Official Journals By StatPerson Publication
|
Table of Content - Volume 7 Issue 1 -July 2018
Dexmedetomidine as an adjuvant to ropivacaine in supra-clavicular brachial plexus block
P V Bhale1*, Tejas Warkari2, Pannag Bhushan Dasmohapatra3
1Professor, 2,3Jr. Resident, Department of Anaesthesia, MGM Medical College, Aurangabad, Maharashtra, INDIA. Email: pramod.bhale@gmail.com
Abstract Background and Aim: The advantages of a supraclavicular technique over other brachial plexus block approaches are its rapid onset and complete and predictable anesthesia for entire upper extremity and particularly, hand surgery. In this study, we observed the efficacy and safety of dexmedetomidine as an adjuvant to ropivacaine in supraclavicular brachial plexus block. Method: Thirty five American society of anaesthesiologist class I and II adult patients who were scheduled to undergo upper limb hand surgery were randomly allocated to following groups to receive unilateral supraclavicular block: Ropivacaine 0.5% (30 ml) + dexmedetomidine 1 µg/kg All the patients were assessed for Onset of sensory block, Onset of motor block, Duration of sensory block, Duration of motor block, Duration of analgesia, Haemodynamic stability, Ramsay sedation score. Any complications such as pneumothorax, hematoma, arrythmias, tinnitus, dizziness, circumoral numbness and seizures was noted and documented. Result: The mean duration of sensory block was 780.3±39.0 min with Ropivacaine and Dexmedetomidine. The mean duration of motor block was 711.1±39.5 min with Ropivacaine and Dexmedetomidine. The mean duration of analgesia with Ropivacaine and Dexmedetomidine was 864.0±44.7 min. Ropivacaine and Dexmedetomidine were similar with regard to pulse rate, mean arterial blood pressure and oxygen saturation. There was no statistically significant difference (P > 0.05). Conclusion: We conclude that dexmedetomidine, 1 µg/kg when added as an adjuvant to ropivacaine in supraclavicular brachial plexus block has significantly prolonged the duration of analgesia along with significant increase in the duration of sensory and motor blockade. Dexmedetomidine also provided better arousable sedative effects without any side effects. So dexmedetomidine is a better adjuvant in supraclavicular brachial plexus block for upper limb surgeries. Key Word: Supraclavicular brachial plexus block, dexmedetomidine, ropivacaine, post operative analgesia.
Modern era can be called as the era of regional anesthesia. Peripheral nerve blocks not only provide intraoperative anesthesia but also extend analgesia in the post-operative period without any systemic side effects. Brachial plexus block is one of the peripheral nerve blockade which has been used for surgeries of upper limb.¹ Brachial plexus block can be given either by interscalene, supraclavicular, infraclavicular or axillary approach. The advantages of a supraclavicular technique over other brachial plexus block approaches are its rapid onset and complete and predictable anesthesia for entire upper extremity and particularly, hand surgery.² Many local anaesthetics has been used to produce brachial plexus block. Most common among them being bupivacaine, because of its higher potency and prolonged duration of action. One of the disadvantage is that its cardiotoxicity, especially with inadvertent injection into subclavian artery. So ropivacaine was developed with properties similar to bupivacaine, having lower lipid solubility and less cardiotoxicity.³ However the duration of the action of local anaesthetics (LA) are short, resulting in conversion to general endotracheal anesthesia which may be sometimes difficult to provide in the middle of the surgery especially in lateral positions. Various methods have been used to extend the duration of analgesia like using higher volume of local anaesthetics but it may also increase the risk of LA systemic toxicity. Continuous catheter-based nerve blocks provide very good postoperative analgesia but their placement requires additional time, cost and skill. So practice of using adjuvants to local anaesthetics is becoming popular.4-9 Alpha-2 adrenergic agonists become popular because for their has sedative, analgesic, antihypertensive, antiemetic actions in addition to reducing the anesthetic drugs requirement. Alpha-2 adrenergic agonists have been tried either alone or in combination with other drugs, in epidural, intrathecal and peripheral injections, to prolong the duration of anesthesia. Clonidine a partial alpha 2 agonist has been shown to prolong the duration of anesthesia and analgesia in nerve blocks. Dexmedetomidine, a selective alpha2 agonist, with affinity eight times that of clonidine, also has been shown to prolong the sensory and motor duration when added as an adjuvant to local anaesthetic in nerve blocks.10-11 In this study, we observed the efficacy and safety of dexmedetomidine as an adjuvant to ropivacaine in supraclavicular brachial plexus block.
MATERIALS AND METHODS Inclusion Criteria
Exclusion Criteria
All the patients were informed about the procedure of anesthesia and consequences. All patients will be kept nil orally for 6 hrs. Equipments
Method: In our study sample size of 35 in group was calculated, taking power of study as 90% (alpha error of 5% and beta error of 95%). Considering the drop rate of 5%, we fixed the sample size (n) as 35 in a group. To make the study double blind one anaesthesiologist (caregiver) will prepare the drug and perform the supraclavicular brachial plexus block while second anaesthesiologist (investigator) will observe the parameters. The patient was also unaware about drug regimen. Statistical Analysis: All data was presented as Mean ± SD (Standard Deviation). Demographic data was analyzed using Chi-square test and statistical significance in mean difference was done using student’s t test. All statistical analysis was made using SPSS 22 for Windows (Statistical Package for Social Science). P<0.05 was regarded as statistically significant and P>0.05 was regarded as non significant.
