Official Journals By StatPerson Publication
|
Table of Content Volume 6 Issue 3 - June 2018
Comparison of efficacy of different concentration of bupivacaine in ultrasound-guided transversus abdominis plane (TAP) block for postoperative pain relief in lower segment cesarean section
Original Research Article
1Associate Professor, Department of Anaesthesiology, Government Thiruvarur Medical College, Thiruvarur-610004, Tamil Nadu, INDIA. 2Assistant Professor, 3Professor, Department of Anaesthesiology, Government Kilpauk Medical College and Hospital, Kilpauk, Chennai–10, Tamil Nadu, INDIA. Email: drsathyan76@gmail.com
Abstract Women undergoing cesarean delivery present distinctive set of challenges to the anaesthesiologist in the immediate postoperative period. These women want to be alert and mobile in the postoperative period to care for their baby. The American college of obstetrics and gynecology states that the objective of postoperative analgesia in cesarean section patients is to hasten early ambulation, postoperative recovery and promote maternal infant bonding. Post-cesarean section pain and discomfort may be anticipated due to skin incision, uterine incision and uterine contraction. A significant component of pain experienced by patients after cesarean section is from the abdominal wall incision. Hence blocking the sensory nerve supply of the anterior abdominal wall will provide effective postoperative analgesia.TAP block is one of the regional anaesthetic techniques that blocks the sensory nerves of the anterior abdominal wall.. Especially use of ultrasound for TAP block, is the most practical imaging tool as it is portable, relatively easy to learn, and does not pose any radiation risk. Though there are many clinical trials using various local anaesthetics in different concentrations in TAP block, there is no standard guidelines regarding the choice of local anaesthetics,its dose and concentration to be used. Hence the goal of our study is to compare the effectiveness of 0.25% Bupivacaine and 0.375% Bupivacaine in ultrasound-guided TAP (Transversus Abdominis Plane) and the intensity of blockade provided by them as a part of postoperative analgesic regimen in patients undergoing lower segment cesarean section via pfannensteil incision. Key Words: Tapblock, Bupivacaine, USG, Postop Analgesia
INTRODUCTION Various modalities of treatment are available for controlling postoperative pain effectively like usage of opioids/NSAIDS, regional techniques and field blocks. As a part of postoperative analgesic regimen, initially opioids are required for effectual analgesia. But opioids can cause side-effects like emesis, nausea, itching, sedation, and respiratory depression. Hence alternative regimen that reduces opioid requirements will be beneficial in this population. McDonnell and his colleagues demonstrated the effectiveness of transversus abdominis plane (TAP) block for postoperative analgesia in cesarean section patients. He performed bilateral TAP block using 1.5 mg/kg ropivacaine and demonstrated reduced postoperative visual analog scale pain scores. It has been very well proved by various studies that TAP block is a promising technique in providing good postoperative analgesia. Ultrasound guidance for TAP block enables direct visualization of the needle and the anatomical structures. Therefore, real time images can be seen during the procedure and drugs can be given more accurately into the target site than performing a blind technique to block the peripheral nerves. This technique enhances the safety and also the efficacy of the procedure. Though there are many clinical trials using various local anaesthetics in different concentrations in TAP block, there is no standard guidelines regarding the choice of local anaesthetics, its dose and concentration to be used. Since there have been no published dose-response studies investigating the effective analgesic dose of bupivacaine for use in a TAP block for postoperative analgesia, we proposed a study primarily examining the effect on requirement of first dose of rescue analgesia when 0.25% bupivacaine, and 0.375% bupivacaine are used for TAP blocks.
MATERIALS AND METHODS This was conducted in Government Kilpauk Medical College after obtaining ethical committee approval of our institute.40 Parturients belonging to ASA physical status I and II undergoing elective Lower segment cesarean section were enrolled in our study. All the patients were explained about the purpose and details of the study. Informed written consent was obtained from each patient. Study Design: Our study was a prospective double blinded randomized control study. Patient Selection Criteria: All the 40 patients were examined and evaluated biochemically and made familiar with study plan. Inclusion Criteria
Exclusion Criteria
OBSERVATION AND RESULTS In out randomized prospective double blinded study a total of 40 patients were studied with 20 patients in each group. The statistical analyses for demographic profile were done with unpaired T test.
