Official Journals By StatPerson Publication
|
Table of Content Volume 8 Issue 1 - October 2018
A prospective randomised study to compare serum lactate level in patients receiving induced controlled hypotension with propofol and isoflurane for functional endoscopic sinus surgery
S Narmatha1, K Radhika2*, R Uma3
1Sr. Resident, 2,3Associate Professor, Department of Anaesthesiology, ESICMC and PGIMSR, K. K. Nagar, Chennai–78, Tamil Nadu, INDIA. Email: radhikamurali0095@gmail.com
Abstract Lactate which the metabolic end product of anaerobic metabolism is being used as a marker of hypoperfusion. It is seen is various conditions which decrease tissue perfusion and hence used as a marker for inadequate cellular oxygen delivery during hypotensive anaesthesia in our study which compares the effect of propofol and isoflurane hypotensive anaesthesia during functional endscopic sinus surgery (FESS). In our study 60 patients of ASA I and II undergoing FESS where divided into two groups randomly to receive either isoflurane (group 1) or propofol (group 2) intraoperatively to maintain a mean areterial pressure between 60-70mmHg. The vitals, blood loss, the quality of the surgical field and serum lactate levels where measured and recorded at appropriate intervals and satistically analysed. There was a raise in serum lactate levels with induction of hypotensive anaesthesia but the raise was within physiological limits and returned to baseline within 60mts of recovery. There was no significant difference between the two group in terms of heart rate, mean arterial pressure, blood loss, operative field or serum lactate levels. Key Words: Hypotensive anaesthesia, serum lactate, propofol, isoflurane.
Lactate is a metabolic end product of anaerobic glycolysis and is produced by the reduction of pyruvate by lactate dehydrogenase (LDH) enzyme. The normal lactate to pyruvate ratio is approximately20:1.Although lactate is produced in all tissues, skeletal muscle, brain, red blood cells and renal medulla are responsible for the majority of the production. Under conditions of hypoxia, pyruvate is unable to enter mitochondria and is converted to lactate instead. The increase in the reduced nicotinamide adenine dinucleotide (NADH)/NAD+ ratio and the concentration of pyruvate both favor the continued production of lactate. Two moles of ATP are produced for every mole of glucose metabolized to lactate. Hence, under anaerobic conditions, energy production continues, at a reduced rate, and at the expense of lactate production1. Hyper lactatemia may be due to severe sepsis, septic shock, tissue hypoxia, circulatory failure, haematological disorders or as a reaction to drug. Lactic acid levels also increase after exercise, but return to normal in healthy individuals. Hyperlactataemia results from anaerobic metabolism, in response to inadequate cellular oxygen delivery. It is often used as a marker of oxygen delivery2. Functional Endoscopic Sinus Surgery (FESS) needs a clear surgical field for good visibility of nasal structures. Controlled hypotension is provided by a combination of 15 degree head up tilt and pharmacological manipulations. Greene et al3 reported that hypotensive anaesthesia is accompanied by a considerable fall in cardiac output, and by reduced renal, hepatic and cerebral blood flows. Is the reduction in circulation great enough to produce permanent or even transient organ damage? In an attempt to answer this we have measured serum lactate level during the hypotensive anaesthesia to uncover any metabolic evidence of cellular hypoxia, since this might exist despite adequate arterial oxygenation.
