Official Journals By StatPerson Publication
|
Table of Content Volume 6 Issue 3 - June 2018
Comparison between ultrasound-guided transversus abdominis plane block and conventional ilioinguinal/iliohypogastric nerve block as post-operative analgesia for unilateral open inguinal hernioplasty under spinal anaesthesia
Original Research Article
Madhuja Kanbarkar1*, Vasudha Jadhav2, Jyotsna Paranjpe3
1Jr. Resident, 2Professor, 3Professor and HOD, Department of Anesthesia, Bharati Vidyapeeth Deemed to be University and Medical College, Sangli, Maharashtra, INDIA. Email: madhuja.a.kanbarkar@gmail.com
Abstract Background: Open inguinal hernioplasty is commonly performed under spinal anesthesia. Transversus Abdominis Plane (TAP) block or ilioinguinal/iliohypogastric (IHN) block are used for postoperative pain relief in these patients. Ultrasound guided TAP blocks have better success rates. Aims and Objectives: To compare the efficacy, duration and quality of post operative analgesia between ultrasound guided TAP block and conventional IHN block after unilateral open inguinal hernioplasty under spinal anesthesia with 0.5% heavy Bupivacaine. To assess the safety of both techniques by comparing the side-effects and complications when used for post-operative pain relief. Material and Methods: After obtaining institutional ethical committee approval, total 60 adult patients of both sexes of ASA I-III undergoing open unilateral inguinal hernioplasty under spinal anesthesia with 0.5% heavy Bupivacaine were selected for the study. Patients were randomly divided in two groups, Group A (n=30) received ultrasound-guided TAP block with 20 ml 0.25% Bupivacaine while Group B (n=30) received conventional IHN block with 20ml of 0.25% Bupivacaine; both for post-operative analgesia. During post operative period other than vital parameters, quality of analgesia was assessed by Visual Analogue Scale (VAS) and time of rescue analgesia was noted. Patients were also monitored for side-effects like nausea and vomiting and complications associated with the blocks. Results: Duration of analgesia in post-operative period for group A was prolonged as compared to group B. Quality of analgesia evidenced by mean VAS scores was better with group A. No side-effects or complications were noted in both the groups. However in one case failure of ilioinguinal/iliohypogastric block was noted. Conclusion: Compared to conventional IHN block, ultrasound-guided TAP block is more effective for post-operative analgesia. Key Words: spinal anaesthesia, VAS.
INTRODUCTION Open inguinal hernioplasty is commonly performed under spinal anesthesia. A substantial component of the pain experienced by patients after hernioplasty surgery is derived from the anterior abdominal wall incision1. Post operative pain management is the key factor to decide the outcome of the patient2. A promising approach to the provide postoperative analgesia after abdominal incision is to block the sensory nerve supply to the anterior abdominal wall3,4. TAP block and INH block are popular regional anesthetic technique for post operative anesthesia after hernioplasty surgery. TAP block involves the injection of local anesthesia into the plane between the internal oblique and transversus abdominis muscle and thus giving pain relief. The technique when performed under ultrasound guidance improves the yield. TAP block provides good analgesia between T10 and L1 level (2). Because the TAP block is a blind technique, it can cause inappropriate blockades. However, the introduction of ultrasound has allowed the block to be made with great precision and has minimized errors in the blockade, due to the real-time visualization of the abdominal planes5,6. Ilioinguinal and iliohypogastric nerves arise from the first lumbar spinal root. The ilioinguinal nerve supplies the skin on the proximal, medial portion of the thigh, and the iliohypogastric nerve supplies the skin in the inguinal region. The IHN block is safe, effective and easy to perform in order to provide analgesia for a variety of inguinal surgical procedures7. There are few data available comparing IHN block with ultrasound-guided TAP block. We thus conducted a study to compare the efficacy of the ultrasound-guided TAP block and conventional IHN block on postoperative analgesia after inguinal hernioplasty surgery under spinal anesthesia.
