Official Journals By StatPerson Publication
|
Table of Content Volume 8 Issue 1 - October 2018
Comparison of two doses of intravenous Dexmedetomidine 0.6mcg/kg and 1mcg/kg given prior to induction in attenuation of hemodynamic stress response of laryngoscopy and endotracheal intubation
R Arun Shankar1, M S Prasanth Kumar2*, G Dhanabagyam3
1Sr. Resident, 2Associate Professor, 3Professor, Department of Anaesthesiology, PSG Institute of Medical Sciences and Research, Peelamedu, Coimbatore – 641004, Tamil Nadu, INDIA. Email: drprasanth1979@yahoo.co.in
Abstract Background: Laryngoscopy and endotracheal intubation is accompanied by sympathomimetic stimulation resulting in increase in Heart Rate and Arterial blood pressure. These hemodynamic adverse effects are minimized by multiple non pharmacological methods and pharmacological agents including alpha 2 agonists such as Dexmedetomidine. Dexmedetomidine has a shorter duration of action and effectively attenuates the hemodynamic response of laryngoscopy and endotracheal intubation during the peri operative period. The aim of our study is to compare two doses (0.6mcg/kg and 1mcg/kg) of the drug in effective attenuation of the sympathetic stimulation. Methodology: 80 patients assessed under ASA 1 – 2 between the age group 18-60 years of both genders were included in this study and randomly divided into two groups namely GROUP A – 0.6mcg/kg Dexmedetomidine and GROUP B – 1mcg/kg of the same drug 10mins before induction. Heart rate, Systolic Blood pressure, Diastolic blood pressure, Mean arterial pressure and SpO2 were recorded at various intervals. Results: In both groups, HR, SBP, DBP and MAP reduced significantly. During intubation, 1 and 3 minutes following intubation there was minimal rise in blood pressure in Group A while in Group B the decrease in pressure was marked and continuous. Conclusion: Both doses of Dexmedetomidine (0.6mcg/kg and 1mcg/kg) attenuated the stress response of laryngoscopy and intubation effectively. The reduction in heart rate, Systolic blood pressure, Diastolic blood pressure and Mean arterial pressure was more in 1mcg/kg group. Hence Dexmedetomidine at a dose of 0.6mcg/kg itself is adequate to control the stress response of laryngoscopy and intubation. Key Words: Attenuation; Laryngoscopy; Intubation; Dexmedetomidine.
Laryngoscopy and endotracheal intubation is accompanied by intense sympathomimetic stimulation resulting in increase in Heart Rate (HR) and arterial Blood Pressure (BP). This response is very hazardous in patients with reduced myocardial reserve / hypertension / cerebro-vascular insufficiency / raised intracranial or intraocular pressure and may predispose to pulmonary edema / myocardial infarction / cerebro-vascular accident1,2,3/ dysrhythmias. To minimize these hemodynamic adverse effects, multiple non pharmacological methods (minimizing mechanical stimuli of laryngoscopy by blind nasal intubation5, reducing time of laryngoscopy to < 15 seconds6) and various pharmacological agents have been tried which act at different levels of reflex arc4. Dexmedetomidine is a lipophilic α methylol derivative which has sedative, anxiolytic and analgesic effects7. It is a highly selectiv alpha 2 agonist (1620 times highly selective to α2 receptor) and has a shorter duration of action. Dexmedetomidine administered at a dose of 1 mcg/kg IV over 10 minutes, 15 minutes prior to the procedure, effectively attenuates the hemodynamic response during the peri-operative period8,9,10,11 but it is associated with side effects like bradycardia and hypotension. The aim of our study was to compare the efficacy of Dexmedetomidine in reducing the hemodynamic stress response in two different doses (0.6 mcg/Kg and 1 mcg/Kg body weight) which was given prior to laryngoscopy and endotracheal intubation
