Official Journals By StatPerson Publication
|
Table of Content Volume 10 Issue 3 - June 2019
Effect of addition of trimetazidine on LV function in patients with LV systolic dysfunction receiving optimal medical therapy in comparison with patients receiving only optimal medical therapy in a tertiary care centre
Shabnam Narayanan1, P N Krishna Kumar2*
{1Assistant Professor, Department of Pharmacology, Government Medical College} {2Assosciate Professor, Department of Cardiothoracic and Vascular Surgery, Government Medical College} Kannur, Pariyaram, Kerala, INDIA. Email: krishna0079@yahoo.com
Abstract Background: Left ventricular dysfunction (LVD) can lead to congestive cardiac failure. LVD was traditionally managed by antiplatelets, diuretics, antihypertensives and statins. However studies have shown that addition of Trimetazidine(TMZ) to standard treatment improve LV function and thus symptomatic improvement in patients. Many studies from western countries have shown beneficial effect of Trimetazidine in terms of LV function improvement. However not much data is available regarding the effect of Trimetazidine on LV function in Indian population. Hence this study was planned in Indian population. Objectives: To find the effect of addition of Trimetazidine on Left ventricular function, in patients with LV systolic dysfunction receiving optimal medical therapy in comparison with patients receiving only optimal medical therapy Materials and Methods: Study was conducted in Department of Cardiology, Kannur Medical College, Anjarakandy. Approval from Institutional Human Ethical Committee and Research Committee was obtained. This is a comparative study in patients with LV systolic dysfunction receiving Trimetazidine along with optimal medical therapy and patients receiving only optimal medical therapy. Study period was from November 2014 to August 2015. Results: In TMZ group, left ventricular systolic function improved significantly compared to optimal medical therapy group. In TMZ group LEVF showed an improvement of 42.56±6.59 vs 35.63±4.70 with a p value of <0.001. Conclusion: TMZ, a specific partial inhibitor of FFA oxidation, added to optimal medical therapy improved left ventricular function. Although highly suggestive, evaluation of effects of partial free fatty acid oxidation inhibition in patients with LVD requires further investigation through large scale, multicentre, randomised placebo controlled trials. Whether the observed beneficial effect of metabolic modulation in LVD, results in decreased morbidity and mortality, needs further evaluation as well. Key Word: optimal medical therapy.
INTRODUCTION Left ventricular dysfunction (LVD) refers to impaired left ventricular (LV) function. It is a complex clinical syndrome characterised by decreased myocardial contractility, hemodynamic abnormality and neuroendocrine activation. LVD can be divided into systolic and diastolic dysfunction. The former is characterized by a reduced ejection fraction and an enlarged left ventricular chamber while the latter by an increased resistance to filling with increased filling pressures.1 A reduction in the left ventricular ejection fraction (LVEF) results when myocardial contractility is decreased throughout the left ventricle. In general terms, systolic dysfunction is defined as a LVEF less than 45%.2 Left ventricular systolic dysfunction(LVSD) is one of the most common causes of heart failure3 and is an increasingly common disorder. Apart from being one of the leading causes of morbidity and mortality, it exerts a significant burden on health care expenditure with a prevalence of 1.3 to 4.6 million and an annual incidence of 0.5-1.8 million in India.4,5 LVD and subsequent heart failure represents a rapidly growing therapeutic challenge for health care providers. Approach to management of LVD is usually guided by the underlying cause. Reversible factors or revascularisation if possible is to be considered. Traditional management of LVD and heart failure has focused on modification of associated haemodynamic alterations. The optimal medical therapy includes Angiotensin Converting Enzyme inhibitors (ACEIs), Angiotensin Receptor Blockers (ARBs) when ACEIs are intolerant; β-blockers; and in selected patients, Aldosterone antagonists, Nitrates, and Diuretics along with drugs for secondary prevention of cardiovascular disease.6 However, with an imbalance between left ventricular performance and myocardial energy consumption, drugs targeted at improving hemodynamics have not yielded satisfying results. Research continues into alternative pharmacological strategies aimed at curbing the poor prognosis associated with heart failure. Recent studies have investigated the possibility of increasing cardiac performance without affecting oxygen consumption and hemodynamics by agents aimed at enhancing myocardial energy efficiency. Myocardial energy metabolism is altered in LVD, mitochondrial oxidative metabolism is reduced and glycolysis is increased with downregulation of glucose and fatty acid oxidation. Evidence suggests that in LVD, a shift of metabolism away from a preference for fatty acid towards more carbohydrate oxidation can improve contractile function, thus slowing progression and improving prognosis.7,8,9,10 Trimetazidine (TMZ) by altering the substrate preference is a promising agent in this new group of modulator drugs. TMZ is a 1-(2, 3, 4 trimethoxybenzyl) piperazine dihydrochloride salt (C12H22O3N2, 2HCl) which selectively inhibits activity of long-chain 3-ketoacyl coenzyme A thiolase, the last enzyme involved in β-oxidation. TMZ displays anti-ischemic effects without inducing any significant haemodynamic changes. TMZ has been shown to affect myocardial substrate utilization by inhibiting oxidative phosphorylation and by shifting energy production from free fatty acid (FFA) to glucose oxidation.7,8,9,10 Several studies from western countries have shown beneficial effects of TMZ in terms of LV function improvement and functional status.7,8,9,10 However not much data is available regarding the effect of TMZ on LV function in Indian population. Given the large number of patients in India, metabolic modulation could be an important tool helpful in improving the outcomes in patients with LVD. Hence this study was planned in our population.