MATERIAL AND METHODS After obtaining institutional ethical committee approval and informed written consent from study subjects, a comparative study was conducted on a predetermined sample size in a tertiary care hospital over a period of one year. Sixty adult patients between 18-60 years of age with the American Society of Anesthesiologists (ASA) I, II and III admitted for elective open inguinal hernioplasty surgery under spinal anesthesia were selected for the study. Pediatric age group, patients with ASA grade IV, those with known allergy to study drugs, renal dysfunction, liver dysfunction, unable to comprehend VAS score and bleeding disorders were excluded from the study. The enrolled patients were randomized into two groups Group A and Group B by lottery method. Patients receiving ultrasound-guided TAP block post hernioplasty were allotted to Group A and patients receiving IHN block post hernioplasty were allotted to Group B. Both the blocks were given immediately after surgery with 20 ml of 0.25% Bupivacaine. Study Procedure: Prior to the day of surgery all patients underwent pre-anesthesia check up with routine and subjective investigations as per institutional protocol.. All patients were kept nil by mouth from midnight before surgery. After receiving the study subject in pre anesthesia room, the baseline parameters were noted. The patients were explained about ‘visual analogue scale’ (VAS) and the procedure. Intravenous access was established with an 18‑gauge cannula. All the patients were premedicated with injection Ondansetron 4 mg intravenously. All emergency drugs were kept ready. Standard monitoring was used, including non-invasive arterial blood pressure (BP), ECG, heart rate (HR) and pulse oximetry. Spinal anesthesia was performed as per institutional protocol with 2.5 to 3ml 0.5% heavy Bupivacaine. Patients allotted to group A received ultrasound-guided TAP block immediately after surgery. Procedure for TAP block: The skin on the operated side was prepared using antiseptic techniques. The ultrasound probe was placed on the abdominal wall anterolateraly between the iliac crest and subcostal margin to identify the 3 muscle layers of the abdomen. The probe was then guided posteriorly to the mid-axillary line. A 22 gauge blunt ended needle was inserted perpendicularly to the mid-axillary line and in plane with the probe (in-plane). With the guidance of ultrasonography the needle was passed through the different muscle layers until the needle tip entered the layer between the internal oblique muscle and transverses abdominis muscle. Correct placement of the needle was confirmed upon injection of a saline solution into the muscle plane, which spread in the planes between the 2 muscle layers. Once correct needle placement was confirmed, 20 ml of 0.25 % Bupivacaine was injected after negative aspiration for blood. Patients allotted to group B received conventional IHN blocks immediately after surgery. Procedure for conventional IHN block: The skin on the operated side was prepared using antiseptic techniques. The anterior superior iliac spine was located and a mark was made 2 cm medial and 2 cm superior from it. After local anesthetic infiltration, a small puncture was made in the skin with a sharp needle to allow subsequent insertion of a blunt needle. The needle was inserted through the skin puncture site perpendicular to the skin. 22G 8 cm needle was advanced through the cephalolateral and inserted to touch the inner surface of the ileum. 10 ml of 0.25% Bupivacaine was administered after negative aspiration into the layers of the abdominal wall while the needle was withdrawn. Then, as the needle was advanced with a right angle, loss of resistance was felt during the passage through the external oblique, internal oblique and transversus abdominis muscles respectively and 10 ml of 0.25% Bupivacaine was administered into the muscles while the needle was withdrawn. All the patients were assessed by VAS score, in postoperative at the beginning and after 30 minutes in the recovery room; every hourly for first 12 hours and every 2 hourly for next 12 hours in the surgical ward. Post operative pain score was measured by using VAS of 0 to 10, where 0 indicated no pain and 10 most severe pain. Time taken for first demand of rescue analgesia was noted and analgesia was provided in the form of injection Tramadol 50 mg slowly intravenously if VAS score was > 3. Patients were observed for any complications like nausea, vomiting and complications associated with the blocks like local anesthetic toxicity, transient lateral femoral cutaneous or femoral nerve palsy, visceral damage (if needle was advanced too far), intraperitoneal injection, bowel hematoma, enlarged liver laceration, enlarged spleen and kidney rupture, accidental intravascular injection of local anesthetic and infection were cross examined and recorded. A questionnaire prepared was filled up as per response of patients and charts were maintained. Statistical Analysis: Data was compiled in MS-Excel. It was analyzed and expressed as mean ± SD. Intergroup comparison was done using paired t test. Statistical analysis was done by using chi square test with a significant P value of <0.05. Statistical package for social sciences (SPSS) version 22- (USA) was used for statistical analysis
