|
Table of Content Volume 10 Issue 3 - June 2019
A study of effectiveness of statins in patients of rheumatoid arthritis at tertiary health care centre
Syeda Ayesha Fatima1, Swetha G2*, Neeraj Sadiq3, Ahmed Abdul Bari Hazari4
1Assistant professor, Apollo Institute of Medical Sciences and Research Apollo Health City Campus, Jubliee Hills, Hyderabad-500096, INDIA.
2Drug safety Physician Isafety Systems, Irrum Manjil, Hyderabad, Telangana, INDIA.
3Assistant Professor, Kamineni Institute of Medical Sciences, Narketpally, INDIA.
4Assistant Professor, Department of Pharmacology, Ayaan Institute of Medical Sciences, Kanaka Mamidi Village, Moinabad, Telangana.
Email: khanashu67@gmail.com, paru.swetha@gmail.com
Abstract Background: Rheumatoid arthritis is chronic inflammatory condition involving multiple systems. Statims have anti-inflammatory properties like regulating leukocyte-endothelial cell adhesion, reducing nitric oxide (NO) production and decreasing levels of TNF-alpha, IL-1 and IL-6. Aim and objective: to study the effectiveness of statins in patients of rheumatoid arthritis. Methodology: Present study was conducted in 76 patients diagnosed as rheumatoid arthritis. Study population were divided into two groups. Group A included patients receiving DMARD therapy with statins. Group B included patients only receiving DMARD therapy. Clinical examination was done. Clinical outcome variable of RA DAS28 was noted. Patients of both groups were followed up after 6 months of initial observation. Both the clinical and biochemical variables were also noted during follow-up visits. After follow up both the groups were compared for biochemical parameters like ESR, CRP and clinical parameters. Results: In our study both the groups were comparable in age, gender, ESR, CRP and DSA28 . (p value >0.05).statistically significant difference was found in ESR, CRP, Total cholesterol , serum HD and DSA28 of both the groups(p >0.05)
Key Word: rheumatoid arthritis.
INTRODUCTION
Rheumatoid arthritis (RA) is a chronic, inflammatory arthritis associated with systemic inflammation and characterized by substantial disability and premature mortality. 1-4This increased risk of mortality is associated with more severe disease activity and is likely due in part to higher levels of systemic inflammation in patients with RA. 5-6 The disease is characterized by inflammation of synovial tissues, joint swelling, stiffness and pain, which may progress to joint and bone erosion. It leads to rapid onset of clinically significant functional impairment. Statins or 3-hydroxy-3-methylglutaryl coenzyme A (HMG CoA) inhibitors belong to the class of lipid-lowering agents that revolutionized pharmacotherapeutics of cardiovascular diseases, leading to a remarkable decline in cardiovascular death and disability in patients with or at risk of developing coronary heart disease (CHD) Many data indicate effects for statins in innate immune response, manifest on endothelial activation,7 macrophage, natural killer cells, and neutrophil effector function.8 Similar effects on acquired immune responses via suppression of antigen presentation9 and T-cell polarization have been shown in vitro and in vivo10 This study was done to see the effectiveness of statins in rheumatoid arthritis patients at tertiary health care center.
AIM AND OBJECTIVE
to study the effectiveness of statins in patients of rheumatoid arthritis.
METHODOLOGY
Present study was a prospective study carried out in a tertiary care center. Study population was patients diagnosed as rheumatoid arthritis.
Inclusion criteria:
- Patients in age group 40-70 years.
- Patients with active RA disease though having DMARD therapy. (The patients having composite 28 joints disease activity score (DAS28)11,12 of 3.2 or higher were taken as having active disease.)
Exclusion criteria
- Patients below 40 years and above 70 years
- Patients not willing to participate in the study
- Allergy to statins
- Chronic liver or renal disease Total 76 patients were enrolled in the study.
Study was approved by ethical committee. A written valid consent was taken from patients after explaining study to them. Study population were divided into two groups. Group A included patients receiving DMARD (Disease Modifying Anti Rheumatoid Drugs ) therapy with statins here in our study we gave rosuvastatin, 10 mg 1 time per day . Group B included patients only receiving DMARD therapy. Total study duration was one year. We enrolled patients in first 6 months. We followed these patients for 6months. Data was collected with pretested questionnaire. Data included sociodemographic data such as age, sex, detailed history. Clinical examination was done. Clinical outcome variable of RA DAS28 was noted. It was calculated using different variables like swollen joint count, tender joint count, patient global assessment, provider global assessment, erythrocyte sedimentation rate (ESR), C-reactive protein (CRP) ,serum hemoglobin%, total leukocyte count, serum creatinine, fasting blood sugar, total cholesterol, serum HDL (High Density Lipoprotein), serum LDL (Low Density Lipoprotein), serum glutamic oxaloacetic transaminase, and serum glutamic pyruvic transaminase. Patients continued treatment for 6 months according to their group. Patients of both groups were followed up after 6 months of initial observation. Both the clinical and biochemical variables were also noted during follow-up visits. After follow up both the groups were compared for biochemical parameters like ESR, CRP and clinical parameters. DAS28 was determined by standard formula given by the following equation:
DAS28 = 0.56 × √(t28) + 0.28 × √(sw28) + 0.70 × Ln (ESR) + 0.014 × VASSr no
Data was analysed with appropriate statistical tests.
