Official Journals By StatPerson Publication
|
Table of Content Volume 8 Issue 1 - October 2018
Effects of addition of dexmedetomidine to bupivacaine on the block characteristics of brachial plexus block by supraclavicular approach
C S Prakash1, S Vigneshwaran2*
1Professor, 2PG Student, Department of Anaesthesiology, Rajah Muthiah Medical College, Annamalai University, Chidambaram, Tamil Nadu, INDIA. Email: drvigneshtvmc@gmail.com
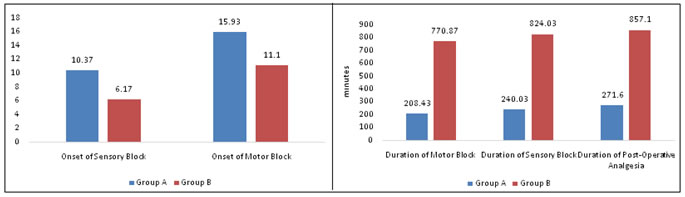
Abstract Background: Dexmedetomidine, a non-opioid adjuvant to neural blockade supposed to improve the quality of nerve blockade. This study intends to compare the effects of addition of dexmedetomidine as an adjutant to bupivacaine for supraclavicular brachial plexus block. Methods: A prospective, double blinded, randomized control study was conducted on 60 adult patients scheduled to undergo elective upper limb orthopedic procedures under regional anaesthesia. The patients were divided into two groups by randomization. Group A patients received 30ml of 0.325% bupivacaine containing 0.3 ml of distilled water.Group B patients received 30ml of 0.325% bupivacaine containing 0.3 ml of dexmedetomidine (30 mcg). Onset of sensory, motor blockade, duration of sensory and motor blockade, duration of post-operative analgesia and adverse effects, if any, were observed. Results: Demographic profile between two groups of patients were comparable. Mean(SD) time of onset of sensory block and motor blockade between group A vs Group B were 10.37 ±2.86 vs 6.17±1.58, 15.93±2.30 vs 11.10±2.12 . Mean (SD) duration of sensory and motor blockade between group A vs Group B were 240.03 ±39.84vs 824.03± 38.05, 208.43± 33.47 vs 779.87± 32.91 . Mean (SD) Duration of post-operative analgesia was 271.60±37.92 vs 857.10 ±37.83 .Statistically highly significant difference was observed between Group A and Group B patients in terms of onset of sensory, motor blockade, duration of sensory, motor blockade and duration of post-operative analgesia (p<0.001) Conclusion: Dexmedetomidine added as an adjuvant to bupivacaine for supraclavicular brachial plexus block has superior quality of sensory and motor blockade with prolonged postoperative analgesia with negligible adverse events. Key Words: Brachial plexus block, bupivacaine, dexmedetomidine, supraclavicular approach.
Regional anaesthesia has better intraoperative and postoperative outcome than general anaesthesia. Regional nerve block was first introduced by surgeons Halsted and Hall using a local anaesthetic cocaine in peripheral nerves1,2. Supraclavicular brachial plexus block is a very popular mode of anaesthesia first introduced by Kulenkampff in 19113. It is used for various upper limb surgeries, due to its effectiveness in terms of cost and performance, margin of safety and good post-operative analgesia. A variety of adjuvants4, like clonidine, buprenorphine, dexamethasone, sodium bicarbonate, tramadol, midazolam etc. have been added to local anaesthetics as adjuvants for regional nerve blockade. Dexmedetomidine, an α2 agonist used as adjuvant to epidural5,6 and spinal anaesthesia7,8 produces superior quality of nerve blockade with less adverse effects than other adjuvants. Dexmedetomidine, a non-opioid adjuvant to neural blockade is supposed to improve the quality of nerve blockade9,10. This study intends to compare the effect of combination of dexmedetomidine with bupivacaine alone for supraclavicular brachial plexus block.
