Official Journals By StatPerson Publication
|
Table of Content Volume 8 Issue 1 - October 2018
A comparative study between the efficacy of fentanyl with bupivacaine 0.5%, buprenorphine with bupivacaine 0.5% and midazolam with bupivacaine 0.5% in spinal anesthesia for lower abdominal surgeries
M Dhakshinamoorthy1, V Anandaraj2*
1Professor, 2PG Student, Department of Anaesthesiology, Rajah Muthiah Medical College, Annamalai University, Chidambaram, Tamil Nadu, INDIA. Email: dranandmbbs@yahoo.com
Abstract Background and Objectives: The major feared consequences of surgery experienced by the patient is pain, both physically and psychically, thus Providing the effective analgesia in post surgical period to the patients becomes challenging in the speciality of anesthesia. Multidimensional analgesic approaches like parenteral analgesics or regional analgesia with spinal adjuvants like opioids, benzodiazepines and a2 agonists are commonly practiced. The main intention of this study is to compare the analgesic efficacy of Fentanyl (A), Buprenorphine (B), midazolam (C) with bupivacaine intrathecally in lower abdominal surgeries. Materials and Methods: A Seventy five American society of anaesthesiologist physical status I and II patients scheduled for various surgeries in lower abdomen were identified and randomised into three groups of twenty five patients each and studied. Group A, B and C received fentanyl, buprenorphine and midazolam with hyperbaric bupivacaine respectively. Patients involved in studies were studied for intraoperative hemodynamic changes, onset of sensory, motor blockade, total period of analgesia, and peri operative complications for twenty four hrs post surgery. Visual Analog Score (VAS) was recorded at the end of surgery and hourly up to 8 hours and the time for rescue dose of analgesia was noted. ANOVA, SPSS version 16 was used for analysis. Results: We have found that all the three drugs provided pain relief for various lower abdominal surgeries with hemodynamic stability. Duration of analgesia was significantly higher in buprenorphine than fentanyl and midazolam groups (446±16.99 mins Vs 225±19.37 mins and263 ± 14.63 mins with ‘P’ value < 0.01). Conclusion: supplementing bupivacaine with buprenorphine 60 micrograms intrathecally provides effective significant pain relief for longer period of time than fentanyl and midazolam in peri operative period. Key Words: Analgesia, bupivacaine, buprenorphine, fentanyl, midazolam, post operative, spinal anesthesia.
”Divine is the task to relieve pain.” Hippocratus The major dreadful consequences of surgery is pain, both physically and psychically1, thus relieving pain during peri operative period remains a challenge. Providing the effective analgesia in post surgical period to the patients becomes challenging in the speciality of anesthesia7. A proper analgesia in post surgical period carries a decrease in amount of respiratory and cardiac complications, early recovery and ambulation2 leading to return of bowel motility and so forth decreased hospital stay., thus improving the quality of life of the patient, There were various modalities tried for the managing the pain in post surgical period including post operative oral and parentral opioids, nsaids which has its own complications like nausea vomiting3 and abuse4. In recent times, Fentanyl, a synthetic lipophilic opioid8 and pure mu receptor agonist, has been commonly used adjuvant6 supplementing bupivacaine in spinal anesthesia due to its quicker onset of sensory and motor block8,9 with minimal intra and post operative events adverse events like depression of respiratory centres10,11.with good cardiovascular stability Buprenorphine, lipophilic opiod, is a mixed agonist antagonist with high affinity at both m(mu) and kappa opiate receptors. These versatile nature of buprenorphine created the base for comparing with other opioids for using as an additive in spinal anesthesia. Midazolam, water soluble, imidazobenzodiazepine derivative. The discovery of analgesic property of midazolam in spinal anesthesia through its action on GABA A receptor located in substansia gelatinosa13 opens the gate for experimenting this drug for intrathecal usage6 as spinal adjuvant replacing opioids due to its minimal to nil complications like peri operative nausea and vomiting commonly seen in opioids6 Hence, The main intention of this study is to compare the perioperative analgesic effiacy of fentanyl, buprenorphine and midazolam along with bupivacaine for surgeries in lower abdomen.