RESULTS
Table 1: Comparison of baseline parameters in Group A and Group B
Sr. no |
Parameter |
Group A |
Group B |
P value |
1 |
Age (years) |
57.31± 2.4 |
56.32± 3.1 |
> 0.05 NS |
2 |
Weight (kg) |
61.53± 4.3 |
62.36± 2.8 |
> 0.05 NS |
4 |
ESR(mm/1sthr) |
48.13± 5.3 |
51.26± 3.4 |
> 0.05 NS |
5 |
DAS28 |
6.07±0.05 |
6.11±0.09 |
> 0.05 NS |
6 |
CRP (mg/dl) |
4.12±0.87 |
4.16±0.91 |
> 0.05 NS |
7 |
Total cholesterol (mg/dl) |
164.45± 29.22 |
161.24± 19.11 |
> 0.05 NS |
8 |
Serum HDL(mg/dl) |
41.23±8.51 |
40.61±13.2 |
> 0.05 NS |
9 |
Serum LDL (mg/dl) |
94.23±12.37 |
91.47±8.26 |
> 0.05 NS |
NS: not significant
Each group included 38 patients. In group A 18 patients were males and 20 patients were females. In Group B 12 patients were males and 24 patients were females. both the groups were comparable. Table 1 shows comparison of baseline parameters in both the groups. Mean age was 57.31± 2.4 and 56.32± 3.1in group A and Group B respectively. Mean weight was 61.53± 4.3kgs in Group A and mean weight in Group B was 62.36± 2.8 kgs. Mean ESR was 48.13± 5.3 mm/1sthr in Group A and in Group B ESR was 51.26± 3.4 mm/1st hr. Mean total cholesterol in group A and Group B were 164.45± 29.22 mg/dl and 161.24± 19.11mg/dl. Serum HDL in Group A and Group B were 41.23±8.51mg/dl and 40.61±13.2mg/dl respectively. Serum LDL in Group A and Group B were 94.23±12.37mg/dl and 91.47±8.26mg/dl respectively. both the groups were comparable with respect to parameters. (p value >0.05 not significant )
Table 2: Comparison of parameters at follow up in Group A and Group B
Sr. no |
Parameter at follow up |
Group A |
Group B |
P value |
1 |
ESR (mm/1sthr) |
29.32± 3.41 |
50.37± 4.53 |
<0.05 |
2 |
CRP(mg/L) |
2.37± 0.07 |
4.14± 0.05 |
<0.05 |
3 |
DAS28 |
3.13± 0.31 |
5.76± 0.7 |
<0.05 |
4 |
Total cholesterol (mg/dl) |
154.31± 14.76 |
160.31± 17.23 |
<0.05 |
5 |
Serum HDL(mg/dl) |
44.21±9.42 |
39.38±7.15 |
<0.05 |
6 |
Serum LDL (mg/dl) |
94.23±12.37 |
96.16±5.23 |
>0.05 |
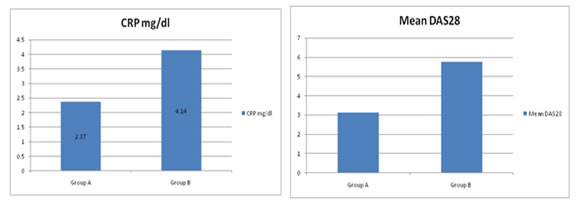
Figure 1: comparison of Mean CRP in Group A and Group B after 6 months follow up; Figure 2: comparison of Mean DAS28 in Group A and Group B after 6 months follow up
At the end of six months patients undergone investigations and DAS28 activity parameters analysis. Table 2 shows comparison of parameters at follow up of 6 months. Mean ESR was 29.32± 3.41 mm/1sthr in group A and 50.37± 4.53 mm/1sthr in Group B. the difference between these group is statistically significant(<0.05). Mean CRP in group A was 2.37± 0.07 mg/L and mean CRP in Group B was 4.14± 0.05 mg/L. there was significant change in group A in CRP. Difference between these two groups is statistically significant (<0.05). Mean DAS28 (Disease Activity Score 28) was 3.13± 0.31 in group A and mean DAS28 was 5.76± 0.7 in group B. difference between these groups was statistically significant (<0.05).Mean total cholesterol in group A and Group B were 154.31± 14.76 mg/dl and 160.31± 17.23 mg/dl. Difference between these two groups is statistically significant (<0.05) Serum HDL in Group A and Group B were 44.21±9.42mg/dl and 39.38±7.15 mg/dl respectively. . Difference between these two groups is statistically significant (<0.05) Serum LDL in Group A and Group B were 94.23±12.37mg/dl and 96.16±5.23mg/dl respectively.