METHODS A prospective double blinded randomized control study was conducted on 60 adult patients of either sex with ASA physical status I and II admitted in Rajah Muthiah Medical College and Hospital, who are scheduled to undergo elective upper limb orthopedic procedures under regional anaesthesia . Patients were randomly allocated to one of the two groups using a standard randomization code. (Group A, Group B) Exclusion Criteria
Procedure: After through history taking and clinical examination, all basic investigations like complete blood count, renal function test, serum electrolytes, electrocardiogram, chest x ray were done. An intravenous line was secured with 18 gauge venous cannula before undertaking the procedure and continued throughout the length of surgery. Routine vital parameter like pulse oximetry, non invasive blood pressure, electrocardiogram were monitored. The patients were randomized using random number technique and divided into two equal groups: Group A: Patients received 30ml of 0.325% bupivacaine containing 0.3 ml of distilled water. Group B: Patients received 30ml of 0.325% bupivacaine containing 0.3 ml of dexmedetomidine (30 mcg). The Study drug solutions was prepared in sterile container by an anesthetist not involved in the study and the person performing the block and observing the patient was blinded to ensure double blinding. The patient as positioned supine with neck in extension, supported by a roll under the shoulder and the head turned away from the side to be injected. A classical subclavian perivascular technique was followed for supraclavicular brachial plexus block. A 22 gauze short bevel 3.5cm needle was used to perform this technique. Under all aseptic precautions 1 ml of 2% lignocaine was infiltrated subcutaneously at the injection site. Using a landmark technique with subclavian artery as a guide, the needle was inserted 1 cm above the midpoint of the clavicle lateral to the pulsation of the subclavian artery and forwarded caudally in the horizontal plane, parallel to the neck to enter the fascial sheath 1 to 2 cm deep to the skin. After eliciting paresthesia, careful negative aspiration was done to exclude intravascular placement and study drug solution 30 ml was injected. Sensory blocks were evaluated by pin prick test using 3 point scale and grades as: 0-Normal sensation,1- Loss of pin prick sensation, 2- Loss of anaesthesia. Quality of Motor block was measured using Upper Limb Bromage 3 Point Score and graded as:0-normal motor function with full flexion and extension of elbow, wrist and fingers,1-decreased motor strength with ability to move fingers and or wrist only, 2-complete motor blockade with inability to move fingers also. Onset of sensory block is defined as the time interval between the injection of total local anaesthetic and complete sensory blockade. Onset of motor block is defined as the time interval between the total local anaesthetic administration and complete motor blockade .Duration of motor block is defined as the time interval between the total motor block and complete resolution of motor blockade. Duration of sensory block is defined as the time interval between the complete sensory block and resolution of anaesthesia of all nerves. Post-operative follow up was carried out in the recovery and post-operative ward. The duration of analgesia was noted according to 0-10 visual analogue score (VAS) for pain evaluated every half an hour for first 10 hours and then hourly till 24 hours. When the patients began to experience the worst pain (VAS =8-10), it was considered that analgesic action of the drugs was terminated and rescue analgesic (1g paracetamol infusion or tramadol 2 mg/kg intravenously) given. Adverse events if any like drowsiness, nausea/vomiting, hypotension (a 20% fall from base line value), bradycardia (<50 beat/min), respiratory depression noted. During the procedure, anaesthesia was considered satisfactory if the patient did not complain of any pain or discomfort and if no sedation was necessary. In the circumstance of inadequate blockade, undue prolongation of surgery, the block has been supplemented with general anaesthesia and excluded from the study. Descriptive statistical analysis was performed with SPSS PASW 20 software. P values less than 0.05 were considered as significant (P<0.05).