MATERIAL AND METHODS After institutional ethical committee approval 60 patients of physical status I and II aged between 18-55yrs scheduled to undergo elective FESS under general anaesthesia of either sex were included in the study after obtaining written informed consent. Patients who were pregnanct, morbidly obese, heavy smoker, patients on anticoagulants and with haematological disorders were excluded. Then study population was divided into two groups (groupI isoflurane and group II propofol by lottery method. The study population was fasted as per the standard guidelines. The allocation was done by lottery method. The principal investigator enrolled the patients and following recruitment, the allocation was revealed in the operating room to the anesthesiologist anesthetizing the patients. Double blinding was not possible because of the nature of the study. The anesthesiologist was not blinded to the study drug but the anesthesiologist assessing the blood loss was blinded to the study drug. On arrival to the operating room, an intravenous (IV) line was sited and pulse oximetry (SpO 2), noninvasive blood pressure (NIBP), electrocardiogram (ECG) and end tidal carbon dioxide(ETCO2). Baseline values were recorded before induction of anesthesia and was recorded every 5 minutes throughout the surgical procedure. After preoxygenation, induction of anesthesia was done with midazolam (2 mg),glycopyrrolate(0.2 mg), fentanyl (2 μg kg–1)and propofol (2 mg kg–1) IV. After ensuring adequate ventilation, vecuronium (0.1 mg kg–1) was administered. Orotracheal intubation was performed and the lungs were ventilated. Oropharynx was packed with a saline-soaked throat pack. In group1 anaesthesia was induced and maintained with 50% oxygen in air, and isoflurane. The concentration of isoflurane was adjusted according to the patient's response and to achieve a mean arterial pressure between 60 and 70 mmHg. However, it was decided not to exceed the end tidal concentration of isoflurane above 2%. In group 2 anaesthesia was induced and maintained with 50% oxygen in air, propofol infusion started at 12 mg kg–1 h–1 for 10 min following intubation, then 10 mg kg–1 h–1 for next 10 min and continued at 8 mg kg–1 h–1. The infusion rate was increased according to the patient's response and to achieve a mean arterial pressure between 60 and 70 mmHg. However, it was decided not to exceed the maximal rate of propofol infusion above 12 mg kg–1 h–1. During the perioperative period, both groups received IV normal saline at 4 ml kg–1 h–1. Neuromuscular blockade was maintained with intermittent boluses of vecuronium. Normothermia was maintained during the whole procedure. The amount of blood loss was determined by collecting all the blood and rinsed fluid from the surgical field in suction canister into which 5 ml of 1:250 000 heparin had already been placed. Haemoglobin concentration was measured from the suction canisters and the blood samples obtained from the patients. The second anesthesiologist who was not involved in the study made visual assessment of blood-soaked gauze pieces used during the surgery. This was also added to the amount of blood loss. Injection diclofenac sodium 75mg i.m. was given to all patients 30 minutes before completion of procedure. Ondansetron 4 mg IV was given at the end of the surgery. The throat pack was removed at the end of the endoscopic procedure. The residual neuromuscular blockade was reversed with 0.05 mg/ kg of neostigmine and 0.01 mg/kg of glycopyrrolate IV. Patients were followed up and monitored for pain, nausea and vomiting in the post-operative period for 48 hours. For evaluation of the visibility of the operative field during surgery, quality scale proposed by Fromm and Boezaartwas used4,5. The operative field conditions were assessed by the same operating surgeon as: Grade 0: No bleeding. Grade 1: Slight bleeding – No suctioning of blood required. Grade 2: Slight bleeding – Occasional suctioning required. Surgical field not threatened. Grade 3: Slight bleeding – Frequent suctioning required. Bleeding threatens surgical field a few seconds after suction is removed. Grade 4: Moderate bleeding – Frequent suctioning required. Bleeding threatens surgical field directly after suction is removed. Grade 5: Severe bleeding – Constant suctioning required. Bleeding appears faster than can be removed by suction. Surgical field severely threatened and surgery impossible. Blood loss was estimated by measuring the weight of dry and blood soaked gauze before and after surgery and by collecting and measuring all blood lost and rinsed fluid from surgical field into suction canisters which are heparinised (5ml of 1:250000 heparin is added) and estimating the Hb concentration of the fluid in the canister using the formula: Amount of blood = Hb (g/dL) X V(ml) / Hbm (g/dL). Hb – Haemoglobin concentration of suction canister. V – fluid volume of suction canister. Hbm - Patient’s mean Hb concentration at beginning and end of surgery (average of haemoglobin one and haemoglobin two). Serum lactate was measured from blood samples during induction, 20 minutes and 40 minutes after induction and 30 minutes and 60 minutes after recovery. The information collected regarding all the selected cases were recorded in a Master Chart. Data analysis was done with the help of computer using Epidemiological Information Package (EPI 2010) developed by Centre for Disease Control, Atlanta. Using this software range, frequencies, percentages, means, standard deviations, chi square and 'p' values were calculated. Student’s ‘t’ test was used to test the significance of difference between quantitative variables and Yate’s chi square test for qualitative variables. A 'p' value less than 0.05 is taken to denote significant relationship. Sixty patients belonging to ASA physical status 1 and 2were enrolled after getting informed consent and randomly allocated to the two groups by lottery method. Both groups were comparable in age, weight and gender variability Table 1: Age distribution
Table 2: Sex distribution
Table 3: Weight distribution
Table 4: Change in serum lactate values
There is slight increase in serum lactate level in both the study groups with onset of hypotension, but within the physiological limits. However, serum lactate level in both the groups returned to the baseline values within 60mts of recovery.
