Official Journals By StatPerson Publication
|
Table of Content Volume 6 Issue 3 - June 2018
Comparison of anaesthetic efficacy of nalbuphine and dexmedetomidine as an adjuvant to ropivacaine and lignocaine in supraclavicular block for upper limb surgeries
Original Research Article
Sowmya Shanmugam1, Uma R2*, T Gayathri3, S Nageshwari4
1,3,4Post Graduate, 2Associate Professor, Department of Anaesthesiology, ESIC MC and PGIMSR, K. K. Nagar, Chennai, Tamil Nadu, INDIA. Email: rsuma@yahoo.com
Abstract Background: Brachial plexus block provides an useful alternative to general anaesthesia for upper limb surgeries. The block characteristics of dexmedetomidine and nalbuphine as adjuvants to ropivacaine, a newly emerging local anaesthetic which is less cardio and neurotoxic along with lignocaine in supraclavicular brachial plexus block is being compared. Materials and Methods: A randomized prospective controlled double blind study was undertaken in patients who were posted for upper limb surgeries under brachial plexus block. 60 patients of ASA class I and II were randomly grouped into two groups. Group N received 20 ml of ropivacaine 0.5%, 10 ml lignocaine 2% mixed with 10mg of nalbuphine and Group D received 20 ml of ropivacaine 0.5%, 10 ml of lignocaine 2% with 50 microgram of dexmedetomidine. The onset and duration of motor and sensory block, incidence of side effects where compared between the two groups. Results: Group D had quicker onset of both sensory and motor block and prolonged duration of postoperative analgesia, thus reducing the requirements of rescue analgesics when compared to group N. Key Words: Dexmedetomidine, nalbuphine, ropivacaine, supraclavicular brachial plexus block.
INTRODUCTION Brachial plexus block1 is the most widely used approach for upper limb surgeries as an alternative to general anesthesia and also in combination with general anaesthesia to achieve ideal operating conditions by providing adequate muscular relaxation, maintaining intraoperative hemodynamic stability and sympathetic blockade . It also reduces postoperative pain and requirement of rescue analgesia.2 The upper limb blocks mainly avoids the untoward effects of general anesthesia like upper airway instrumentation, difficult airway and the pressor response to laryngoscopy3,4,5. It is beneficial due to its effectiveness in terms of cost, margin of safety, along with good postoperative analgesia. A variety of approaches of brachial plexus block have been described- interscalene, supraclavicular, infraclavicular, axillary approaches. However, supraclavicular block is the easiest and most reliable method. Ropivacaine6,7 is now one of the most widely used amide local anesthetic as it has a longer duration of action varying from 5 to 8 hours and has less cardiotoxic effects. However, it has limiting factors like delayed onset and poor motor blockade. To minimize these drawbacks many drugs like morphine, neostigmine, fentanyl, hyaluronidase, midazolam, dexmedetomidine, clonidine, dexamethasone etc., have been added to local anesthetics to improve the quality of blockade and duration of action and postoperative analgesia. Dexmedetomidine8 is one of the alpha 2 agonists which is widely used as an adjuvant to regional techniques. It prolongs the duration of action of plexus blocks to more than 10 hours without causing respiratory depression.Nalbuphine9 is recently introduced opioid with agonist and antagonist property. Unlike other opioids it has got ceiling effect for respiratory depression. It also prolongs the duration of regional blocks by up to 10 hours and it is highly economical. In this study we aim to compare efficacy of nalbuphine and dexmedetomidine with lidnocaine and ropivacaine for upper limb surgeries using supraclavicular block in terms of onset of sensory and motor block and also duration of sensory and motor blockade, time to rescue analgesic and sedation scores.
