Official Journals By StatPerson Publication
|
Table of Content Volume 8 Issue 1 - October 2018
Evaluation of adding clonidine to lignocaine during bier’s block in upper limb surgeries
Dhanasekaran C1, Nivedita B2*
1Professor, 2Postgraduate, Department of anaesthesiology, Rajah Muthiah Medical College, Annamalai University, Chidambaram, Tamil Nadu, INDIA. Email: nivedita.spartan@gmail.com
Abstract Background and aims: Bier’s block a.k.a Intravenous regional anaesthesia (IVRA) is used for short duration procedures for limb surgeries. IVRA provides reliable analgesia with good muscular relaxation of the extremity distal to the tourniquet, but tourniquet pain and absence of post-operative analgesia are the major drawbacks. In this study, the efficacy of adding clonidine as an adjuvant to IVRA for upper limb surgeries, was evaluated with respect to block characteristics, tourniquet pain and post-operative analgesia. Methods: A prospective, randomised, double-blind study was conducted on 60 adult patients of American Society of Anaesthesiologists grade 1 and 2, undergoing short duration upper limb surgeries. Patients were randomised into two groups of 30 each. One group received 40 ml of 0.5% preservative-free plain lignocaine and other group received clonidine 1µg/kg added to 40 ml of 0.5% plain lignocaine. Results: Sensory recovery time, sedation score and duration of post - op analgesia were significantly increased in clonidine group (p < 0.05). Sensorimotor block onset, motor recovery time and need for rescue analgesia were comparable in both the groups. Haemodynamic parameters were comparable. Conclusions: Clonidine significantly increased post-operative analgesia and sensory recovery time but it did not prevent tourniquet pain. Sedation scores were higher in clonidine group. Key Word: Intravenous regional anaesthesia, clonidine, tourniquet pain
INTRODUCTION Bier’s block a.k.aIntravenous regional anaesthesia (IVRA) was first introduced by German surgeon August Gustav Bier in 19081.This technique gained popularity after reintroduction by Holmes in the late 1960s2.IVRA is technically simple and provides rapid analgesia with success rate of around 90%3. The rapid return of sensory and motor power after surgery, aids in rapid recovery facilitating early discharge of patients. Drawbacks of IVRA are torniquet pain and absence of post - operative analgesia. Various additives like opioids, muscle relaxants, NSAIDs and alpha 2 agonists like clonidine and dexmedetomidine have been used to overcome these disadvantages and improve analgesia4. In our study, we evaluated the addition of clonidine to lignocaine during Bier’s block in upper limb surgeries. Aprospective randomized double blind control study was conducted after obtaining approval from the ethical committee. 60 patients of ASA grade 1 and 2 who came for upper limb surgeries lasting less than 90 minutes, between 18 and 55 years of age of either sex were included in the study. Patients who were not willing for IVRA, allergic to the study drugs, raynaud’s disease, sickle cell anemia, infection in the extremity to be used and patients with significant cardiovascular and respiratory diseases were excluded from the study. The study population were divided into 2 groups of 30 each randomly. One group received 40 ml of 0.5% lignocaine (Group L) and the other group received 40 ml of 0.5% lignocaine with 1µg/kg clonidine (Group C). Patients were kept nil per oral overnight according to ASA guidelines and premedicated with Tablet Ranitidine 150 mg and Tablet Diazepam 5 mg, the night prior to the surgery and morning of surgery. Informed consent for surgery and anaesthetic procedure was obtained. Materials needed for the study including anaesthesia machine, resuscitation equipment, emergency drugs were checked and kept ready before the arrival of the patient in the operating room. Starvation status and informed consent confirmed in the preoperative holding room before the patient was shifted inside the operating room. Patients were connected to monitors like electrocardiography, non Invasive blood pressure and pulse oximeter. The initial pulse rate, blood pressure and oxygen saturation were recorded and then continuous monitoring was done during the procedure. A 22G cannula was placed intravenously as distal as possible in the limb to be anaesthetized. Venous access was established in the opposite limb to allow administration of fluids and drugs if necessary. After adequate padding of the operative limb, double pneumatic tourniquet was applied. The operative limb was exsanguinated by using Esmarch bandage. Proximal tourniquet was inflated to 100 mmHg higher than the patient’s systolic blood pressure. Absence of the radial pulse and the loss of pulse oximetry tracing confirmed the circulatory isolation of the operative limb. Solutions were injected by an anesthesiologist blinded to the study drugs. Patient were divided into two groups according to the drug which they received. After injecting the drugs sensory and motor blocks were assessed. After complete sensory and motor blocks were achieved, distal tourniquet was inflated and the proximal one was deflated. 22 G cannula was removed from the anaesthetized limb and the surgery was allowed to proceed. Intra - operatively heart rate, blood pressure, oxygen saturation, visual analog scale and ramsay sedation score were recorded at 5, 10, 15, 20, 30, 40, 50, 60, 75 and 90 minutes after tourniquet application. If patients complained of tourniquet pain (VAS >3) they were supplemented with Injection. Fentanyl 1µg/kg intravenously and the requirement for rescue analgesics were recorded. Tourniquet should not be deflated upto 30 minutes after injection of local anesthetics, even if the surgery was completed before 30 minutes and it should not be inflated more than 90 minutes. Cuff deflation was performed in cycles with deflation/ inflation times of less than 10 seconds to avoid systemic toxicity. After tourniquet deflation duration of sensory, motor blockade and time for first analgesic requirement were noted. Patients were monitored for both intra - operative and post - operative complications. Statistical Analysis: The collected data were analysed with IBM.SPSS statistics software 23.0 Version. To describe about the data descriptive statistics frequency analysis, percentage analysis were used for categorical variables and the mean and standard deviation were used for continuous variables. To find the significant difference between the bivariate samples in paired groups the Paired sample t-test was used and for independent groups the Unpaired sample t-test was used. To find the significance in categorical data Chi-Square test was used, similarly if the expected cell frequency is less than 5 in 2×2 tables then the Fisher's Exact was used. In all the above statistical tools the p value ≤ 0.05 was considered as significant level.