MATERIAL AND METHODS The study was conducted in the Department of Cardiology, Kannur Medical College, Anjarakandy. Approval from Institutional Ethical Committee (IEC) was obtained before commencement of the study. This is a comparative study between patients with LV systolic dysfunction receiving TMZ along with optimal medical therapy versus patients receiving only optimal medical therapy. Study included 46 patients and period was from November 2014 to August 2015. All patients who attended Cardiology Outpatient department were screened by echocardiography for LV dysfunction (LVD). Patients with LV systolic dysfunction (LVSD) with an ejection fraction less than or equal to 45% (LVEF≤45%), who fulfilled the inclusion and exclusion criteria were taken into study. The patients were then divided into two groups. The first 46 patients with LV systolic dysfunction (LVEF ≤ 45%) were allocated into group 1 and group 2 respectively Patients in group 1(Optimal medical therapy group) were given only optimal medical therapy. Patients in group 2(TMZ group) were given TMZ 35mg BD (twice daily) (FLAVEDON MR) along with optimal medical therapy. Written informed consent was taken from all patients before initiation of study. Inclusion Criteria Patients included in the study were:
Exclusion Criteria Patients with below criteria were excluded from study:
Optimal medical therapy which includes a combination of the drugs mentioned below-
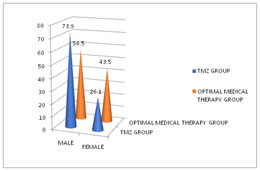
All patients were assessed for echocardio graphic parameters using echocardiography equipment (vivid S5/vivid S6 CE 0344, GE Medical system, Freiburg, Germany). Echocardiography for all the patients was done by the echo technician and confirmed by cardiologist. All patients underwent transthoracic echocardiogram according to the guidelines of the American Society of Echocardiography17, using parasternal and the apical views to calculate dimensions. Left ventricular end-diastolic and end-systolic diameters were obtained from the parasternal long axis view. A biplane algorithm was used to calculate left ventricular volume. Left ventricular end-diastolic volume (LVEDV) and Left ventricular end-systolic volumes (LVESV) were obtained from the apical four and two chamber views using the modified Simpson’s method. The ejection fraction is the ratio between stroke volume and end-diastolic volume (the normal range lying between 50% and 70%). Ejection fraction was calculated as the difference between end-diastolic volume (EDV) and end-systolic volume (ESV) normalised to end-diastolic volume (EDV) as (EDV-ESV)/EDV. All patients were followed up at 3rdand 6thmonth by transthoracic echocardiography. The data was entered in an excel sheet and was analysed using SPSS 17.0. Diagrams and graphs depicted by using Microsoft excel 2010.Continous variables were expressed as mean with standard deviation. Categorical variables summarized in terms of frequency with percentage. Continuous variables between TMZ group and optimal medical therapy group were compared by using independent sample t test. Repeated measures of ANOVA were used to compare the change in continuous variables within the groups. A p value < 0.05 is considered as statistically significant. RESULTS Figure 1: Male –female distribution pattern TMZ- TMZ This study showed a sex ratio of male 73.9 % and female 26.1 % with a mean age of 65.96±10.40 in TMZ group and ratio of males 56.5% and female 43.5% with a mean age of 61.43±12.58 in optimal medical therapy group. Table 1: Comparison of echocardiographic parameter, LVEF, done by ANOVA
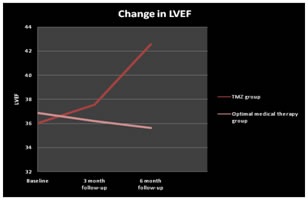