RESULTS Table 1: Demographic and surgical profile of patients were comparable between both groups (Table 1)
*NS- Not statistically significant Onset time of sensory and motor blockade was earlier in Group B (Dexmedetomidine) when compared with Group A (P<0.01). Duration of Sensory and Motor blockade was prolonged in Group B when compared with Group A (P<0.01). Table 2: Block Characteristics
Figure 1 Figure 2 Figure 1: Mean duration of onset of sensory and motor blockade between 2 groups; Figure 2: Mean duration of sensory and motor blockade, Postoperative analgesia between the two groups
The duration of postoperative analgesia in Group A (control) is 271.60±37.92 minute and group B (dexmedetomidine) is 857.10 ±37.83 minute, which is statistically significant (p <0.01). Mean duration of postoperative analgesia is prolonged in dexmedetomidine group (14.2 hours). Vital parameters like mean pulse rate, systolic blood pressure, mean respiratory rate and mean arterial saturation values were similar in both the groups. The side effects were found to be insignificant and incidental. DISCUSSION Peripheral nerve blocks are preferred as an alternative or as an adjunct to general anaesthesia, as well as for postoperative analgesia for a wide variety of procedures. With the use of continuous catheter techniques, use of adjuvants become common. Bupivacaine, a local anaesthetic has longer duration and faster onset of action. In this study we compared bupivacaine alone and bupivacaine with dexmedetomidine for supraclavicular brachial plexus block. Dexmedetomidine, a highly selective α2 adrenoceptor agonist with α2:α1 binding selectivity ratio of 1620:1 decreases the unwanted side effects of α1 receptors11, 12. Presynaptic activation of α2 adrenoceptor in central nervous system (CNS) inhibits the release of norepinephrine, terminating the propagation of pain signals and their postsynaptic activation inhibits sympathetic activity, thereby decreasing HR and BP.12,13. High selectivity for α-2A receptors mediates analgesia, sedation, and anxiolysis. Dexmedetomidine used in central neuraxial blockade like spinal,14,15 epidural16, caudal anaesthesia 17, has superior quality of anaesthesia with negligible adverse effects . Its effects on spinal α2 receptors, prolongs the neural blockade by hyperpolarization of unmyelinated C fibers (sensory) and to a lesser extent the A fibers (motor), when used as an adjuvant to local anaesthetics for neuraxial blocks18. In this study there was no significant differences between the study groups with respect to pattern of changes in heart rate, systolic blood pressure, diastolic blood pressure post operatively. Onset of Sensory blockade and Motor blockade: In our study, we observed that onset time of Sensory blockade was earlier in dexmedetomidine group (Group B) having a mean value of 6.17 ± 1.58 minutes in comparison with bupivacaine group (Group A) having a mean value of 10.37± 2.86 minutes, which is statistically significant. P < 0.01 In our study, we observed that onset time of Motor blockade was earlier in dexmedetomidine group (Group B) having a mean value of 11.10 ± 21.2 minutes in comparison with Bupivacaine group (Group A) having a mean value of 15.93± 2.30 minutes, which is statistically significant. P < 0.01 Sandhya Agarwal et al 10,Rajesh Meenaet al 19, Obayah GM et al 20, observed that dexmedetomidine added as an adjuvant to bupivacaine shortens the onset time of sensory and motor blockade. Duration of Sensory block and Motor block: In our study the duration of motor block was 779.87 ± 32.91 minutes with dexmedetomidine group and 208.43 ± 33.47 minutes with bupivacaine group. The duration of motor block was longer in dexmedetomidine group compared with Bupivacaine group, which is statistically significant. P < 0.01 The duration of Sensory block was 824.03 ± 38.05 minutes with dexmedetomidine group and 240.03 ± 39.84 with Bupivacaine group. The duration of sensory block was longer in dexmedetomidine group compared with Bupivacaine group, which is statistically significant. El-Boghdadly K et al 21, Kenan Kaygusuz et al22, found that dexmedetomidine as a local anaesthetic adjunct for brachial plexus block enhances duration of sensory and motor blockade. Duration of Post-Operative Analgesia: The mean time from onset of block to request of analgesics was taken as total duration of analgesia. The duration of analgesia was 857.10 ± 37.83 hours with dexmedetomidine group (Group B) and 271.60 ± 37.92 hours with Bupivacaine group (Group A) in our study. The duration of analgesia was longer in dexmedetomidine group compared with Bupivacaine group, which is statistically highly significant. P<0.001 Amany S. Ammar et al 23, ArchanaTripathi et al 24, Rachana Gandhi et al 25 concluded that dexmedetomidine in combination with bupivacaine prolongs the duration of analgesia in supraclavicular brachial plexus block.
CONCLUSION Dexmedetomidine added as an adjuvant to bupivacaine for supraclavicular brachial plexus block has superior quality of sensory and motor blockade with prolonged postoperative analgesia with negligible adverse events.
REFERENCES
|
|
 Home
Home