RESULTS Both groups were comparable with respect to age, sex, weight, baseline HR/MAP, duration of surgery, sensorimotor onset, motor recovery and rescue analgesia (Table 1)
Table 1: Comparison Between Groups With Respect To Demographic Profile, Vital Signs, Surgical Duration, Sensorimotor Onset, Motor Recovery And Rescue Analgesia
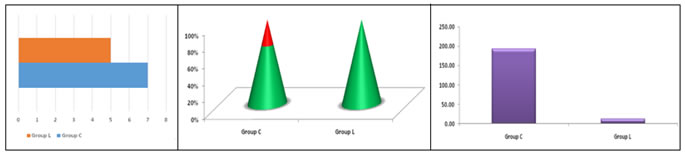
Values (except sex distribution and rescue analgesia) are mean ± standard deviation; MAP - Mean arterial pressure; HR - Heart rate. Sensory recovery time after the release of torniquet was 6.57 ± 1.135 min. in group C and 4.80 ± 0.714 min. in group L which was statistic all significant (p=0.0005). (Fig. 1)
Figure 1 Figure 2 Figure 3 Figure 1: Comparison Of Sensory Recovery Time; Figure 2: Comparison Of Sedation Scores; Figure 3: Comparison Of Duration Of Post - Operative Analgesia (Vas >3)
Figure 2, In group C 21 patients had asedation score of 1 and 9 patients had a sedation score of 2. None of the patients in group L had sedative effects and was found to be statistically significant (p=0.002). Figure 3, Visual Analog scale (VAS) score of > 3 was reached at 192.17 ± 11.3 min. in group C and 2.53 ± 0.959 min. in group L. It was statistically significant (p=0.0005). (Fig. 3) DISCUSSION Clonidine stimulates central α2 adrenoreceptors in the dorsal horn of spinal cord5,6. However, central mechanisms of analgesia may not be applicable when clonidine is added to IVRA. Several hypothesis for this action has been proposed. Clonidine selectively depresses neuronal action potential conduction of peripheral nociceptive Aδ and C fibers5,6. It also causes localized vasoconstriction resulting in prolonged action of local anaesthetics by decreasing vascular absorption7. It causes hyperpolarization of activated cation currents as supposed to α2 receptors, are important in the peripheral analgesia of clonidine. Reuben et al8 concluded that the addition of clonidine to lignocaine during IVRA diminished torniquet discomfort and intra operative fentanyl requirement. In our study we found that adding clonidine to lignocaine during IVRA, neither prevented torniquet pain nor decreased intra operative fentanyl requirement. Kleinschmidt et al9 conducted a placebo controlled trial of clonidine 2 mcg/kg in 0.5% prilocaine IVRA which failed to demonstrate post operative analgesia. In our study we found that addition of clonidine caused an increase in the duration of post operative analgesia. Our study differs from Kleinschmidt’s in their use of prilocaine and higher dose of clonidine. In our study we used lignocaine 0.5% and clonidine at 1 mcg/kg. Hypotension was noted in Kleinschmidt’s subjects. There were no such hemodynamic side effects noted in our study as the dose of clonidine was 1 mcg/kg. Kleinschmidt et al found that the mean time to complete sensory and motor recovery was prolonged in those patients who received clonidine for IVRA in comparison with prilocaine IVRA but these results didn’t reach statistical significance. In our study we found that time for sensory recovery was prolonged and was statistically significant but motor recovery was comparable to plain lignocaine group. Ivie et al10 concluded that the addition of clonidine less than 1.5 mcg/kg as an adjunct to lignocaine in IVRA doesn’t appear to improve post operative analgesia. In our study addition of clonidine increased the duration of post operative analgesia. Lurie et al11 demonstrated that addition of clonidine 1 mcg/kg to lignocaine IVRA prolonged the onset of intolerable upper extremity torniquet pain. In our study we found that addition of clonidine did not prolong the onset of torniquet pain. Lower dose of clonidine used by Lurie et al was not assosciated with any side effects like sedation, hypotension and bradycardia. In our study, patients receiving clonidine had significant sedation scores but there were no hemodynamic side effects requiring intervention.
CONCLUSION The addition of clonidine 1 mcg/kg as an adjunct to lignocaine did not prevent torniquet pain but improved post operative analgesia when compared to plain lignocaine group.
REFERENCES
|
|
 Home
Home