Official Journals By StatPerson Publication
|
Table of Content Volume 6 Issue 3 - June 2018
Comparison of post-operative analgesic efficacy of bupivacaine and ropivacaine using ultrasound guided oblique subcostal transverse abdominis plane block in open cholecystectomy under general anaesthesia
Original Research Article
N Sumathi1, A Ganesh2*, S Balasubramaniam3
1,2Sr. Assistant Professor, 3Resident, Department of Anaesthesiology, Rajiv Gandhi Government General Hospital, Madras Medical College, Chennai, Tamil Nadu, INDIA. Email: drganesh78@gmail.com
Abstract Background: Cholecystectomy involves upper abdominal incision with considerable postoperative pain. Adequate postoperative analgesia has to be provided to prevent major pulmonary complications in the postoperative period. Ultrasound guided oblique subcostal Transverse abdominis plane block has been extensively used to provide adequate analgesia without haemodynamic complications. Aim: To compare the post operative analgesic efficacy of Inj.Bupivacaine 0.25% and Inj.Ropivacaine 0.2% in Ultrasound guided Bilateral Oblique Subcostal Transverse Abdominis Plane block for patients undergoing open cholecystectomy under general anaesthesia. Materials and Methods: The study was done on 60 patients who underwent bilateral oblique subcostal Transverse abdominis plane block for open cholecystectomy surgeries under general anaesthesia. Group A: 30 patients given Inj.Bupivacaine 0.25%, 40 ml (20ml on each side). Group B: 30 patients given Inj.Ropivacaine 0.2%, 40 ml (20ml on each side). Results: The mean visual analog score was less in group A when compared to group B from 30 minutes to 8 hours time intervals, which also has statistical significance. The mean duration of analgesia was longer in group A than group B. Both groups had significant reduction in opioid usage for alleviationg postoperative pain.Both the group had stable intraoperative and postoperative hemodynamics when mean HR, SBP, DBP and MAP were monitored. Conclusion: It is concluded that postoperative analgesia wih Inj.Bupivacaine 0.25% is more effective when compared to Inj.Ropivacaine 0.2% in prolonging the duration of Ultrasound guided Oblique subcostal transverse abdominis block. Intraoperative and Postoperative hemodynamics were maintained well in both the groups. Key Words: Oblique subcostal transverse abdominis block, open cholecystectomy postoperative analgesia.
INTRODUCTION Ultrasound guided Oblique subcostal transverse abdominis block plays important role in postoperative analgesia of Open Cholecystectomy patients. The ultrasound‑guided transversus abdominis plane (TAP) block involves local anaesthetics infiltration into the plane between the transversus abdominis and the internal oblique muscles to block the thoracolumbar intercostal nerves which are derived from anterior divisions of spinal segmental nerves T6 to L1. In “Oblique Subcostal Transverse plane approach” needle is inserted along the oblique subcostal line from the xyphoid process toward the anterior part of the iliac crest to give analgesia to both supra and infra umbilical surgeries. Hence this study targets to give postoperative pain relief for those patients undergoing open cholecystectomy.