MATERIAL AND METHODS After institutional ethical committee approval 60 patients between 20-70 years of age, of either sex, of ASA physical status I and 2 undergoing upper limb surgeries were included in this study after obtaining informed written consent. Patients with bleeding disorders, on anticoagulants, with neurological and musculoskeletal disease, infection at the site of injection or history of allergy to local anaesthetics were excluded from the study Sample size was calculated using n Master 2.0 software with alpha error of 5% and power of 80% and was found to be 28 per group, which was rounded off to 30 per group. Patients underwent routine pre anaesthetic check up and only those of ASA status I and II were included in the study. They were randomly allocated into two groups: GROUP N: 10 mg nalbuphine (1 ml) with 20 ml 0.5% ropivacaine (100mg), 10 ml of lignocaine (200 mg) -31 ml GROUP D: 50 microgram of dexmedetomidine (.5ml and diluted to 1 ml with distilled water) with 20ml of 0.5% ropivacaine (100mg), 10 ml of lignocaine (200 mg)-31 ml. In the operation theatre the patients were connected to standard monitors such as Pulse oximetry for saturation (SpO2), Noninvasive blood pressure monitoring(NIBP), Electrocardiogram(ECG) and baseline pulse rate, blood pressure, oxygen saturation were recorded. An intravenous line was started before procedure with 18G cannula and crystalloid infusion started. Oxygen at the rate of 4 l/min administered through face mask. Vital parameters were observed throughout the procedure at time intervals specified. Before the commencement of the procedure, patients were instructed on the method of sensory and motor assessments. The local anaesthetic mixture was prepared by the principal investigator and the block was conducted by another person who did not know which group the patient belonged to. Supraclavicular block was performed under ultrasound guidance (Sonosite TitanTM ultrasound machine with a 6-13MHz linear probe). After the plexus was indentified with the ultrasound probe the needle was introduced under ultrasound guidance and position confirmed with 0.5ml of the block solution and then the block was instituted. Adequacy of block was checked by pin prick method at the level of the elbow. The surgery was allowed to proceed when complete anaesthesia was achieved. The onset of sensory block was the time taken from the completion of injection to the loss of pin prick sensation in all dermatomes at the level of the elbow. Duration of analgesia was taken as the time from the onset of sensory block to the time when the patient requires first dose of analgesia for post operative pain. By using modified LOVETT rating scale motor block is scored from 6(usual muscular force) to 0 (complete paralysis) based on these movements which as follows -thumb abduction for radial nerve, thumb adduction for ulnar nerve, thumb opposition for the median nerve and elbow flexion and extension .Duration of motor blockade was taken as the time from onset of motor block till when the patient is able to move thumb in all directions. Adduction of thumb for median nerve, opposition for ulnar and extension of thumb for radial nerve were tested. Heart rate and blood pressures were recorded before the procedure and immediately after the supraclavicular block, then at 2 minutes interval for 10 minutes, later at 5 minutes interval until 30 minutes and then after every 10 minutes till completion of the surgery, the last reading is taken 10 minutes after the procedure. Post operative blood pressure and heart rate will be measured every two hrs until 24hrs. Pasero post operative sedation scale (POSS) was used to assess the sedation level intraoperatively and postoperatively (1=awake and alert .2=slightly drowsy, easily aroused, 3= frequently drowsy, arousable, drifts off to sleep during conversation 4=somnolent no response to verbal or physical stimulation). Complications such as arrhythmias, bradycardia, nausea, vomiting, shivering, pruritus and respiratory depression was looked for and treated accordingly. Descriptive statistics such as mean, standard deviation are used to describe the various variables. Chi square test was used for finding the difference between two groups for discrete variables and unpaired t test was used for the continuous variables. Statistical significance was considered at a “p” value<0.05. The analysis was performed using SPSS statistical software (version 21.0). The graphs were provided by Microsoft office excel.
RESULTS Table 1: Both the groups are comparable in terms of demographic data such as age, sex ratio and weight.
Table 2: Block characteristics comparison between two groups
There was statistically significant difference in the onset of motor and sensory blocks between the two groups, the onset being faster in dexmedetomidine group (5±0.89 minutes for sensory and 10.03±1.03 for motor)than the nalbuphine group (10.72±1.01 minutes for sensory and 15.26±1.47minutes for motor), and also in the duration of sensory block and the duration of analgesia (or the time to request of rescue analgesic) which were significantly prolonged in the dexmedetomidine group (13.36±1.24 hours and 13.36±1.24 hours respectively) when compared to the nalbuphine group(9.33±0.88 hours and 10.13±0.81 hours respectively). Though the duration of motor blockade was also more in the dexmedetomidine (7.65±0.54hrs) when compared to nalbuphine group (7.43±0.71hrs), the difference was not statistically significant.