MATERIAL AND METHODS After getting the institutional ethical committee clearance, the study was conducted in PSG institute of medical sciences and research, Coimbatore. Patients aged 18-60years belonging to both genders, assessed under ASA 1 – 2 with Mallampatti class I- II were included in the study. Patients with hypertension, bradycardia, cardiac disease, coronary artery disease, cerebro vascular disease, difficult airway, BMI > 30 Kg/ m2, on β blocker therapy or known hypersensitivity to the study drug were excluded. 80 patients who fulfilled the inclusion criteria were included in the study and informed consent was obtained. They were premedicated with Tab. Alprazolam 0.5 mg and Tab. Ranitidine 150 mg on the night before surgery. Patients were randomly allocated to one of the following two groups by random table number generated by computer. The procedure was double blinded wherein the consultant anaesthesiologist prepared the infusion of the study drug in 100ml normal saline and handed over to the resident. Hence, the resident conducting the study and the patient both were blinded to the group of drug. The two study groups were labelled as follows - Group A: 0.6 mcg/kg Dexmedetomidine Group B: 1 mcg/kg Dexmedetomidine After preoxygenation, Inj.Glycopyrrolate 0.2 mg i.v, Inj.Fentanyl 2 mcg /kg i.v was given and induced with Inj.Thiopentone sodium till the abolition of the eyelash reflex. After confirming the adequacy of mask ventilation, inj. Succinylcholine 1.5 mg/kg was given and intubated after a minute. Anesthesia was maintained with Oxygen, Nitrous oxide, Isoflurane 1% and inj. Vecuronium bromide. The duration for laryngoscopy and intubation was recorded. Heart rate, systolic BP, diastolic BP, mean arterial BP and SpO2 were recorded before and after induction, at the time of intubation (0 minute), 1st min, 3rd min, 5th min and 10th min after intubation. Surgical stimulus was avoided for 10 minutes after intubation. Adverse effects were noted and treated accordingly as follows
Statistical Analysis: Statistical analysis was performed using the statistical software (SPSS) 19.0. Data was expressed as percentages and mean values (with standard deviations). Differences between groups were analyzed with the Independent Sample t-test for continuous variables and Pearson’s Chi-square test for categorical variables. Paired sample t-test was used to compare the difference between pre and post values. Results were defined as statistically significant when the P value was less than 0.05. OBSERVATIONS AND RESULTS Table 1: Age distribution between two groups
Table 2: Sex distribution between two groups
There was no significant statistical difference in the sex and age distribution between the two groups. Table 3: Side effects in two groups
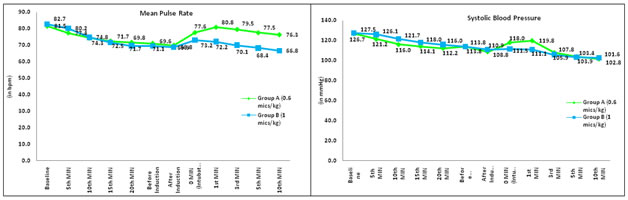
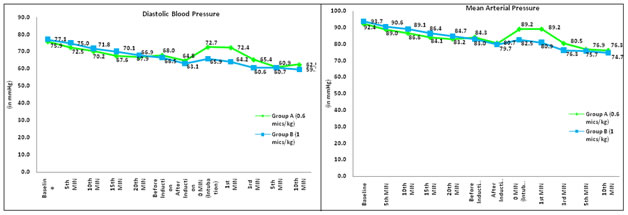
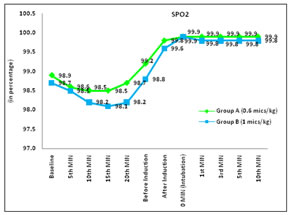
There was no significant statistical difference between the two groups with regard to side effects (p value 0.602). Figure 1 Figure 2 Figure 3 Figure 4 Figure 5 Figure 1: Intergroup comparison for heart rate between Group A and Group B; Figure 2: Intergroup comparison for SBP between Group A and Group B; Figure 3: Intergroup comparison for DBP between Group A and Group B; Figure 4: Intergroup comparison for MAP between Group A and Group B; Figure 5: Intergroup comparison for SpO2 between Group A and Group B Figure 1, In group A, the basal mean heart rate was 81.58 ± 8.86 bpm. The mean heart rate after administration of the study drug at 5 th, 10 th, 15 th, 20 th min, before induction, after induction, at the time of intubation was 77.40 ± 11.06, 74.30 ± 11.31, 72.58 ± 10.69, 71.72 ± 10.41, 71.10 ± 9.76, 69.90 ± 11.65, 77.63 ± 10.89 respectively and showed a significant reduction from mean heart rate (p value <0.05). No change was noted in the 1st and 3rd minute following intubation. The reduction in heart rate started from the 5th minute following intubation onwards (p value < 0.05). In group B, the basal mean heart rate was 82.70 ± 4.48 bpm. The mean heart rate reduced after administration