Official Journals By StatPerson Publication
|
Table of Content Volume 8 Issue 2 - November 2018
Amar Nath Gupta1, Ravi Anand2*, Ramanuj Singh3
1Assistant Professor, 2Senior Resident, Department of Anaesthesiology, Gouri Devi Institute of Medical Sciences, Durgapur, INDIA. 2Professor, Department of Anatomy, Gouri Devi Institute of Medical Sciences, Durgapur, INDIA. Email: drravianand75@yahoo.com
Abstract Direct laryngoscopy and endotracheal intubation result in hemodynamic changes which may lead to increased morbidity and mortality. The present interventional study was conducted to compare the effect of nebulized lignocaine with intravenous lignocaine on stress response to laryngoscopy and endotracheal intubation among the patients undergoing elective surgery under general anaesthesia. Mean pulse rate of subjects was 85.0±13.1 per minute, increased to 109.1±15.1 per min after two minutes of endotracheal intubation and was 98.8±14.9 per min at five minutes. Mean arterial blood pressure (MAP) of subjects was 94.2±7.8 mm of Hg, increased to 114.8±10.7 mm of Hg after two minutes of endotracheal intubation and was 98.7±11.7 mm of Hg at five minutes. The difference in mean arterial pressure among the three study groups was significant statistically at two minutes (p=0.00) as well as at five minutes (p=0.00). It is concluded that the hemodynamic instability after endotracheal intubation was lesser with nebulized lignocaine as compared to intravenous lignocaine. Key Word: Endotracheal intubation, Intravenous, Lignocaine, Nebulized, Stress response
INTRODUCTION One of the essential requirements of general anaesthesia is to ensure secure airway and adequate ventilation. Endotracheal intubation is the widely practiced technique to achieve the same1. However, direct laryngosopy and endotracheal intubation are associated with significant hemodynamic changes due to increased sympathetic activity. This leads to increase in BP and heart rate as well as cardiac arrythmias. This transient phenomenon is not important for healthy individuals. But, in persons with pre-existing cardiac or cerebrovascular diseases, it may lead to serious consequences2. Various drugs are used to blunt the hemodynamic response including calcium channel blockers, opioids, alpha and beta blockers and nitroglycerine3,4. Lignocaine has been used as local anaesthesia as well as given intravenously also. It is Class Ib antiarrhythmic drug and acts during the zero phase of the cardiac cells’ action potential. Intravenous lignocaine is effective in controlling the hemodynamic response to laryngeal manipulations5. On the other hand, nebulized lignocaine has been used to treat bronchial asthma6. Very few studies have been done to find the effect of nebulized lignocaine on hemodynamic response to airway manipulation and have found that its efficacy is similar to other regional techniques7,8. The present study was conducted to compare the two techniques, so that safe choices can be made available to the anaesthetist to prevent the hemodynamic complications related to airway manipulation.
AIMS AND OBJECTIVES The present study was conducted to compare the effect of nebulized lignocaine with intravenous lignocaine on stress response to laryngoscopy and endotracheal intubation.
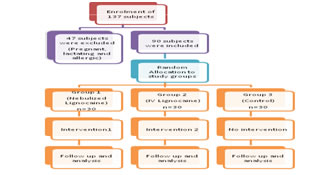
MATERIAL AND METHODS The study design of the present study was randomized clinical trial in nature conducted at Gouri Devi Institute of Medical Sciences, Durgapur. The study subjects included patients admitted in the institute and planned for elective surgery under general anaesthesia who needed endotracheal intubation. Inclusion criteria was being in the age group of 18 to 45 years, belonging to ASA grade I and II and not having underlying diseases such as diabetes, hypertension, cardiovascular disease or respiratory infection. Exclusion criteria were those allergic to lignocaine and pregnant and lactating mothers. The patients were randomly allocated to three study groups till 30 patients fulfilling the selection criteria were included in the each group in the study. Intervention: Main drugs used for induction of anaesthesia were fentanyl, midazolam, thiopentone Sodium and atracurium. After induction of anaesthesia, endotracheal tube was put in position. In the first group, the patient was nebulized with 2% lignocaine in the dose of 2 mg/kg body weight using a simple fitting face mask and nebulized for 10 min. before induction. The induction drug was injected next and endotracheal tube was put in place. In the second group, 2% lignocaine in the dose of 2 mg/kg body weight was injected intravenously and 90 seconds after that, the drugs used for induction were injected followed by placement of endotracheal tube. In the control group, lignocaine was not used. Outcome was measured in terms of hemodynamic and vital signs including systolic blood pressure, diastolic blood pressure, pulse rate and mean arterial pressure. Double blinding was used in this study in which the person measuring vital signs and the person analysing data were unaware of the study interventions. Statistical analysis was done using SPSS version 16.0 and results were reported in terms of standard statistical description. For calculation of significance, p value< 0.05 was taken into consideration. Informed consent was taken from all the participants and they were explained about the procedure and its various aspects. Confidentiality was maintained and the study subjects were free to quit from the study. Figure 1: Flow chart showing study design