Table 3: Heart rate (beats/min)
Table 4: MAP (mm Hg)
The difference in heart rate and MAP between two groups were statistically significant between two groups after 2 hours, it being significantly lesser in the dexmedetomidine group. Table 5: Sedation score
Mean sedation was 2.30 in dexmedetomidine group and 2.00 in nalbuphine group and the difference was statistically significant between two groups (p value 0.001)
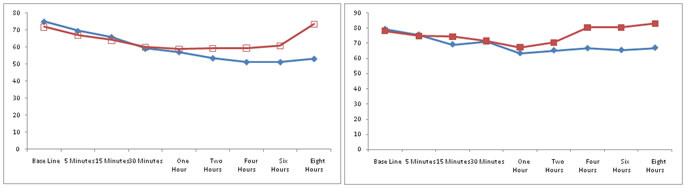
Figure 1: Comparison of mean heart rate Figure 2: Comparison of mean MAP between two groups
In figure 1, red line represents the heart rate in bpm in group N The blue line represents the heart rate in bpm in group D The mean heart rate in nalbuphine-ropivacaine group was 63.87 minutes and mean heart rate in dexmedetomidine-ropivacaine group was 59.55mins. There was statistically significant difference in the mean heart rate (beyond 1 hour) between the two groups. In figure 2, red line represents the MAP in mmHg in group N The blue line represents the MAP in mmHg in group D
DISCUSSION Brachial plexus block has emerged as one of the popular anaesthetic technique for upper limb surgeries1. This regional technique avoids untoward effects of general anaesthesia related to airway instrumentation and poly pharmacy3,4,5. Brachial plexus block is usually performed using a mixture of local anaesthetics. Ropivacaine, a newer amide linked local anaesthetic with added advantage of lesser cardio toxicity is used in this study6,7. But however it has added disadvantage of patchy and incomplete analgesia. In order to overcome this disadvantage various adjuvant drugs have been used to make it more effective for surgery and postoperative analgesia. Dexmedetomidine8 is an alpha 2 agonist (α2:α1 – 1620:1) which when added as an adjuvant prolongs the duration of analgesia and shortens the onset of motor and sensory blockade. It is best used as a sedative without risk of respiratory depression. It acts by decreasing the activity of nor adrenergic neurons in the locus ceruleus in the pons, thereby inhibitory GABA neurons activity is increased in ventrolateral pre optic nucleus. Thus the propagation of pain pathway is terminated. α2b receptors stimulation is responsible for transient increase in blood pressure initially. α2a receptors stimulation is responsible for sedation, analgesia and causes vasoconstriction thereby prolonging the effect of local anaesthetics. Nalbuphine9 is a mixed kappa agonist and mu antagonist opioid. Its analgesic and sedative action is due to its affinity to kappa receptors. It has cardiovascular stability, unike other opiods it has ceiling effect on respiratory depression. The mean time of onset of sensory block in nalbuphine group was 10.72 ±1.01minutes which was longer when compared with dexmedetomidine group which was 5 minutes. In a study conducted by Suneet Katuria et al10 in Punjab, which compared ropivacaine with ropivacaine- dexmedetomidine, the mean onset of sensory blockade was 9.75±4.23 minutes in dexmedetomide. In a study conducted by Kumkum et al11 there was no effect on onset of sensory blockade. The onset of sensory blockade was comparable with a study conducted by NaziaNazir et al12 which was 4.89±1.5minutes. The difference in mean sensory block onset time in our study could be due to addition of lignocaine. The mean onset of motor blockade in our study in nalbuphine group 15.26±1.47minutes which was longer than dexmedetomidine group which was 10.03±1.03minutes. The mean onset of motor blockade in a study conducted by Suneeth Kathuria10 was 18.75± 6.37 minutes. Onset of motor blockade of nalbuphine was comparable with a study conducted by Nazia Nazir12. The difference in onset of motor blockade could be due to addition of lidnocaine in our study. In the study duration of sensory blockade was 13.36± 1.24hours in group D and 9.33 ± 0.88 hours in group N. In a study conducted by Suneet Kathuria10 duaration of sensory blockade was 967.55±310.50 mins. In study conducted by Kumkum et al11 duration of analgesia in nalbuphine group was 481.53±42.45mins. In a study conducted by NaziaNazir et al12 duration of analgesia in nalbuphine group was 389.33±14.53 mins which was comparable with our study. The mean heart rate and MAP in nalbuphine group was slightly higher (63.866±6.4bpm) than dexmedetomedine group (54.23±4.53bpm). There was no significant difference in heart rate and MAP between the two groups intra operatively whereas post operatively (after 60 mins) heart rate and MAP were significantly lower in dexmedetomedine group as compared to nalbuphine group. This could be due to the inherent property of dexmedetomidine to cause bradycardia or due to prolonged duration of analgesia in dexmedetomidine group. Sedation was assessed using POSS rating and it was found to be statistically significant with mean score of 2.30 ± 0.47 in dexmedetomidine group and mean of 2±0.01 in nalbuphine. The time of rescue analgesia was significantly more in dexmedetomidine group 14.53±1.07 hours compared to nalbuphine group in which it was 10.13±0.81 hours. No adverse effects like respiratory depression, hypotension, bradycardia,nausea and vomiting were reported in both the groups in the study. In a study conducted by Suneet Kathuria10 only 2 cases had hypotension one patient had allergy and no respiratory depression in dexmedetomidine group. In this study it was found that both nalbuphine and dexmedetomidine were good adjuvants with no significant side effects and stable hemodynamics. Of the two groups dexmedetomidine prolonged the duration of analgesia more and also hastened the onset of block. Nalbuphine though not on par with dexmedetomidine has an added advantage of lower cost.
CONCLUSION In this study it was found that both dexmedetomidine and nalbuphine where good adjuvants to ropivacaine for supraclavicular block. The drugs did not show any significant side effects and provided stable intra and postoperative hemodynamics. Of the two groups dexmedetomidine prolonged duration of analgesia and hastened onset of motor and sensory block more than nalbuphine. Nalbuphine though not on par with dexmedetomidine has an added advantage of lower cost. Sedation was higher in the dexmedetomidine group when compared to the nalbuphine group. REFERENCES
|
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
 Home
Home