Table 1: Patients characteristics
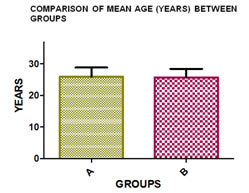
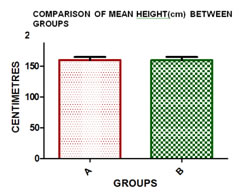
The demographic profiles like age, weight, height, BMI were compared in both groups. As per Table 1 there were no statistically significant differences in these profiles between the two groups. Figure 1: As per Figure 1, Mean age (years) between the two groups (A and B) was compared. Error bar represents the standard deviation (SD). Unpaired t test was used to compare the two groups. There was no statistically significant difference between the groups (p>0.05) Figure 2: As per Figure 2, Height (cm) between the two groups (A and B) was compared. Error bar represents the standard deviation (SD). Unpaired t test was used to compare the two groups. There was no statistically significant difference between the groups (p>0.05)
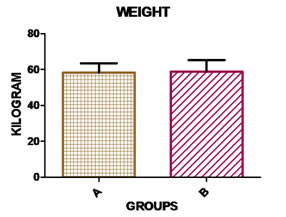
Figure 3: As per Figure 3, Mean weight (kg) between the two groups (A and B) was compared. Error bar represents the standard deviation (SD). Unpaired t test was used to compare the two groups. There was no statistically significant difference between the groups (p>0.05)
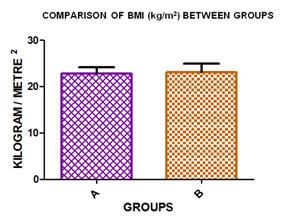
Figure 4:
As per Figure:4, Mean body mass index (kg/m2) between the two groups (A and B) was compared. Error bar represents the standard deviation (SD). Unpaired t test was used to compare the two groups. There was no statistically significant difference between the groups (p>0.05)
Table 2:
As per Table 2, there was no significant difference between two groups depending on duration of surgery.
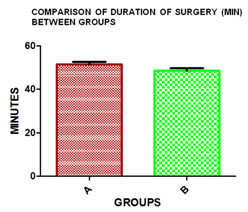
Figure 5:
As per Figure 5, Mean duration of surgery (min) between the two groups (A and B) was compared. Error bar represents the standard error of mean (SEM). Unpaired t test was used to compare the two groups. There was no statistically significant difference between the groups (p>0.05)
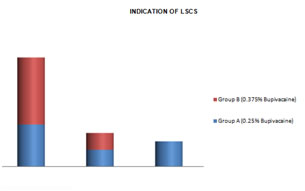
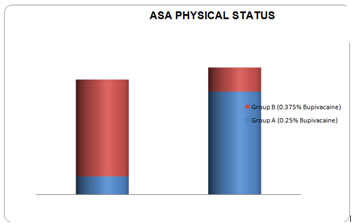
Figure 6:
Figure 7:
As per Figure 6 and 7 ASA physical status, history of previous abdominal surgery does not give any significant difference in the datas between two groups. Similarly Incision methods, surgeon and operation time were compared in both and no significant difference was noted. Observed Parameters
Table 3:
As per Table 3,
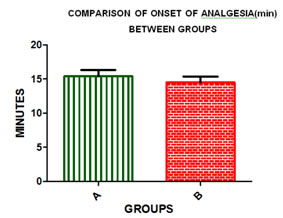
Figure 8: As per Figure 8, Comparison of mean time of onset of analgesia (min) between the two groups (A and B). Error bar represents the standard error of mean (SEM). Unpaired t test was used to compare the two groups. There was no statistically significant difference between the groups (p>0.05)
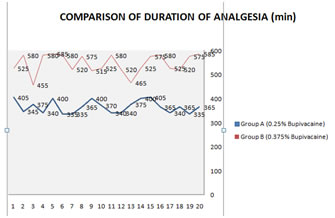
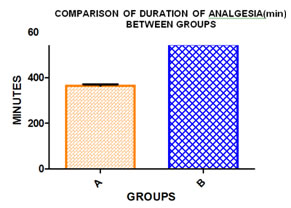
Figure 9:
Figure 10: As per Figure 9 and 10, Mean duration of analgesia (min) between the two groups (A and B) was compared. Error bar represents the standard error of mean (SEM). Unpaired t test was used to compare the two groups. The mean duration was significantly lower in the Group A compared to Group B (p< 0.0001)
Figure: 11
As per Figure 11, Group B patients had lesser VAS score for prolonged duration compared to Group A
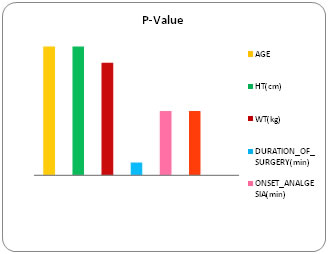
Figure 12:
As per the figure 12, statistically significant P-Value (<0.05) is obtained only for duration of analgesia which implies that 0.375% of Bupivacaine has prolonged duration of analgesia than 0.25%. DISCUSSION Based on the observation and results obtained in our study involving 20 patients in each group, results of our study was discussed in detail by comparing with the obtained data and available evidence in the literature. This study compared two different concentration of equivolume dose of bupivacaine in US-TAP block in patients undergoing cesarean section via a pfannensteil incision. The US-TAP block has the advantage of being performed accurately and safely in a short time and the target site has no vital anatomical structures. The somatic pain arising in the postoperative period can be fully managed by using a US-TAP block alone, but not by the epidural analgesic method as the somatic pain comes from the narrow dermatomes in the surgery with pfannensteil incision. The patients selected in our study were patients undergoing cesarean section, as these patients wants to be more alert and mobile in the immediate postoperative period for breast feeding and to care for their baby. Immediate pain relief in the post operative period has several implications in recovery of these patients. Kang et al. carried out a survey about postoperative pain and they reported that nearly 70% of patients expected more pain in the immediate postoperative period and most patients who answered the questionnaires had pain mainly in the early period only. So, they suggested that pain control should be in