higher in Group B compared to Group A, and the difference was statistically highly significant. It indicated that onset, duration and quality of postoperative analgesia was better in group A. 6 patients in group B and one patient in group A needed rescue analgesia with Inj. Diclofenac (75 mg im) due to higher VAS score at 4 hrs postoperatively.
Table 4: First onset of pain
Table 5: No. of patients requiring rescue analgesia
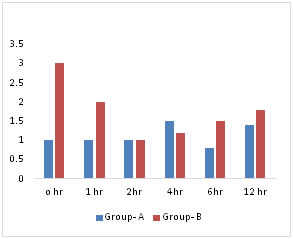
Four patient in group A and 12 patients in group B (40%) received rescue analgesia when recorded VAS score was > 4 in the early postoperative period. Results = Group B patients required more frequently rescue analgesic after 4 hrs postoperatively as compared to group A patients Graph-2 Comparison of side effects of Rectal Tramadol versus Intravenous Tramadol Figure 2:
Table 6:
RD: Respiratory depression, PDPH: post dural puncture headache Result- Rectal route of Tramadol has less side effects as compared to intravenous route Side effects noted were in the form of post operative nausea- vomiting (PONV). The incidence of nausea and vomiting was higher (43.5%) in Group B than Group A (16%).
DISCUSSION Amongst opioids, Tramadol has less side effects.In our study we had compared intravenous versus rectal tramadol for postoperative analgesia in inguinal hernia patients. The drug was received by the patients half hour after sub arachnoid block and before the end of surgery. Tramadol exists as the racemic (1:1) mixture of the (+) and (-)-enantiomer. It has a multimodal mechanism of action as on the one hand the (+) and (-)-enantiomer act on the serotonin and noradrenaline reuptake, and on the other hand the O-desmethyl metabolite of tramadol (called M1 or ODT) acts on the µ-opioid receptor. This implies that the analgesic mechanism of action of tramadol includes both non-opioid components, i.e., noradrenergic and serotonergic components, and opioid components. Tramadol is a centrally acting analgesic with a multimode of action. Tramadol is used to treat both acute and chronic pain of moderate to severe intensity. The analgesic effect of tramadol appears to be produced in a multimodal mechanism involving the µ-opioid system, the noradrenergic system, and the serotonergic system.. Tramadol is suitable to treat post operative pain, but after intravenous route, peak concentrations are reached rapidly and this has been associated with post operative nausea and vomiting. Rectal administration of Tramadol is an alternative in this situation. A rectal dose of 2.0 mg / kg Tramadol is used, therefore a dose of 100 mg was used in our study as suppository.We had compared haemodynamic monitoring in both the group of patients, it showed that patient with rectal suppository had minimal changes in haemodynamic parameters as compared to those who received intravenously. It also showed that there was high incidence of nausea and vomiting in intravenous group as compared to rectal suppository group of patients.1,4 In our study, we compared tramadol suppository with intravenous tramadol. In intravenous group 6 patients had mean VAS score 4 after 4 hrs postoperative, and after that rescue analgesia was given in the form of inj Diclofenac 75 mg im as compared to 1 patients in rectal tramadol suppository group. This shows that suppository group of tramadol had less mean VAS score as compared to intravenous group of tramadol and this difference was statistically significant. It also showed rectal group of tramadol had less side effect as compared to intravenous group of tramadol. Hina N. Gadani et al1 studied analgesic efficacy of rectal tramadol against intravenous tramadol for adult tonsillectomy. They found that after i.v. and oral administration, peak concentrations are reached rapidly, and this has been associated with postoperative nausea and vomiting. This limits the use of tramadol as a postoperative analgesic by intravenous route especially in day surgery. In their study they found only 60% of the patients required rescue analgesia in rectal group within 10 h of the postoperative period. Another 40% of the patients in rectal group did not require rescue analgesia at all, which was not seen with intravenous group. In intravenous group, 100% of the patients required rescue analgesia within 10 h of the postoperative period. Analgesia was significantly prolonged in rectal group as compared to intravenous tramadol group. Lotfalizade et al2 studied diclofenac suppository against intravenous tramadol injection and combination of these two for analgesia in caesarean section. duration of analgesia in the group of combination of tramadol and diclofenac was 66.8 min more than diclofenac suppository alone that was not statistically