Table 5: Changes in weight of gauze
Both study population showed increase in weight of the guaze of around 20 grams.
Table 6: Fluid volume of suction
Table 7: Haemoglobin %
Table 8: Blood loss
Table 9: Duration of surgery
Duration of surgery in isoflurane group is 86-165 minutes and in propofol group is also 83-165 minutes.
Table 10: Grading of operating field
In isoflurane group, 46.7% of patients had grade 2 quality of operating field, 46.7% patients had grade 3 quality of operating field and 6.7% of patients had grade 3 quality of operating field. In propofol group, 50% of patients had grade 2 quality of operating field, 43.3% patients had grade 3 quality of operating field and 6.7% of patients had grade 3 quality of operating field.
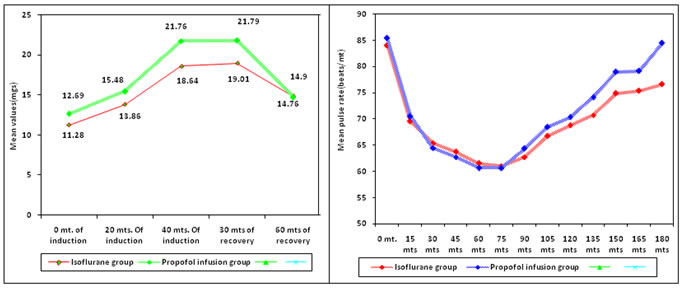
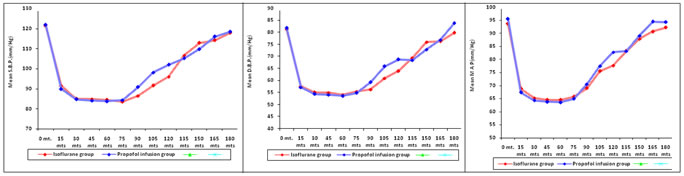
Figure 1 Figure 2 Figure 3 Figure 4 Figure 5
There was no significant difference in heart rate, systolic blood pressure, diastolic blood pressure or mean arterial pressure between the two groups at all times. DISCUSSION Our study is intended to measure and compare the pattern of serum lactate in patients during the episodes of controlled hypotension using propofol versus isoflurane undergoing functional endoscopic sinus surgery to uncover the metabolic evidence of cellular hypoxia. Because hyperlactataemia results from anaerobic metabolism, in response to inadequate cellular oxygen delivery. It is often used as a marker of oxygen delivery and circulatory status2. At 0 minutes of induction, the serum lactate level in isoflurane group was 11.28± 2.1 and in propofol group was 12.69± 3.32. These values were taken as the baseline values. Their p value was 0.0531, statistically insignificant. At 20 minutes of induction, controlled hypotension had been induced in patients of both groups. The serum lactate level in isoflurane group was 13.86± 3.8 and in propofol group was 15.48± 4.14. Both the groups of patients showed slight elevations from their baseline values, but remain within the physiological limits which was statistically insignificant (p=0.102). At 40 minutes of induction, the serum lactate level in isoflurane group was 18.64± 5.13 and in propofol group was 21.76± 8. Both the groups of patients showed progressive elevations in serum lactate levels from their baseline values, but remain within the physiological limits and the p value was statistically insignificant(p=0.0781). At 30 minutes of recovery, in the post operative period, the serum lactate level in isoflurane group was 19.01± 4.83 and in propofol group was 21.79±6.02. Both the groups of patients show slight elevationsin serum lactate levels from their levels at 40 minutes of induction, but remain within the physiological limits which was statistically insignificant(p=0.0532). At 60 minutes of recovery, in the post operative period, the serum lactate level in isoflurane group was 14.7± 4.83 and in propofol group was 14.76±3.12. Both the groups of patients showed decrease in serum lactate levels from their levels at 30 minutes of recovery, returning towards its baseline values and it was statistically insignificant (p=0.9481). Our results showed that there is slight rise in serum lactate level with onset of hypotension in both group of patients suggesting minimal metabolic disturbances, but within physiological limit and serum lactate level returns to its baseline values after 60 min of recovery from hypotension in both groups. There are no significant differences in lactate values between two groups. These findings are consistent with the study conducted by M.C.Newton et al6. In the study conducted by Nicholas et al3, during the period of hypotension there were, in most cases, slight elevations in serum lactate, pyruvate, lactate pyruvate ratio and potassium. They concluded that the minimal metabolic disturbances of hypotensive spinal anesthesia do not indicate that cellular hypoxia exists. In our study, though there is rise in serum lactate levels, but it doesn’t cause any major metabolic derangements, as the serum lactate level always reminded within the physiological limits (9-36mg/dL)7,8. Blood loss assessment in our study measured in two methods. Change in weight