OBSERVATIONS AND RESULTS Comparison of demographic values
Table 1: Comparison of Demographic Data
NS: not significant
The data in table 1 suggests that both the groups are demographically comparable. Table 2: Post-operative mean VAS score
It is evident from the Table 2 that, mean VAS scores in group A was 0 till 5 hrs in postoperative period indicating effective analgesia produced by ultrasound guided TAP block. While on intergroup comparison, we found that Mean VAS score was higher in Group B compared to Group A till 8 hours postoperatively indicating early onset of pain in group B whereas Mean VAS score was higher in Group A from 9 hours to 16 hours postoperatively indicating delayed onset of pain in Group A. The difference was statistically highly significant at 6, 7, 8, 9, 10, 11, 12, 14 and 16 hours postoperatively. It indicated that onset, duration and quality of postoperative analgesia was better in group A. However, after 16 till 24 hours postoperatively there was no significant difference in P values of mean VAS scores indicating comparable analgesia after 16 hours in both the groups. 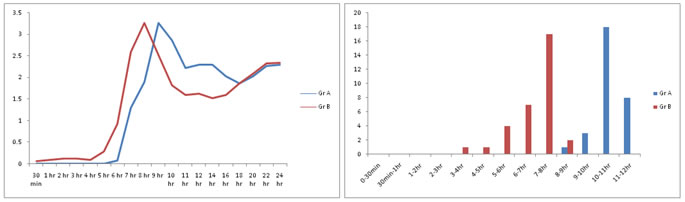 Figure 1: Mean VAS Score Figure 2: Rescue analgesia .
Table 3: Rescue analgesia demand time
Demand for rescue analgesia was earlier in group B, immediately after 2 hours of administration of block for 1 patient due to failure of the block where as first demand for rescue analgesia for group A was after 7 hours of administration of the block. 50% of patients in group B were given rescue analgesia after 8 hours where as 47% patients from Group A were given rescue analgesia after 9 hours. Analgesia for group A extended till 12 to 14 hours were as in group B by 10 hours all patients received rescue analgesia. Table 4: Complications ck
In Group A, 6.67% patients complained of post-operative nausea vomiting (PONV) where as 10% patients in group B complained of PONV. No side-effects or complications were noted in both the groups. However in one case failure of IHN block was noted.
DISCUSSION The international Association for Study of Pain defines pain as an unpleasant sensory and emotional experience associated with actual or potential tissue damage or described in terms of such damage. Pain after surgery can adversely affect both physical and physiological functions. Post operative pain management is the key factor to decide the outcome of the patient (2). Postoperative pain can prolong recovery, increase the duration of hospital stay thereby increasing health care cost. All the abdominal surgeries whether open or laparoscopic, are associated with significant post operative pain. Various methods used for post operative analgesia are parenteral opioids, NSAIDS, infiltration of local anesthetic agents, dermal patches, patient controlled analgesia and epidural catheters, etc. Peripheral nerve blocks provide effective anesthesia and analgesia in a site specific manner with the cost. All the abdominal surgeries whether open or laparoscopic, are associated with significant post operative potential for long-lasting effects. Accurate identification of target nerves and precise and adequate placement of local anesthetic are critical for performing safe and successful peripheral nerve blocks. Peripheral nerve blocks can be performed by land mark technique, under guidance of peripheral nerve stimulator or with ultrasound guidance. Nerve blocks associated with bony or vascular landmarks are more reliable and easy to perform than those dependent on surface landmarks alone. Peripheral nerve stimulators are useful tools to facilitate nerve blocks, but do not eliminate the risk of nerve injury. Ultrasound imaging allows direct visualization of all anatomical structures, the needle, and the spread of local anesthetic and is associated with an increased margin of safety and optimal block qualities(8)(9). The TAP block has been described as an effective regional anesthetic method for various surgical procedures. The ultrasonographic guidance enables exact placement of the local anesthetic between internal oblique abdominal muscle and transverses abdominis muscle. The IHN block is a popular regional anesthetic technique for surgical procedures in the sensory area of the ilioinguinal and iliohypogastric nerves. In our institute, conventional landmark guided IHN