the acute period, that is on the initial postoperative stage. In our study the demographic profiles [as per table 1 and figure 1-4] like age, height, weight and BMI are comparable and there was no statistically significant difference between Group A and Group B. There were no significant differences between the two groups regarding the ASA Physical status, surgery duration, surgeon, History of any previous abdominal surgery. The effect of the US-TAP block is more when the block is carried out in patients who are responsive and alert rather than in a sedated patient. In alert patient we are able to elicit the VAS pain score, the time of onset of analgesia and the intensity of pain relief can be very well studied. In our study we used 0.25% and 0.375% bupivacaine for US TAP block. We did not find any local anaesthetic toxicity in our study group. The optimal effective volumes and concentrations of injected local anesthetics are not established in any studies and not much is known about onset time of analgesia and its duration. Therefore, it is necessary to study these parameters during a TAP block. In a recent study[29], done by Kato et al.40ml was given in TAP block and serum concentrations of lidocaine was investigated. They found out that the serum concentrations were within the therapeutic range for the anti-arrhythmic effect of lidocaine. Hence it is suggested that the analgesic effect may be caused by a systemic rather than a local effect of the local anaesthetic, and needs further studies After initiation of the block, the time of Onset of analgesia was compared between the groups and it was noted that varying the concentration of local anaesthetic does not produce any significant difference in Onset of analgesia. The VAS pain scores assessed in the US-TAP Block with 0.375% bupivacaine were significantly lower than the 0.25% group in the PACU in the immediate postoperative period. This demonstrates that the US-TAP block with higher concentration provides effective and prolonged analgesia in the initial postoperative stage. This study very well correlates with the study of Siddiqui et al[28 who in his analysis of Seven randomized, double-blinded studies of both blind and ultrasound guided TAP technique for postoperative analgesia in infra umbilical surgeries demonstrated average and significant reduction in IV PCA requirement as a part of multimodal analgesic regimen. He also demonstrated reduced VAS score both at rest and movement in the early postoperative period. He also found out the reduced incidence of postoperative nausea, vomiting and sedation. The time interval for requirement of first dose of rescue analgesia was prolonged in 0.375% bupivacaine group[mean analgesic duration-544 min] than the 0.25%bupivacaine group[mean analgesic duration-365 min]. This finding suggest that the total rescue analgesic usage is decreased in the first 24–48 h among women who received a TAP block with higher concentration than the other, immediately after cesarean delivery. This correlates with studies of PATEL et al., who. found that there was a 34% reduction in oral narcotic dosing in patients who received a TAP block. They also observed decreased opioid usage and hence the decreased side effects of it like pruritis, vomiting and nausea.This blockalso facilitates early ambulation, no urinary retention, and a more active state of the patient. In our study, there were no complications during the procedure or after the block. The adverse effects pertaining to the TAP block have been reported in the literature. There was a case report of liver trauma and peritonitis with US-TAP block in a patient who underwent hernioplasty. This incidence was due to failure to accurately image the entire needle while imaging, resulting in excessive penetration of the needle. Therefore, when the exact direction and depth of the needle is under real time images of the ultrasound, this complication can be avoided. So far US-TAP block has been used for very few surgical procedures only.But the US-TAP block could be applied more widely, warranting further researches in this field. If this block is developed more, it can be used for treating the patient’s pain more effectively. Results: A prospective randomized double blinded study was designed to compare the efficacy 0.375% and 0.25% bupivacaine in ultrasound guided transversus abdominis plane block in patients undergoing elective lower segment ceaserean section under general anesthesia. Based on the analysis of the results and discussion in our study, the conclusions arrived at are summarized as below.
CONCLUSION Hence we conclude that usage of 0.375% of bupivacaine provide more prolonged duration of action compared to equivolume dose of 0.25% bupivacaine and can be safely used in TAP block without producing any adverse effects. REFERENCES
|
|
 Home
Home