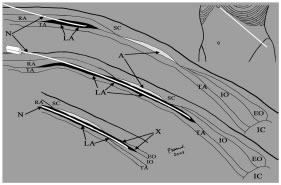
MATERIALS AND METHODS The study is a Prospective randomized study. The study was duly submitted before the ethical committee of our Institution and the Ethical Committee approval was obtained. The study was done on 60 patients who underwent open cholecystectomy under general anaesthesia. Inclusion Criteria: Age - 18 years to 60years,Sex - Both male and female, Weight - BMI < 35 Kg/m2, ASA - I, II, Surgery -Elective open Cholecystectomy, Mallampati scores : I and II, informed consent. Exclusion Criteria: Not satisfying inclusion criteria, Patient’s refusal to participate in the study, Allergy to local anaesthetics, Coagulopathy, Systemic or local sepsis, Pregnancy, Patients with severe cardiovascular, respiratory, renal, hepatic diseases, H/O seizures and any neurological deficit Study Groups: 60 patients who needs to be operated for Elective Cholecystectomy will be given Bilateral Oblique subcostal Transverse abdominis plane block randomly assigned into two groupsGroup A: 30 patients given using Inj.Bupivacaine 0.25%. 40 ml (20ml on each side). Group B: 30 patients given using Inj.Ropivacaine 0.2%. 40 ml (20ml on each side). Standardized general anesthetic regimen employed for all the 60 patients which consists of Inj.Glycopyrrolate 0.2 mg i.m and Inj.fentanyl 2mcg/kg i.v. The patient was then preoxygenated with a 100 % O2 for 5 minutes. Induction was done with inj.Thiopentone 5mg/kg and muscle relaxation with Inj.Atracurium 0.5mg/kg. The patient was then ventilated with a N2O : O2 (50% : 50%) along with Sevoflurane 2% for a time interval of 3 minutes. Endotracheal intubation was then done with the cuffed endotracheal tube of appropriate size. Maintenance of anaesthesia was attained with N2O :O2 in the ratio of 50 % : 50 % along with Sevoflurane1-1.5% and Inj.Atracurium 0.1mg/kg is given at every 20 minutes interval with intraoperative non-opioid analgesia of paracetamol (15–20 mg/kg). Ultra sound guided ‘OSTAP’ technique: Foremost important step in doing Ultrasound guided nerve block is maintanence of Strict aseptic precaution. Visualising the ultrasonographic image of Transverse abdominis plane near costal margin where only two muscle bellies, (i.e.) Transverse abdominis muscle belly seen immediately behind Rectus abdominis muscle is the important step. Patient put in supine position maintained in general anaesthesia. Once probe applied and Transverse abdominis muscle belly seen below the costal margin, Superior epigastric vessels can be visualized using colour or power Doppler, 18G needle is inserted through rectus abdominis muscle and enough care must be excersied in avoiding the Superior epigastric vessels. Once needle tip is identified in the plane Local anaesthetic injectate of 0.5ml to 1ml is injected to see the hydrodissection and needle is advanced as explained by Prof. Hebbard in his description. Figure 1: Upper right diagram showing the oblique plane along the costal margin, following the needle direction for oblique subcostal TAP block. In the upper left figure, the needle has entered the TAP posterior to rectus abdominis muscle (RA), and the local anesthetic (LA) hydrodissection done. In the middle figure, the needle is passing down the hydrodissection and continuing in the plane after being rotated to 180 degrees.(A) denotes aponeurotic area. In the lower diagram, the hydrodissection and needle have incorrectly passed (X) between internal oblique muscle (IO) and external oblique muscle (EO). TA indicates transversus abdominis muscle, IC indicates iliac crest, SC indicates subcutaneous tissue. Technique of block: An in plane image was obtained and 18 G Tuohy needle was inserted through the rectus muscle 1 cm medial to the probe. Once the tip of the needle was visualised in the plane, 20 ml of Inj.Bupivacaine 0.25% (if patient is under group A) or Inj.Ropivacaine 0. 