block was routinely used for post operative analgesia in inguinal hernioplsty surgeries. However TAP block is a new promising technique as post operative analgesia for inguinal hernioplsty surgeries with more efficacy and safety under ultrasound guidance (8)(9)(10)(11)(12)(13). Very few data is available on the use of ultrasound guided TAP block in comparison with conventional IHN block in patients undergoing inguinal hernioplasty. We thus conducted a study to compare the efficacy of the ultrasound-guided TAP block and conventional IHN block on immediate postoperative analgesia after inguinal hernioplasty. Various studies have compared the efficacy of TAP block for post-operative analgesia with conventional systemic analgesics in various surgeries like abdominal surgery for large bowel resection14, Caesarean delivery15, total abdominal hysterectomy16, open retropubic surgery17 and major gynecological surgical operations18. These studies have used different local anesthetic drugs with different concentrations- 40 ml of 0.375% of Levobupivacaine14, 1.5 mg/kg of Ropivacaine15,16 and 40 ml of 0.375% Bupivacaine17. All the above studies were performed under general anesthesia14,16,17 except one study that was done under spinal anesthesia15. These studies have documented that TAP block provided effective post-operative analgesia upto 24 hours compared to conventional analgesic methods. A metanalysis by Siddique et al on the clinical effectiveness of TAP block has documented that TAP block reduced requirement of post-operative opioid use, increased time to first rescue analgesia, provided more effective pain relief and reduced opioid associated side-effects19. In the literature, studies have also proved the efficacy of ultrasound guided TAP block with prolonged analgesia upto 24 hours as compared to conventional methods in surgeries like laparoscopic cholecystectomy8,11,13, Caesarean delivery10 and open appendicectomy10. The above studies were performed under general anesthesia8,14,17,19 as well as spinal anesthesia10. In the current study, 20 ml of 0.25% Bupivacaine was used and TAP block provided analgesia upto 14 hours post operatively. J. Toivonen et al conducted a randomized blinded study in 100 patients undergoing herniorrhaphy under spinal anesthesia to study the effect of pre-incisional IHN block on post-operative analgesic requirement. They concluded that IHN block provided reduced analgesia requirement for about 6 hours post-operatively20. In our study, analgesia duration for IHN block was 6 to 10 hours amongst which 50% patients demanded rescue analgesia between 8 to 9 hours suggesting prolonged duration of analgesia compared to above study. The duration of ultrasound guided TAP block was 7 to 14 hours out of which 70% subjects demanded rescue analgesia between 9 to 11 hours. Thus ultrasound guided TAP block provided prolonged analgesia compared to conventional IHN block. In the study by Weintraud M et al, ultrasonography was used to determine accurate placement of local anesthetic drugs for landmark based IHN blocks. It was observed that successful block was achieved in only 62% of cases and based on ultrasound findings only 9 out of 62 blocks had accurate placement of the local anesthetic21. In our study, out of 30 subjects, failure of landmark based IHN block was noted in 1 subject evidenced by rescue analgesia demand by 3 hours of block administration after receding of spinal action. Various studies in children22,23,24 have confirmed the 100% accuracy of ultrasound guidance of IHN block compared to the blind standard techniques of IHN block. C. Aveline et al, in a randomized double blinded study on 273 patients undergoing open inguinal hernia repair under general anesthesia with Levobupivacaine 1.5mg/kg compared ultrasound guided TAP block and conventional IHN blocks25. The study concluded that ultrasound guided TAP block provided better immediate post-operative pain relief and reduced opioid demand with conventional loss of resistance IHN block. These findings are in line with our study. Liver puncture has been occasionally documented after a blind TAP block(26) and colon injury after a blind IHN block (27)and the use of ultrasound may also reduce these risks. Except failure of block, no other complications were noted in our study. In conclusion, post-operative duration of analgesia of ultrasound guided TAP block was prolonged as compared to conventional IHN block. Quality of analgesia evidenced by mean VAS scores was better with ultrasound guided TAP block as compared to conventional IHN block. One case of failure of IHN block was noted. No other side-effects or complications were noted in both the groups. Ultrasound-guided TAP block is more effective for post-operative analgesia compared to conventional IHN block. REFERNCES
|
|
 Home
Home
