Official Journals By StatPerson Publication
|
Table of Content Volume 10 Issue 2 - May 2019
A study of patient related barriers affecting effective treatment of asthma
Shreyas Ramchandra Burute1, Ruchi Doongarshi Shah2, Ramchandra B. Burute3*, Sunita Jaiprakash Ramanand4
{1Associate Professor, Department of Pharmacology} {3Associate Professor, Department of Emergency Medicine} Government Medical College, Miraj, Sangli, Maharashtra, INDIA. 2Medical Advisor, Wockhardt Pharmaceuticals, Mumbai, Maharashtra, INDIA. 4Professor and HOD, Department of Pharmacology, Government Medical College, Kolhapur, Maharashtra, INDIA. Email: shreyas.burute@gmail.com
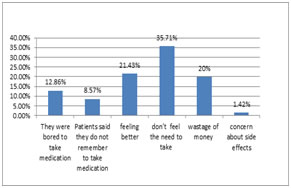
Abstract Background: Drugs play an important role in improving human health and promoting well-being. However, to produce the desired effect, they have to be safe, efficacious and have to be used rationally. Aims and Objectives: To study patient related barriers affecting effective treatment of asthma. Methodology: The study was a prospective observational study for a period of one year from February 2015-January 2016. The study was conducted at outpatient and inpatient department of medicine and paediatrics in a tertiary care hospital. Details of Age and Sex was asked and the reasons for not taking drugs were also noted. The data was entered in excel sheet and analyzed by for excel software for windows 10. Result: In our study we have seen that The average age of the Patients was 37.56±22.87 Yrs. (Range- 6-83), majority of the patients were Male -52.8% and Females were 47.2%. Among the 108 inhaled corticosteroid users; 38 patients used inhaled corticosteroid regularly and were excluded from answering this question. Out of remaining 70 patients who did not use inhaled corticosteroid regularly, 9 (12.86%) patients said that they were bored to take medication. 6 (8.57%) patients said they do not remember to take medication. 15 (21.43%) patients did not use inhaled corticosteroid as they were feeling better. 25 (35.71%) patients did not feel the need to take ICS. 14 (20%) patients said that it was wastage of money to use ICS. 1 (1.42%) patient had concern about side effects. Conclusion: It can be concluded from our study that the most common barrier found were bored to take medication, do not remember to take medication, feeling better, no need to take it, wastage of money, concern about side effects. Key Word: Barriers of treatment of asthma, Bronchial asthma(BA), Inhaled Cortico- Steroids (ICS)
INTRODUCTION Drugs play an important role in improving human health and promoting well-being. However, to produce the desired effect, they have to be safe, efficacious and have to be used rationally. Drug use is a complex subject involving the prescriber, the patient and pharmaceutical institutions. It is influenced by factors such as drug availability, prescribers' experience, health budget, promotional activities of the pharmaceutical industry, cultural factors, communication system and the complex interaction between these factors1. Drug utilization has been defined by the World Health Organization (WHO) in 1977 as “the marketing, distribution, prescription, and use of drugs in society, with special emphasis on the resulting medical, social, and economic consequences”2. The principal aim of drug utilization research is to facilitate the rational use of drugs in populations in terms of efficacy, safety and cost. Nearly 60% of patients with persistent asthma have suboptimal asthma control, a figure that has remained unchanged since 2000 in Canada and abroad3-5. Suboptimal asthma control is associated with preventable asthma symptoms, overuse of bronchodilators (i.e., rescue medication), functional impairment (e.g., work absenteeism), increased health service use (e.g., emergency visits), and even deat6,7. The goal of asthma management is to control the disease so that patients may lead a normal active life and prevent long-term impairment.8,9. Through guided self-management plans, patients learn to manage their asthma under the recommendations of their physician8,10,11. The cornerstone of asthma management in individuals with persistent asthma is the daily use of long-term controller medication for the disease, most notably, inhaled corticosteroids5. Unfortunately, adherence to recommended medications remains very low and is recognized as the main cause of therapeutic failure and preventable asthma morbidity 12,13.