of the guaze. Isoflurane group showed mean increase in weight of guaze by 19.1±3.17 gram and in propofol group, it is by 20.3±4.39 grams. The p value (0.2294) was insignificant. Amount of blood loss (ml) = Hb (g/dL) X V(ml) / Hbm (g/dL)(17). Hb – Haemoglobin concentration of suction canister V – fluid volume of suction canister Hbm - patient’s mean Hb concentration at beginning and end of surgery Haemoglobin concentration of suction canister in isoflurane group was 0.88± 0.55g/dl and in propofol group was 0.98±0.5g/dl.Their p value was 0.4641, statistically insignificant. Fluid volume of suction canistercanister in isoflurane group was1.41± 0.34 L and in propofol group was 1.3±0.21 L. Their p value was 0.1243, statistically insignificant. Pre-induction Haemoglobin concentration of patients in isoflurane group was 13.02± 1.24 g /dl and in propofol group was 13.15±0.99 g/dl. Their p value was 0.6631, statistically insignificant. Post operative Haemoglobin concentration of patients in isoflurane group was 11.81± 1.32 g /dl and in propofol group was 11.94±1.04 g/dl. Their p value was 0.6728, statistically insignificant. Amount of blood loss (ml) calculated by using the above formula showed that blood loss in isoflurane group was 105.2±80.8ml and in propofol group was 102.5±57.1ml. Their p value was 0.8842, statistically insignificant. The technique of controlled hypotension can reduce the blood loss in FESS by between 80 to 140 millilitres. The intra operative blood loss in the study conducted by Saravanan P Ankichetty et al9 in isoflurane group was 132.5±92.15 ml and in propofol group was 109±82.96ml suggest that controlled hypotension in decreasing intraoperative blood loss in our surgery was effective. In isoflurane group, duration of surgery was 118.7±22.2 minutes and in propofol group, it was 115.9±23.4 minutes. Their p value was 0.6433, statistically insignificant. The duration of surgery was less with propofol group when compared to isoflurane group [131(±36) vs. 98(±41) min, P = 0.01] in the study by Saravanan P Ankichetty et al9. But in our study, duration of surgery in both group of patients does not show any significant difference. For evaluation of the visibility of the operative field during surgery, quality scale proposed by Fromm and Boezaart was used5,11. The operative field conditions were assessed by the same operating surgeon.In isoflurane group, 46.7% of patients had grade 2 quality of operating field, 46.7% patients had grade 3 quality of operating field and 6.7% of patients had grade 3 quality of operating field. In propofol group, 50% of patients had grade 2 quality of operating field, 43.3% patients had grade 3 quality of operating field and 6.7% of patients had grade 3 quality of operating field. The heart rate changes were monitored and compared at every 5 minutes interval of time both intra operatively and postoperatively one hour from recovery. The heart rate was maintained below 70 per minute intraoperatively throughout the procedure in both groups. Heart rate changes were manageable intraoperatively, without the need for inj. Atropine or any inotropic support. Our study was intended to achieve induce controlled hypotension with the mean arterial blood pressure in the range between 60-70mmHg[10]. The mean arterial blood pressure was maintained in the range between 60-70 mmHg in both group of patients intra-operatively throughout the procedure and the mean arterial blood pressure was monitored for one hour from recovery, post operatively for any fall in mean arterial blood pressure. None of the patients required any inotropic support both intra-operatively and post operatively. None of the patients had intraoperative or postoperative complications
CONCLUSION Our study concludes that there is a slight rise in serum lactate level with onset of hypotension in both groups of patients suggesting minimal metabolic disturbances, but within physiological limit and serum lactate level returns to its baseline values after 60 min of recovery from hypotension in both groups. There are no significant differences in lactate values between two groups
REFERENCES
|
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
 Home
Home