Official Journals By StatPerson Publication
|
Table of Content Volume 8 Issue 1 - October 2018
Comparative study of epidural bupivacaine 0.125% and combination of epidural bupivacaine with clonidine 2µg/kg for postoperative analgesia
J Jayaganesh1*, C S Prakash2
1PG Student, 2Professor, Department of Anaesthesiology, Rajah Muthiah Medical College, Annamalai University, Chidambaram, Tamil Nadu, INDIA. Email: jaiganesh84@gmail.com
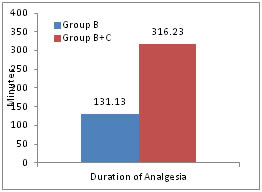
Abstract Background and Objectives: Epidural analgesia offers superior post operative pain relief compared with systemic drugs. In addition to improved pain control, epidural analgesia canimprove patient outcome by attenuating detrimental post operative stress. Clonidine, an alpha -2 receptor agonist, administered epidurally, is gaining popularity for its analgesic, sedative, sympatholytic properties. The present study was undertaken to compare and evaluate the analgesic efficacy of epidural bupivacaine and bupivacaine with clonidine. Materials and Methods: 60 patients of ASA I and II between the age group 20- 60 yrs of either sex undergoing abdominal, gynaecological and orthopedic surgeries under subarachnoid blockade were included. After the surgery was over and when the patients complained of pain or VAS > 4, they were allocated to receive either Group B - plain bupivacaine (0.125%) 10 ml (n=30), Group B + C - Clonidine 150 mcg (1ml) + 0.125% Bupivacaine 9ml (n=30). Data obtained were subjected to analysis using statistical software SPSS 20. Results: Onset of analgesia was statistically significant shorter in Group B+C than Group B (16.86±1.89 minutes vs 12.86±2.06 minutes ) with P value <0.05).Duration of analgesia was significantly longer in Group B+C than Group B (316.23±33.78 minutes vs 131.13±25.37 minutes ) with P value <0.001). 100% of patients were found asleep in Group B+C from 30min till 2.5hrs and in the Group B, no patient was found asleep. Conclusion: Epidural clonidine with bupivacaine significantly shortened the of onset of analgesia, provides good sedation, excellent and long duration of analgesia postoperatively. Key Words: Bupivaicaine, Clonidine, Epidural, Post-operative analgesia.
Effective pain control is essential for optimal care of surgical patients. Today, as then proper management of pain remains one of the most important issues of society in general and the health care professionals in particular. Analgesia not only improves the quality of life of the patients but also results in fast recovery and hence reduces the medical costs. In addition to relieving pain, epidural anesthesia and analgesia decrease the severity of perioperative physiologic derangements.1 By using lower concentrations of local anaesthetics, it provides continuous postoperative analgesia for longer duration or in combination with different agents.2 Sedation, stable hemodynamics and an ability to provide smooth and prolonged post operative analgesia are the main desirable qualities of an adjuvant in post operative epidural analgesia. α-2 adrenergic agonists have both analgesic and sedative properties when used as an adjuvant in regional anaesthesia.3-5. Alpha - 2 receptors at the spinal cord level are thought to be responsible for the analgesic properties of α2-adrenergic agonists. The analgesic requirement gets reduced to a huge extent by the use of these adjuvants because of their analgesic properties and augmentation of local anaesthetic effects as they cause hyperpolarisation of nerve tissues by altering transmembrane potential and ion conductance at locus coerulues in the brain stem.6,7 This study was designed to evaluate the analgesic efficacy of bupivacaine and clonidine mixture given through epidural route in patients undergoing elective orthopaedic, lower abdominal surgeries, comparing the sedation, quality, duration of analgesia with epidural plain bupivacaine.
MATERIALS AND METHODS This study was a prospective, randomized, double blinded controlled study conducted after approval from ethical committee and informed consent from the willing patients at Rajah Muthiah Medical College and Hospital, Chidambaram during the period April 2017- June 2018.60 patients of ASA grade I and II between the age group 20- 60 yrs of either sex, undergoing abdominal, gynaecological and orthopedic surgeries were included. Patients refusal, age <18 >60 years, ASA grade 3 and 4, ischemic heart disease, heart block, conduction defects, perioperative hypotension, neurological disorders, coagulation defects, infection at the site were excluded. Those 60 patients will be randomly allocated into two group Group B and Group B+C. Table 1: Quality of analgesia
At the end of study, the data were compiled and subjected to statistical analysis using students paired “t” test and chi square test. SPSS version 20 was used for analysis. A statistical value of p<0.05 was considered significant.