MATERIALS AND METHODS It was a prospective randomised controlled, double blinded study, conducted after approval from institution ethical committee and obtaining valid written informed consent from the patients. Study was conducted at RAJAH MUTHAIH MEDICAL COLLEGE AND HOSPITAL, Chidambaram from 1st July 2017 to 1st June 2018 A Seventy five American society of anaesthesiologist physical status I and II patients scheduled for various surgeries in lower abdomen were identified and randomised into three groups of twenty five patients each and studied. Group A received 15mg of 0.5% hyperbaric bupivacaine with 25 µg of fentanyl, Group B received 15mg of 0.5% hyperbaric bupivacaine with 60 µg of buprenorphine, Group C received 15mg of 0.5% hyperbaric bupivacaine with 2 mg of midazolam intrathecally. Patient’s denial, known allergen to local anaesthetics, infection over spinal block area and patients with coagulopathy were excluded. The randomization was generated by computer and patients were randomised into three groups Double blinding is executed by designating another anesthetist who will prepare bupivacaine with spinal adjuvants as mentioned above and wont participate in the study for further follow up. The anesthetist or patients participated in the study were not informed about the drug constitutes in the preloaded sterile syringes. Patients were educated about the Visual analog score (VAS) preoperatively. After shifting the patient inside operation theatre, the patient’s baseline hemodynamics like heart rate, blood pressure, SpO2, respiratory rate were monitored and documented. Under strict aseptic protection and care, patients were made to lie over neutrally levelled table and positioned in left lateral recumbent or sitting position and lumbar subarachnoid block was performed in the L3- L4 interspace in classic midline approach by 23G or 25G quinke babcock spinal needle after infiltrating the skin with 2 ml of 2% lignocaine. By confirming the uninterrepted flow of CSF and negative aspiration of blood, the loaded drug was admistered in slow steady manner. After completion of injection, patients were made to lie over table supine quickly with head support and hemodynamic parameters were monitored accordingly. In Postoperative period Visual Analogue Scale (VAS) was used for assessing pain relief with score of "0" indicates nil pain and score of "10" indicates worst possible pain. Patients were followed up in post operative period and assessed with VAS. When a patient reaches VAS score of 4 or more, rescue analgesic was given and recorded. The study was concluded with first request of analgesia by patient. At the end of study, the data were compiled and subjected to statistical analysis using ANOVA, SPSS version 16 for analysis. A statistical value of p<0.01 was considered significant.
RESULTS AND DISCUSSION Currently., spinal anesthesia is the choice for various lower abdominal surgeries and being popular due to various reasons like profound blockade by the relatively simple injection of minimal amount of local anesthetic drug intra the cally14 Bupivacaine become routinely used local anesthetic intrathecally for various lower abdominal and lower limb surgeries. The sensory block produced by bupivacaine intra operatively is sufficient to conduct surgery and ensure the satisfaction of patient in pain relief. Adequate motor block by bupivacaine aid the surgeon’s work in terms of relaxation in field of surgery. Good sensory and motor blockade was continuing in initial post operative period but the pain relief in later part of post operative period is always an unresolved problem. The limited duration of action of bupivacaine in post operative period were addressed and introduction of opioids and benzodiazepines as spinal adjuvant to bupivacaine gained interest among anaesthesiologists. In our study we compare the efficacy of fentanyl, buprenorphine and midazolam with hyperbaric bupivacaine 0.5% in spinal anesthesia. All the three groups were comparable with respect to demographic variables (Age, Height, Weight) and ASA status did not vary significantly between three groups. (Table 1 and 2) Table 1: Patient demographics
Table 2: ASA Classification
Table 3: Onset of sensory block