METHODOLOGY The study was a prospective observational study for a period of one year from February 2015-January 2016. The study was conducted at outpatient and inpatient department of medicine and paediatrics in a tertiary care hospital. The study was approved by Institutional Ethics Committee of the Institution to which the study site is affiliated. Permission was acquired from the head of department of medicine and paediatrics for the study. Confidentiality regarding patients information was maintained. A written informed consent was obtained from patients willing to take part in the study. A written informed consent of patients of either sex above age 5 years was obtained from parents/guardians and assent was obtained from children above age 7 years. Previously diagnosed patients of bronchial asthma of varied duration who visit the hospital outpatient department of medicine and paediatrics or are admitted in the inpatient department of medicine and paediatrics. Newly diagnosed patients of bronchial asthma by physicians either clinically, radiologically or by laboratory investigations were included into the study while Patients with coexistent respiratory disorders like bronchitis or emphysema (COPD), fibrosis and any other known lung disease. Patients who were not willing to give written informed consent were excluded from the study. Details of Age and Sex was asked and the reasons for not taking drugs were also noted. The data was entered in excel sheet and analyzed by for excel software for windows 10. RESULT Table 1: Distribution of the patients as per the Age and Sex
The average age of the Patients was 37.56±22.87 Yrs. (Range- 6-83), majority of the patients were Male -52.8% and Females were 47.2%. Figure 1: Barriers of treatment Figure 1. Shows reasons for poor adherence to inhaled corticosteroids. Among the 108 inhaled corticosteroid users; 38 patients used inhaled corticosteroid regularly and were excluded from answering this question. Out of remaining 70 patients who did not use inhaled corticosteroid regularly, 9 (12.86%) patients said that they were bored to take medication. 6 (8.57%) patients said they do not remember to take medication. 15 (21.43%) patients did not use inhaled corticosteroid as they were feeling better. 25 (35.71%) patients did not feel the need to take ICS. 14 (20%) patients said that it was wastage of money to use ICS. 1 ( 1.42%) patient had concern about side effects. DISCUSSION With regard to asthma control, this encompasses adherence to treatment. Adherence enables individuals to self-manage their condition and is essential to the success of self-management interventions.14 Effective self-management has resulted in improved quality of life and reduced healthcare utilisation, days absent fr om work or school, and nocturnal asthma.15 However, despite effective medication being available, asthma is poorly controlled in over 50% of cases,16,17 and the promotion, uptake and use of self-management among people with asthma, carers of children with asthma, and healthcare professionals remain low.18–20 To maximise the benefits of self-management, barriers and facilitators to effective self-management (which may be encountered by the individual with asthma (or carer), the healthcare professional, or at the organisational level)21–23 need to be identified. Further, more effective treatment and management strategies are needed. Identification of the needs, beliefs, and behaviours of these individuals and organisational features23 can indicate where improvements should be focused to help groups of people least likely to benefit from existing self-management interventions, and potentially inform the design and implementation of future interventions.21 In our study we have seen that The average age of the Patients was 37.56±22.87 Yrs. (Range- 6-83), majority of the patients were Male -52.8% and Females were 47.2%. Among the 108 inhaled corticosteroid users; 38 patients used inhaled corticosteroid regularly and were excluded from answering this question. Out of remaining 70 patients who did not use inhaled corticosteroid regularly, 9 (12.86%) patients said that they were bored to take medication. 6 (8.57%) patients said they do not remember to take medication. 15 (21.43%) patients did not use inhaled corticosteroid as they were feeling better. 25 (35.71%) patients did not feel the need to take ICS. 14 (20%) patients said that it was wastage of money to use ICS. 1 (1.42%) patient had concern about side effects. Sandra Peláez et al 24 they found Patients were aged 2–76 years old and 58% were female. Nine patients were followed by an asthma specialist (pulmonologist or allergist), 13 patients by family doctors or pediatricians, and two patients had no regular follow-up. Barriers and facilitators to long-term daily inhaled corticosteroids were classified into the following loci of responsibility and its corresponding domains: (1) patient (cognition; motivation, attitudes and preferences; practical implementation; and parental support); (2) patient-physician interaction (communication and patient-physician relationship); and (3) health care system (resources and services). Patients recognized that several barriers and facilitators fell within their own responsibility. They also underlined the crucial impact (positive or negative) on their adherence of the quality of patient-physician interaction and health care system accessibility.
CONCLUSION It can be concluded from our study that the most common barrier found were bored to take medication, do not remember to take medication, feeling better, no need to take it, wastage of money concern about side effects.
REFERENCES
|
|
 Home
Home