2% (if patient falls under group B) administered in incremental volumes depending on the group. The drug was injected along the oblique subcostal line, extending inferolaterally from the xiphoid process towards the anterior part of the iliac crest. And on the contralateral side drug is injected in the same manner. All patients were given minimal amount of Positive end expiratory pressure PEEP of 5 cm H2O once pneumoperitoneum has been created. Patients were put in reverse trendelenburg position from supine position in slow increments of 5degrees monitoring the hemodynamics. Open cholecystectomy done by making subcostal incison (Kocher’s incision) of 8-10cm leng. Intra operative vitals monitored and recorded as indicated in master chart. Towards the end of the surgery patients were slowly weaned from Sevoflurane by monitoring end tidal gas monitoring and ventilated with N2O :O2 in the ratio of 50 % : 50 % and reversed with Inj.Neostigmine 50micrograms /kg and Inj.Glycopyrrolate 10micrograms /kg and extubated once objective and subjective criteria for extubation satisfied. And they are observed in recovery room for 15min and shited to postoperative ward. Heart rate, Systolic blood pressure, Diastolic blood pressure, Mean arterial pressure were measured at baseline and at intervals of 1,5,10,15,30,45,60,75,90 min and 1,2,3,4,5,6,7,8,9,10,11,12 hours ( till the time of post-operative rescue analgesia). Pain scoring done by asking the patient to mark the severity of pain from 0 to 10.Vitals and visual analog score were then monitored immediately and also post operatively at regular intervals in the post-operative ward. Pain assessment was done using VAS score. VAS score >3 indicates pain. Duration of effective analgesia was defined as time interval between the time ‘Oblique Subcostal Transverse abdominis block’ given to the time of reach VAS score >3. When the VAS score was greater than 3, the patients were given rescue analgesic of Inj.Paracetamol 15-20mg/kg of iv infusion and if the patient complains of pain even after 30 min of starting Inj.Paracetamol, Inj.Tramadol 50-100mg i.m given. Parameters Monitored
OBSERVATION, RESULTS AND ANALYSIS Table 1:
Table 2:
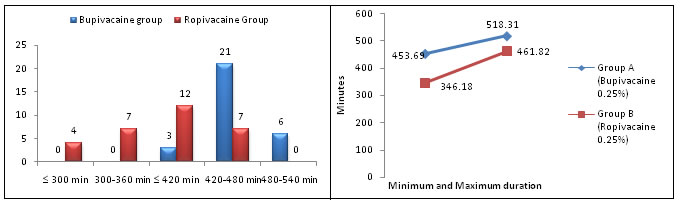
Mean duration of analgesia for group A is 486 ± 32.31 min. Mean duration of analgesia for group B is 404 ± 57.82 min. The two-tailed P value is less than 0.0001. By conventional criteria, this difference is considered to be extremely statistically significant.
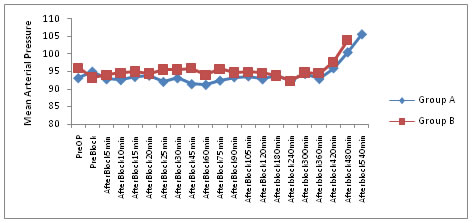
Figure 2 and Figure 3: Duration of Analgesia
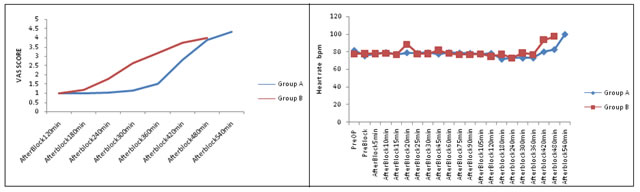
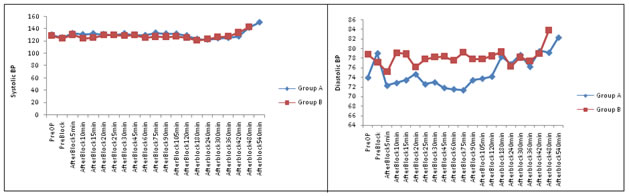
Figure 4: Mean VAS score distribution Figure 5: Mean Heart rate distribution By conventional criteria the association between the intervention groups (Inj.Bupivacaine group and Inj.Ropivacaine group) and VAS score is considered to be statistically significant since p < 0.05 as per unpaired t test. In group A mean heart rate varies from 71.77 ± 3.14 bpm to 100 ± 2.65. And in group B mean heart rate varies from 73.1 ± 6.45. to 97.25± 6.26. Using unpaired t test overall p value is not statistically significant (significant value of p < 0.05 in unpaired t test). It shows no significant difference between two groups. Figure 6: Mean SBP distribution Figure 7: Mean DBP distribution In group A mean ‘Systolic blood pressure’ varies from 122.43 ± 7.43 mm Hg to 150 ± 3.2 mm Hg. And in group B mean heart rate varies from 121.53 ± 7.87 mm Hg. to 143.25 ± 3.73 mm Hg. Using unpaired t test overall p value is not statistically significant (significant value of p < 0.05 in unpaired t test). It shows no significant difference between two groups. Diastolic Blood Pressure: In group A mean ‘Diastolic blood pressure’ varies from 71.4 ± 7.12 mm Hg to 82.3 ± 5.5 mm Hg. And in group B mean heart rate varies from 75.2 ± 7.86 mm Hg. to 83.88 ± 2.2 mm Hg. Using unpaired t test overall p value is statistically significant (significant value of p < 0.05 in unpaired t test). It shows significant difference between two groups. Figure 7: Mean Arterial pressure distribution In group A mean ‘Mean arterial pressure’ varies from 91.23 ± 4.5 mm Hg to 92.3 ± 3.9 mm Hg. And in group B mean heart rate varies from 92.3 ± 3.9 mm Hg to 103.88 ± 1.9 mm Hg. Using unpaired t test overall p value is statistically significant (significant value of p < 0.05 in unpaired t test). It shows significant difference between two groups.