In our study the time taken to achieve T10 sensory blockade is the time taken as onset of sensory blockade. Buprenorphine group (group B) shows statistically earlier onset than other groups( p < ). The mean onset of sensory blockade in group A, B, C are 3.11 mins, 2.05 mins and 2.85 mins respectively. A dose of 60 μg of Buprenorphine was used intrathecally by Dixit S et al15. with 1.7 ml of hyperbaric Bupivacaine in parturients undergoing elective caeserean section. He concluded that mean onset of analgesia was 1.85 minutes15. Thomas and co-workers16 in their study showed that the onset of sensory analgesia was about 157 seconds with a range of 30 - 306 seconds.16 our results are similar to the above studies. Our result regarding group A is supported by studies done by Singh et al17, where they concluded that fentanyl does not alter the onset of sensory block. however Avinash et al18, in their study showed that fentanyl hastens the onset of sensory blockade (mean onset time 2.15 mins)when compared to nalbuphine (2.92mins). also a study concluded by Krishnakumar et al19, concluded that there is no difference in onset of sensory blockade between buprenorphine and fentanyl when combined with Bupivacaine. Regarding group C Dubey R et al20, conducted a study concluding that midazolam hastens the onset of sensory blockade (mean 2.15mins) which is comparable to our results. However results of Agarwal et al21, and Vibhuti et al22, concluded that midazolam doesnot hastens the onset of sensory blockade (mean onset of sensory blockade 3.15 mins and 6.64 mins respectively). ONSET OF MOTOR BLOCKADE Table 4: Onset of Motor Block
In our study onset of motor blockade is significantly faster in Buprenorphine group (2.5 mins) when compared to other groups (3.5 and 3.71 minutes in the Group A and group C respectively). Its comparable with studies done by Gupta et al23, and Krishnakumar et al19, in which they used 60mcgs and 75mcgs respectively to achieve motor blockade of Bromage 3 at 1.98 mins and 2.74 mins respectively. However Krishnakumar et al19 concluded that fentanyl 25mcgs had an earlier onset of motor blockade (2.2mins) than Buprenorphine 75mcgs which is contrary to our studies (3.4mis). Group C shows onset of motor blockade at 3.17 mins which is comparable with the studies of Vibhuti et al22, and Dubey.R et al20(3.03 mins). Maximum Level of Sensory Blockade: There is no statistical difference in the maximum level of sensory blockade achieved. In majority of the cases the level reached is T6.This is support In studies done by Harsha vardhan et al24, comparing bupivacaine with bupivacaine and buprenorphine, addition of buprenorphine showed higher level of sensory blockade than control group.
Duration of Analgesia Table 5: Duration of analgesia
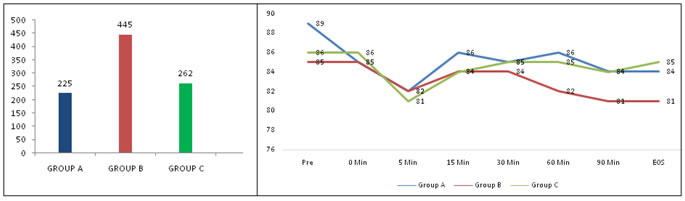
The mean duration of sensory blockade in our study is significantly longer in Group B (445 mins, p< 0.001) than in Group A(225mins) and Group C(262mins).Study conducted by Krishnakumar et al19, concluded that Buprenorphine (75mcgs) addition prolonged the sensory blockade when compared to Fentanyl(25mcgs)(267 mins vs 174 mins). However its supported by the study of Pawar et al18 which showed duration of analgesia with addition of 25mcgs was around 208mins.When compared to this study our study shows more prolonged analgesia even with 60mcgs Buprenorphine. Our study results on addition of Buprenorphine are comparable with studies by Harsha vardhan et al24, Anoop singh et al25, (362mins) and Gupta et al20, (289 mins). Capogna et al12, study on parturients concluded increasing dose of Buprenorphine increased the duration of sensory blockade (173 mins for 30mcgs vs 420 mins for 45mcgs of Buprenorphine). Group C (midazolam) results are supported by the study of Dubey R et al20 which showed a sensory blockade of 231 mins. However its contrary to the studies of Nidhi Agarwal et al21, in which 2mg midazolam intrathecally produced analgesia upto 17hrs. M.H. Kim and Y.M. Lee27 used 1 mg and 2 mg midazolam with bupivacaine on 45 patients undergoing haemorrhoidectomy. The duration of analgesia with bupivacaine was 3.99±0.78 hours, with 1 mg midazolam 6.02±1.49 hours and with 2 mg of midazolam the duration of analgesia was 8.37±2.51 hours. The results of their study are like present study.12 Batra YK et al28 found that addition of midazolam(2mg)to bupivacaine produces better postoperative analgesia (up to 6 hours) without prolonging recovery, which is similar to our study. These results are comparable to our results.