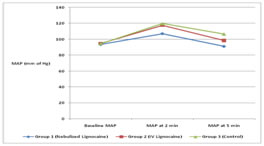
RESULTS AND DISCUSSION The present study enrolled 137 patients of which 47 were excluded. 30 patients were included in the three study groups each. Table-1 shows the baseline characteristics of study groups. Mean age of subjects was 34.4±6.1 years and difference among the three study groups was not significant (p=0.68). Mean weight of subjects was 59.7±11.4 Kgs and difference among the three study groups was not significant (p=0.51). Mean systolic blood pressure (SBP) of subjects was 124.7±11.7 mm of Hg and difference among the three study groups was not significant (p=0.59). Mean diastolic blood pressure (DBP) of subjects was 78.9±11.0 mm of Hg and difference among the three study groups was not significant (p=0.74). Mean arterial blood pressure (MAP) of subjects was 94.2±7.8 mm of Hg and difference among the three study groups was not significant (p=0.79). Mean pulse rate of subjects was 85.0±13.1 per minute and difference among the three study groups was not significant (p=0.63). Thus, it is evident that the three study groups were similar in nature. Table-2 shows the hemodynamic changes among study subjects following endotracheal intubation. Among the study subjects, mean pulse rate increased to 109.1±15.1 per min after two minutes of endotracheal intubation and was 98.8±14.9 per min at five minutes. One-way ANOVA indicated that the difference in pulse rate among the three study groups was not significant statistically at two minutes (p=0.49) and at five minutes (p=0.8). Mean arterial pressure increased to 114.8±10.7 mm of Hg after two minutes of endotracheal intubation and was 98.7±11.7 mm of Hg at five minutes. The difference in mean arterial pressure among the three study groups was significant statistically at two minutes (p=0.00) as well as at five minutes (p=0.00). Thus, it is clear that though the increase in pulse rate was similar among all the study groups, increase in MAP was higher in patients receiving lignocaine intravenously which did not differ much from the controls. However, the group receiving nebulized lignocaine showed significantly lesser increase in MAP at two minutes and this difference was also persistent at five minutes after endotracheal intubation. Agarwal et al also found that the changes in heart rate following endotracheal intubation were similar in groups receiving lignocaine in the nebulized form or intravenously. They also observed that MAP increased in response to endotracheal suctioning in both the study groups as compared to the baseline. The changes within the study groups were significant. However, the difference was not significant in between the groups. They concluded that MAP returned towards baseline with nebulized lignocaine earlier as compared to intravenous lignocaine and they promoted use of Nebulized Lignocaine over Intravenous Lignocaine8. Prasad et al studied the hemodynamic response to endotracheal suction and found that the increase in heart rate was significant among both the groups receiving nebulized and intravenous lignocaine at the end of two suctions. It normalized to the baseline at the end of four minutes in the IV lignocaine group (p<0.01) and six minutes in the nebulization group (p<0.05). They noted that there were significant differences of MAP within groups while the changes in MAP between the groups were not different significantly7. This is in contrast to the present study. Jokar et al observed that there was no significant difference between the control group and the IV lignocaine group. They also found significant MAP mean changes over time and average reduction of MAP in inhalation group was faster than intravenous lignocaine and control groups. The concluded that the administration of lignocaine through inhalation leads to a decrease in MAP and pulse rate of the patients even more rapidly than IV injection.9. Chung et al found that nebulized lignocaine and intravenous lignocaine were both effective in attenuating increase in systolic pressure to tracheal intubation but they failed to attenuate increases in diastolic pressure and heart rate10. The findings of present study are in line with those of Agrawal et al8, Jokar et al9 and Chung et al10. The hemodynamic stability is seen more with nebulized lignocaine as compared to intravenous lignocaine.
Table 1: showing baseline characteristics of study groups
Table2: showing stress response to endotracheal intubation among study groups
Figure 2: showing changes in MAP over time in the study groups
CONCLUSION The present study compared the hemodynamic response to endotracheal intubation. It is seen that the hemodynamic instability was lesser with nebulized lignocaine as compared to intravenous lignocaine. The effect on MAP was more clearly evident than pulse rate. Use of nebulized lignocaine is safe, effective and better. It is also convenient nowadays due to availability of nebulizer in higher centers.
REFERENCES
|
|
 Home
Home