significant Giorgi M. et al3 showed that after rectal administration, tramadol was detected from 5 minute up to 10 hour. After rectal suppository, though absorption of the active ingredient was rapid, its metabolism quickly transformed the parent drug to high levels metabolites such as N-desmethyl-tramadol (M2) and, O-didesmethyl-tramadol. In our study the mean duration of analgesia i.e. mean duration of first onset of pain in rectal tramadol group was longer as compared to in intravenous tramadol group. Petron D et al4 studied that after intravenous administration of tramadol peak concentrations are reached rapidly. This has been associated with postoperative nausea and vomiting. This limits the use of tramadol as a postoperative analgesic, especially in day surgery. In their study demonstrated that a slower titration rate of tramadol HCl improves tolerability in patients who previously discontinued therapy due to nausea and/or vomiting. This study also demonstrates that the rate of titration of tramadol HCl rather than the target dose is the major determinant of tolerability. Zwaveling J et al5 showed the pharmacokinetics of rectal tramadol in postoperative paediatric patients. They found that difference in tramadol clearance between children and adullts after rectal administration in contrast to iv administration no difference in clearance between the two age group was found.They studied that after the 2 mg/kg dose of tramadol, it increases therapeutic concentration and it could be correlated with the duration of analgesia. Their study also showed that after rectal administration, tramadol was well absorbed and showed a relatively low variability in absorption and clearance. Hale Yarkan. et al.,6 in their study evaluated the efficacy and quality of recovery with intravenous paracetamol versus tramadol for postoperative analgesia after adenotonsillectomy No statistically significant difference was found in postoperative pain scores in either group. They found that number of patients who received rescue analgesia and time to administration of rescue analgesia were similar in both groups. Dejonckheere M et al,7 compared intravenous tramadol to propacetamol for postoperative analgesia following thyroidectomy. More patients complained of nausea and vomiting during the first two hours following injection of tramadol as compared to propacetamol. Pendeville et al.8 compared the postoperative analgesia between paracetomol and tramadol for day care tonsillectomies in children and showed postoperative pain scores in recovery, numerical pain scale in the ward and at home, and rescue analgesic use were significantly lower in the tramadol group. In urosurgery, Aghamir et al.9 compared proparacetamol and tramadol after urologic open surgeries and found proparacetamol useful, but inadequate in cases of severe pain necessitating supplementary analgesics. Patients with severe pain were more in the Propacetamol group than the tramadol group postoperatively. Kela et al.10 compared the efficacy of intravenous paracetamol versus intravenous tramadol in the postoperative period in cardiothoracic surgery and found 10.0% of the subjects in paracetamol group and 13.3% out of total cases in tramadol group suffered nausea and vomiting, side effect of an intravenous administration of tramadol. V. Khazin et al11 studied postoperative analgesia with rectal tramadol and indomethacin for diagnostic curettage and early termination of pregnancy. They found rectal tramadol provides superior postoperative analgesia with minimal adverse effects. Dr. Joshi V.S. et al12 studied rectal suppository of tramadol and diclofenac in caesarean section. However they found that rectal suppository of diclofenac is better alternative for postoperative analgesia in cesarean section as compared to tramadol. Thus various oral, rectal and parenteral formulations of tramadol are available. The rectal route is an alternative and also no significant side effect was found in suppository group. Thus, rectal suppository of Tramadol is better alternative for postoperative analgesia in inguinal hernia surgery patient as compared to intravenous tramadol. Our all above results are comparable to previous studies. Limitations scope: Further Studies on large number of patients and both the sexes and on high risk group patients needed to be done using tramadol as analgesic by intravenous and rectal route.
CONCLUSION From the above study it can be concluded that intravenous Tramadol and rectal Tramadol, both provide satisfactory post operative analgesia. Rectal route of tramadol causes minimal side effects with longer postoperative analgesia than intravenous tramadol in the inguinal hernia patients.
REFERENCES
|
|
 Home
Home