Figure 1: Duration of analgesia Figure 2: Mean arterial pressure
Duration of Motor Blockade: There is no significant difference in duration of motor blockade among the groups(p>0.05). With mean duration of motor blockade of 155mins, 180mins and 153mins in Group A, B and C respectively. Agarwal K et al31., showed by their studies that Buprenorphine with a dosage of <75mcgs intrathecally doesnot prolong the duration of motor blockade. Also Group B result are supported by Gupta et al23 and Krishnakumar et al19. Batra YK et al28 found that addition of 2 mg midazodam to spinal bupivacaine increased the duration of sensory analgesia from 229.8+41.4 min. to 267.6+67.38 min without prolonging the duration of motor blockade. The results of our study are similar to studies of P.H. Tan et al, Ping Heng Tan et al, Batra YK et al, Mahima Gupta M, Shailaja S, Hegde KS28-30 which also concluded that midazolam doesnot prolong motor blockade. The duration of motor block in group A shows that fentanyl does not prolong it as supported by the study of Singh et al and Krishnakumar et al19. VAS SCORES: Postoperative period was assessed by VAS scores which showed significantly better scores in Group B. This is supported by Harsha Vardan et al24., which showed significant better VAS scores in Buprenorphine group(p<0.001). Krishnakumar et al19, concluded that there is no difference in VAS scores after administration of intrathecal Buprenorphine and Fentanyl along with Bupivacaine. Kim MH et al found no significant difference in VAS score after administration of midazolam26 Batra YK et al28 found a significantly higher VAS score (6.6+3.05 to 55.00+0.00) in bupivacaine group from 90 to 360 min. as compared to midazolam group during this period (1.43+2.90 to 15.00+5.53). Hemodynamic Changes: The vital parameters monitored are pulse rate, blood pressure, respiratory rate and oxygen saturation. There is no significant changes in the hemodynamic parameters monitored during the study. In Group A and C hypotension was observed in 16% ofpatients (4 patients), whilein Group B 8% (2 patients) had hypotension. Bradycardia was observed in 4% of patients (1patients) in Group A and C and no bradycardia observed in Group B. By comparing all three drugs Group B (buprenorphine) found to have good hemodynamic stability throughout surgical procedure, however it is statistically insignificant. Respiratory depression is one of the main concerns with our study drugs. In our study no case had respiratory depression. Peripheral arterial oxygen saturation in all cases remained above 95% and respiratory rate of all patients was above 10 per minute. Our results are supported by studies of Krishnakumar et al19., Dubey R et al20., Soumya et al32., and Harsha Vardhan et al24.
Table 6: Mean arterial pressure
Table 7: Comparison of side effects
There is no statistically significant difference seen between the groups. Bradycardia and Hypotension are discussed above. Shivering was observed in 4% of patients (1 patients) in Group A and B and no shivering was observed in Group C. Nausea and vomiting was observed in 4% (1 patients) in Group A and C and nil in Group B.Sedation was observed in 3 patients (12%) of group C and 1 patient in group B and, nil patients in group A. Capogna et al26 observed Nausea and vomiting during post surgical period in 34 % and 40% of patients who received 30 mcg and 45 mcg of buprenorphine with hyperbaric bupivacaine 0.5% respectively. Sen et al33 studied on elderly patients who undergone various lower limb surgeries and he observed nil adverse effects except nausea and vomiting during post surgical period in 33% of patients with higher doses of 300 mcg of buprenorphine with one ml of hyperbaric bupivacaine 0.5% intrathecally Kim MH27, et al found no episodes of hypotension, bradycardia, sedation or dizziness in any patient receiving intrathecal midazolam. Obara et al20. evaluated the effects of intrathecal Fentanyl added to hyperbaric Bupivacaine for cesarean section and concluded that addition of intrathecal Fentanyl to hyperbaric Bupivacaine improved the quality without side effects. By comparing all three drugs in terms of intra operative complications.all are effective in decreasing the intraoperative complications,but Group B (buprenorphine) holds superior with minimal adverse effects intra operatively and found to have good hemodynamic stability throughout the surgical procedure. CONCLUSION This study found that supplementing bupivacaine with 60 mcg of buprenorphine fastens the onset of both sensory and motor blockade of bupivacaine with relatively stable hemodynamics and provides significant relief of pain in both intraoperative and post surgical period for longer period of time
REFERENCES
|
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
 Home
Home