DISCUSSION Transverse abdominis plane block is an effective means of providing pain relief. In Transverse abdominis plane there is lesser vascularity as described in the study done by Rozen WM et al ” a new understanding of the innervation of the anterior abdominal wall”. which account for longer duration of blockade. Apart from producing adequate analgesia it has various beneficial effect. It reduces the intra operative and postoperative analgesics requirements in the form of narcotics and NSAIDS. It provides faster and comfortable wake up time, helps in early ambulation, less hospital stay, thereby alleviating most of the anxiety. In our study, the demographic profile was comparable with respect to mean age, body weight and ASA physical status. We compared 60 patients who are planned for open cholecystectomy were given biilateral oblique subcostal Transverse Abdominis Plane (OSTAP) block in the group A with Inj.Bupivacaine 0.25% 20ml on each side and in the group B with Inj.Ropivacaine 0.25% 20ml on each side. The clinical technique of OSTAP blockade is done as described by Prof. Hebbared et al in his article “Ultrasound-guided OSTAP blockade: description of anatomy and clinical technique. Reg Anesth Pain Med.2010; 35: 436-41”published in A.S.R.A (American Society of Regional Anesthesia) pain medicine. The study results are similar and in consistent with other studies in reducing postoperative reduction in pain. Most studies revealed the efficacy of TAP blocks by reducing postoperative opioid requirement, lower pain scores, and/ or reduction in opioid-related side effects. A meta-analysis of 7 studies (180 cases and 184 controls) demonstrated an average reduction in 24-h morphine consumption of 22 mg in favor of TAP block patients compared with standard management. Many studies found that Ultrasound guided TAP blocks reduce pain scores in phase I recovery and at 24 h. Other studies demonstrated that US-guided TAP blocks reduce morphine consumption during phase I recovery and at 24 h, and reduce the incidence of postoperative nausea and vomiting at 30 min, when compared to systemic analgesia for patients undergoing laparotomy or laparoscopic surgery. The median visual analogue score (<3) is significantly less in both group A in which Inj.Bupivacaine 0.25% is used and in Group B in which Inj.Ropivacaine 0.25% is used. Mean duration of analgesia for group A is 486 ± 32.86 min. Mean duration of analgesia for group A is 404 ± 58.81 min. And this study results are in consistent with study done by. ”Mukherjee A and others in An observational study on a new and promising analgesic technique. In which - the study results are Median VAS score was below three in 83% of patients. No fentanyl bolus was required in 37% of patients while 50% required one or two and 13% more than two boluses. Sixty‑three percent of patients enjoyed complete analgesia (VAS < 3) for 12–18 h, and in 17%, analgesia lasted <12 h. Only one patient had episodes of nausea while all the patients had sedation score below two without any other adverse effect”
SUMMARY The following observations were made in this study. The mean visual analog score was less in Inj.Bupivacaine group when compared to Inj.Ropivacaine group from 30 minutes to 8 hours time intervals, which also has statistical significance. The mean duration of analgesia was longer in Inj.Bupivacaine group than Inj.Ropivacine group. Both produces significant reduction in opiod usage for alleviationg postoperative pain. Both the group was maintained well with good intraoperative and postoperative hemodynamics when mean HR, SBP, DBP and MAP are monitored. Hence, Ultrasound guided Oblique subcostal transverse abdominis block with Bupivacaine is effective in postoperative analgesia of Open Cholecystectomy patients. When administered along with non-opiods like Inj.Paracetamol it provides adequate postoperative analgesia. In addition all the side effects of opioid usage like PONV,sedation,respiratory depression can be minimized.
CONCLUSION It is concluded that though haemodynamic parameters are comparable postoperative analgesia wih Inj.Bupivacaine 0.25% is more effective when compared to Inj.Ropivacaine 0.2% in prolonging the duration of Ultrasound guided Oblique subcostal transverse abdominis block.
|
|
||||||||||||||||||||||||||||||||||||||||||||||||||||
 Home
Home