LVEF-Left ventricular ejection fraction, SD- standard deviation; TMZ -TMZ, p value < 0.05 considered statistically significant Table (1) shows the echocardiographic parameter, LVEF, in TMZ group and optimal medical therapy group. In TMZ group, LVEF shows significant improvement from baseline (36.03±6.12) to 6 months follow up (42.56±6.59) with a p value <0.001. In contrast, LVEF deteriorated in patients in optimal medical therapy group from baseline (36.87±5.001) to 6 months follow up (35.63±4.70) with a p value of 0.014
Table 2: Comparison of echocardiographic parameter, LVEF, between TMZ and Optimal Medical Therapy groups (done by independent t test)
LVEF –Left Ventricular Ejection Fraction, SD - standard deviation, TMZ –TMZ, p value < 0.05 considered statistically significant. TABLE (2) shows comparison of LVEF between TMZ and optimal medical therapy group. LVEF does not show any significant difference between TMZ group and Optimal Medical Therapy group in the baseline and 3 months follow up period. But in the 6 months follow up period there is a significant difference in LVEF values between the two groups. TMZ group shows a significant higher value (42.56±6.59) as compared to optimal medical therapy group (35.63±4.70) with a p value of < 0.001. Figure 2: Changes in LVEF TMZ –TMZ, LVEF –Left Ventricular Ejection Fraction Above graph shows improvement in LVEF in TMZ group and deterioration in optimal medical therapy group.
DISCUSSION LVD refers to altered LV function. LVD can be divided into systolic and diastolic dysfunction. The former is characterized by a reduced ejection fraction and, the latter by an increased resistance to filling with increased filling pressures. LV systolic dysfunction is characterized by a decreased ejection fraction (less than 45%).LV systolic dysfunction is the most common cause of heart failure, resulting due to mostly end-stage coronary artery disease, either with a history of myocardial infarction or with a chronically under perfused, yet viable myocardium. Metabolic modulation with shifting the energy substrate preference away from FFA metabolism and toward glucose metabolism has been shown to be an effective adjunctive treatment in patients with LVD.8 TMZ, a partial free fatty acid oxidation inhibitor, selectively inhibits activity of long-chain 3-ketoacyl coenzyme A thiolase, the last enzyme involved in β-oxidation. TMZ thus affects myocardial substrate utilization by inhibiting oxidative phosphorylation and shifts energy production from FFA to glucose oxidation. The effect of TMZ is obtained at the cellular level, by shifting the energy substrate reference from fatty acid oxidation to glucose oxidation, which is more efficient in terms of ATP production per mole of oxygen used.8 This study showed a significant improvement in LVEF in TMZ group compared to optimal medical therapy group (Table 1and2). In TMZ group, LVEF showed significant improvement from baseline to 6 months follow up whereas deterioration in patients from optimal medical therapy group from baseline to 6 months follow up. LVEF did not show any significant difference between TMZ group and Optimal Medical Therapy group in the baseline and 3 months follow up period. However, at 6 months TMZ group showed a higher LVEF compared to optimal medical therapy group. Limitations of Study
significant changes in LV function and NYHA functional class.
CONCLUSION The present study showed that shifting the energy substrate preference away from fatty acid metabolism and towards glucose metabolism by TMZ, a specific partial inhibitor of FFA oxidation, added to optimal medical therapy improved left ventricular function in patients with left ventricular systolic dysfunction. Although highly suggestive, evaluation of effects of partial free fatty acid oxidation inhibition in patients with LVD requires further investigation through large scale, multicentre, randomised placebo controlled trials. Whether the observed beneficial effect of metabolic modulation in LVD, results in decreased morbidity and mortality, needs further evaluation as well.
REFERENCES
|
|
 Home
Home