OBSERVATIONS AND RESULTS The study population consists of 35 patients scheduled for surgery of elbow, forearm and hand. Ropivacaine and Dexmedetomidine received Ropivacaine 0.5% (30 ml) + dexmedetomidine 1 µg/kg via supraclavicular brachial plexus block.
Table 1: Onset of sensory block
The mean duration of onset of sensory blockade of Ropivacaine and Dexmedetomidine was 10.14±1.83 min.
Table 2: Duration of sensory block
The mean duration of sensory block was 780.3±39.0 min in Ropivacaine and Dexmedetomidine.
Table 3: Onset of motor block
The mean time of duration of onset of motor block in Ropivacaine and Dexmedetomidine was 17.37±1.94 min.
Table 4: Duration of Motor block
The mean duration of motor block was 711.1±39.5 min in Ropivacaine and Dexmedetomidine.
Table 5: Duration of analgesia
The mean duration of analgesia in Ropivacaine and Dexmedetomidine was 864.0±44.7 min.
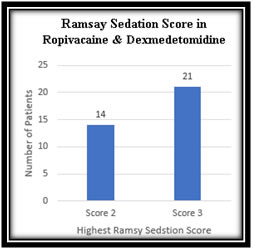
Table 6: Highest Ramsay Sedation Score
Figure 1: Highest Ramsay Sedation Score Achieved in Ropivacaine and Dexmedetomidine. The highest Ramsay Sedation Score achieved for Ropivacaine and Dexmedetomidine was 2/6 (in 14 patients) or 3/6 (in 21 patients). Although higher number of patients achieved greater sedation score in Ropivacaine and Dexmedetomidine but it was not statistically significant (p>0.05). Table 7: MeanPulse Rate
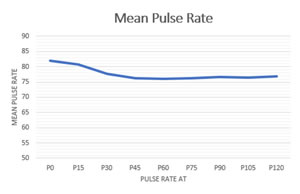
Figure 2: Pulse Rate in minute at different time in Ropivacaine and Dexmedetomidine
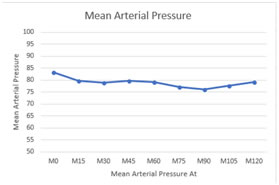
Figure 3: Mean Arterial Pressure in minute at different time in Ropivacaine and Dexmedetomidine
DISCUSSION Brachial plexus block is one of the most commonly performed peripheral nerve blocks in day today practice. It can be used as the sole anaesthetic technique or in combination with general anesthesia for intraoperative and postoperative analgesia. Ropivacaine is less lipophilic than bupivacaine and that, together with its stereo selective properties, contributes to ropivacaine having a significantly higher threshold for cardiovascular and central nervous system toxicity than bupivacaine in healthy volunteers. There has always been a search for adjuvants to the regional nerve block with drugs that prolong the duration of analgesia but with lesser adverse effects. Alpha-2 adrenergic receptor agonists have been the focus of interest for their sedative, analgesic, perioperative sympatholytic and cardiovascular stabilizing effects with reduced anaesthetic requirements. Hence dexmedetomidine has been selected as adjuvants in our study. The present study population consists of 35 patients scheduled for surgery of elbow, forearm and hand. Ropivacaine and Dexmedetomidine received Ropivacaine 0.5% (30ml) with dexmedetomidine 1 mcg/kg via supraclavicular brachial plexus block Demographic data and mean duration of surgery were similar in the groups. (p>0.05) Characteristics of sensory block, motor block, duration of analgesia, sedation score, haemodynamic effects and complications were studied in group.
SUMMARY In our study, patients received dexmedetomidine 1 mcg/kg as an adjuvant to 30 ml of 0.5% ropivacaine in supraclavicular brachial plexus block. The onset of sensory block was 10.14±1.83 min. The duration of sensory block was 780.3±39.0 min which showed statistically longer duration of sensory block. The onset of motor block was 17.37±1.94min. The duration of motor block was 711.1±39.5min which showed statistically longer duration of motor block. The duration of analgesia was 864.0±44.7 min thus patient had a statistically longer duration of analgesia. Sedation score was better with dexmedetomidine (RSS 3 in 60% patients). Haemodynamic stability was well maintained in all patient.
CONCLUSION We conclude that dexmedetomidine, when added as an adjuvant to ropivacaine in supraclavicular brachial plexus block has significantly prolonged the duration of analgesia along with significant increase in the duration of sensory and motor blockade. Dexmedetomidine also provided better arousable sedative effects without any side effects. So dexmedetomidine is a better adjuvant in supraclavicular brachial plexus block for upper limb surgeries.
REFERENCES
|
|
 Home
Home