of the study drug at the 5th, 10th, 15th, 20 th min, before induction and after induction. Further fall in the heart rate was noted during intubation and 1st, 3rd, 5 th, 10 th min following intubation (p value <0.05), The baseline heart rate was comparable in both the groups as p value of 0.476. However 5th, 10th, 15th, 20th min, just before and post induction there was no statistical significance as the p value was > 0.05. There was a significant difference in the mean heart rate of the two groups at the time of intubation, 1st, 3rd, 5th, 10th min after intubation (p value < 0.05). Figure 2, In group A, the basal mean SBP was 126.70 ± 12.07 mmHg. The mean SBP after administration of the study drug at the 5 th, 10 th, 15 th, 20 th min, before induction and after induction were 121.20 ± 10.92, 116.05 ± 12.53, 114.13 ± 11.90, 112.20 ± 11.26, 113.83 ± 14.24 and 108.83 ± 14.75 mmHg respectively. There was a subsequent fall in mean SBP following intubation also. (p <0.05) In group B, the basal mean SBP was 127.58 ± 6.33 mmHg. Significant reduction in the mean SBP was seen constantly thereafter till the measurements were noted (p <0.05). The baseline mean SBP was comparable in both the groups (p value - 0.686). There was a significant reduction in the 5th and 10th min following administration of the study drug and at the 1st min after intubation ( p value < 0.05). Figure 3, In group A, the basal mean DBP was 75.97 ± 5.96 mmHg. The mean DBP after the administration of study drug at 5th, 10th, 15th, 20th min, before induction and after induction was 72.58 ± 6.79, 70.20 ± 7.30, 67.68 ± 8.31, 66.95 ± 7.17, 68.00 ± 10.44, 64.80 ± 12.36 mmHg respectively. This showed highly significant reduction of mean DBP from baseline (p value 0.000). But at the time of intubation and 1st min after intubation the mean DBP showed no change. However, Statistical significance was noted during 3rd, 5th and 10th min after intubation with p value < 0.05. In group B, the basal mean DBP was 77.18 ± 5.28 mmHg. The mean DBP after the administration of the study drug was constantly less than the baseline (p value 0.000). There was a significant difference in the mean DBP between the two groups at the time of intubation, 1st and 3rd min after intubation (p value less than 0.05). Figure 4, In group A, the basal mean MAP was 92.48 ± 6.83 mmHg. The mean MAP after the administration of study drug at 5th, 10th, 15th, 20th min, before induction, after induction were 89.00 ± 7.68, 86.68 ± 8.81, 84.18 ± 9.47, 83.23 ± 7.73, 84.35 ± 10.25, 80.70 ± 12.94 mmHg respectively and showed a significant reduction of mean MAP (p value < 0.05). There was no statistical significance at the time of intubation and 1st min after intubation, but the mean MAP at the 3rd, 5th and 10th min after intubation were 80.53 ± 11.65, 76.90 ± 10.34, 76.35 ± 9.28 mmHg respectively, suggestive of a significant reduction from baseline ( p value 0.000). In group B, the basal mean MAP was 93.78 ± 4.33 mmHg. There was a significant reduction of the mean MAP from the 10th minute onwards following administration of the drug from the baseline value (p value was 0.000). There was a significant difference in mean MAP at the time of intubation and 1st min after intubation in both the groups (p value of less than 0.05). Figure 5, In group A, the basal mean SpO2 was 98.93 ± 0.69. The mean SpO2 after the administration of study drug at 5th, 10th min were 98.63 ± 1.33, 98.50 ± 1.21 respectively and showed a significant reduction from baseline value ( p value < 0.05). The mean SpO2 after induction till 10th min was comparable to baseline value with (p value 0.000). In group B, the basal mean SpO2 was 98.78 ± 1.00. The mean SpO2 after the administration of study drug at 5th, 10th, 15th, 20th min from baseline and till 10th min post induction showed significant change from baseline value (p value < 0.05). There was no significant difference in mean SpO2 between two groups (p value >0.05).