RESULTS Both the groups were comparable with respect to demographic variables (Age, Height, Weight) and ASA status did not differ significantly between groups.
Table 2: Demographic profile
Table 3: Distribution of Sex
Table 4: Type of Surgery
Table 5: ASA Status
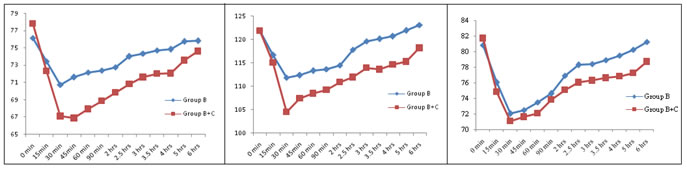
Figure 1: Comparison of heart rate Figure 2: Comparison of Systolic blood pressure Figure 3: Comparison of diastolic blood pressure
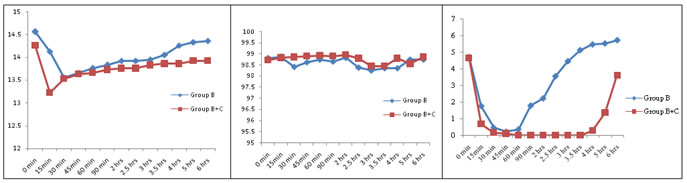
Figure 4: Comparison of Respiratory rate Figure 5: Comparison of SPO2 Figure 6: Comparison of visual analogue scale
Table 6: Comparison of Sedation Score
Table 6 shows the Sedation Score variation between two groups. The Sedation Score difference between two groups were statistically significant (p< 0.01) at 30, 45, 60, 90 mins, 2hrs, 2.5hrs, 3hrs, 3.5hrs, 4hrs in the post operative period. Table 7: Quality of analgesia (QOA)
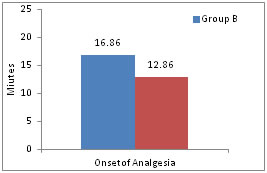 Figure 7: Comparison of Onset analgesia Table 8: Duration of analgesia
Table 9: Comparison of Side effects
As seen in table comparison of Side effects between the two groups were not statistically significant (P>0.05). DISCUSSION The incidence of postoperative pain varies with individual patients. The state of pain following a surgical procedure is a combination of pain as a specific sensation due to nociceptive response to tissue damage and pain as a suffering. Uncontrolled postoperative pain can result in several negative physiological effects that include disturbances of respiratory, cardiac, gastrointestinal, coagulation, renal, autonomic nervous system, endocrine and central nervous system function. Hemodynamics: Two patients of clonidine group (6% of group B +C) had episodes of hypotension during post operative period who were managed with a single dose of ephedrine 6 mg iv and crystalloids. In the studies conducted by Paech et al8, Senard et al 9 Eisenmach et al 10, epidural administration of clonidine caused a dose dependent reduction in haemodynamic parameters such as blood pressure and heart rate which concurs with our study. Duration of Analgesia : From our study, we showed that addition of 2μg/kg clonidine as an adjuvant to epidural bupivacaine (0.125%) not only prolongs the duration of analgesia but also provides a good sedation in the post operative period. Bupivacaine - clonidine mixture has a visible edge over plain bupivacaine as it enables an earlier onset and establishment of analgesia. This was correlated with the studies done by Antonio Mauro Vieira et.al, 11 Bonnet et al, 12 Mendez et al,13 and Armand et al 14. The level of sedation was monitored using Ramsay Sedation Scale.The patients in group B+C were well sedated and comfortable than in group B. This study correlates with the study conducted by Antonio Mauro et al15.
CONCLUSION It was concluded that epidural bupivacaine with clonidine provides a rapid, excellent and longer duration of analgesia when compared to epidural bupivacaine alone. It also significantly shortened the onset of analgesia. Longer duration of analgesia with good sedation was seen in epidural clonidine and bupivacaine group as compared with epidural bupivacaine group.
REFERENCES
|
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
 Home
Home