DISCUSSION Multiple non pharmacological methods and pharmacological agents have been tried before intubation to attenuate the hemodynamic adverse effects of laryngoscopy and intubation that act at different levels of the reflex arc. The commonly used pharmacological agents are iv Fentanyl, Morphine, Lignocaine, Beta Blockers, Calcium channel blockers, Magnesium Sulphate, Alpha 2 Agonists such as Clonidine and Dexmedetomidine. Dexmeditomidine is a highly selective alpha 2 agonist (1620 times highly selective to α2 receptor when compared to clonidine). In our study we compared the efficacy of Demeditomidine in attenuating the sympathetic stress response to laryngoscopy and intubation in two different doses (0.6 mcg/Kg and 1 mcg/Kg body weight ) when given prior to intubation. After administering the study drug, both groups showed a statistically significant fall in heart rate from the baseline till induction. In Group A, the post intubation heart rate increased but not more than the baseline value. In group B, there was a minimal increase in the heart rate during intubation and one minute post intubation while it decreased after that. To conclude the fall in heart rate was comparatively more in Group B than group A12. The fall in the systolic blood pressure from the baseline (126.70 ± 12.07 mm Hg) following administration of the drug upto 10 minutes post intubation in Group A was associated with a slight increase during intubation (118.03 ± 16.65 mm Hg)13.While in group B, a significant decrease in the systolic blood pressure (111.58 ± 15.30 mm Hg) from the baseline (127.58 ± 6.33 mm Hg) was noted after administrating the study drug with no increase during intubation (111.13 ± 10.06 mm Hg)11 {Menda et al}. Changes in Diastolic BP following administration of drug in Group A was similar to Systolic BP 14. The range of increase was 8 mmHg from induction value but not more than baseline value with a significant difference in the diastolic blood pressure from baseline till 10 minutes post intubation. In group B the fall in Diastolic BP was constant11, statistically significant and more when compared to Group A. A significant fall in the mean arterial pressure from the baseline till 10minutes post induction was recorded in Group A with a mild increase of 9mmHg above the induction value at the time of intubation and 1 minute post intubation. This finding was similar to the study done by Mowafi et al15 who observed that there was an increase in MAP of 5 mmHg from post induction value but less than basal value. The decrease in MAP was continous in Group B11. here was significant fall in SpO2 in both groups during the infusion of the study drug but post induction the SpO2 increased significantly probably due to pre oxygenation. In both groups, there was a marked reduction in dose requirement of Thiopentone for induction (Group A- 160.00 ± 15.19, Group B- 166.75 ± 23.73) than the usual dose required to anaesthetise patients16. In our study, 3 patients in each group developed hypotension and 1 patient in group A developed bradycardia which required pharmacological management.
CONCLUSION Both doses of Dexmedetomidine (0.6mcg/kg and 1mcg/kg) attenuated the stress response of laryngoscopy and intubation effectively. The reduction in heart rate, systolic blood pressure, diastolic blood pressure and mean arterial pressure was more in 1mcg/kg group. Hence Dexmedetomidine at a dose of 0.6mcg/kg itself is adequate to control the stress response of laryngoscopy and intubation.
REFERENCES
|
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
 Home
Home