DISCUSSION
In our study both the groups were comparable in age, gender, ESR, CRP and DSA28. (p value >0.05). Baseline ESR in Group A and Group B was29.32± 3.41 mm/1sthr and 50.37± 4.53 mm/1st hr. After follow up period of six months we found that Mean ESR was 29.32± 3.41 mm/1sthr in group A and 50.37± 4.53 mm/1sthr in Group B. The difference between these group is statistically significant(<0.05).similar results were seen in McCarey et al.13 Mean CRP in group A was 2.37± 0.07 mg/L and mean CRP in Group B was 4.14± 0.05 mg/L. there was significant change in group A in CRP. Difference between these two groups is statistically significant (<0.05).Both anti-inflammatory and immunomodulatory actions of statins play an important role in RA. Statins have been shown to reduce the level of CRP in patients with RA independent of their cholesterol lowering effects.14 Mean DAS28 (Disease Activity Score 28) was 3.13± 0.31 in group A and mean DAS28 was 5.76± 0.7 in group B. difference between these groups was statistically significant (<0.05).Similar results were seen in McCarey et al13where they found that significant change was observed in group receiving statins along with DMARD therapy than those receiving DMARD therapy. Statins have also been shown to decrease adhesive interaction between monocytes and vascular wall, reduce monocyte chemotaxis by interfering with monocyte chemotactic protein-1.15 Statin therapy also inhibits growth and proliferation of macrophages.16Some studies found that Statins induce apoptosis so it is beneficial in killing of inflammatory cells in RA patients17,18. One study has suggested anti-inflammatory role of statin therapy by reduction of mRNA for cyclooxygenase-219 Atorvastatin, lovastatin, and pravastatin have been shown to reduce the expression of major histocompatibility complex-II (MHC-II) on antigen presenting cells and MHC-II mediated T-cell activation.20 Statins have been suggested to reduce inflammatory cytokines production like tumor necrosis factor-α and interleukin-1β (IL-1β), chemotactic cytokines like IL-8 and IL-6.21
REFERENCES
-
Ogdie A, Haynes K, Troxel AB, et al. Risk of mortality in patients with psoriatic arthritis, rheumatoid arthritis and psoriasis: a longitudinal cohort study. Ann Rheum Dis. 2014 Jan; 73(1): 149–153.
-
Bjornadal L, Baecklund E, Yin L, et al. Decreasing mortality in patients with rheumatoid arthritis: results from a large population based cohort in Sweden, 1964–95. J Rheumatol. 2002 May; 29(5): 906–912.
-
Maradit-Kremers H, Crowson CS, Nicola PJ, et al. Increased unrecognized coronary heart disease and sudden deaths in rheumatoid arthritis: a population-based cohort study. Arthritis Rheum. 2005 Feb; 52(2):402–411.
-
Avina-Zubieta JA, Choi HK, Sadatsafavi M, et al. Risk of cardiovascular mortality in patients with rheumatoid arthritis: a meta-analysis of observational studies. Arthritis Rheum. 2008 Dec 15; 59(12):1690–1697.
-
Sattar N, McCarey DW, Capell H, et al. Explaining how "high-grade" systemic inflammation accelerates vascular risk in rheumatoid arthritis. Circulation. 2003 Dec 16; 108(24):2957–2963.
-
Wolfe F, Michaud K, Gefeller O, et al. Predicting mortality in patients with rheumatoid arthritis. Arthritis Rheum. 2003 Jun; 48(6):1530–1542.
-
Palinski W, Napoli C. Unraveling pleiotropic effects of statins on plaque rupture. ArteriosclerThrombVasc Biol. 2002; 22: 1745–50.
-
Weitz-Schmidt G, Welzenbach K, Brinkmann V, Kamata T, Kallen J, Bruns C, et al. Statins selectively inhibit leukocyte function antigen-1 by binding to a novel regulatory integrin site. Nat Med. 2001; 7: 687–92.
-
Kwak B, Mulhaupt F, Myit S, Mach F. Statins as a newly recognized type of immunomodulator. Nat Med. 2000; 6: 1399–402.
-
Leung BP, Sattar N, Crilly A, Prach M, McCarey DW, Payne H, et al. A novel anti-inflammatory role for simvastatin in inflammatory arthritis. J Immunol. 2003; 170: 1524–30.
-
van der Heijde DM, van Riel PL, van Leeuwen MA, van ’t Hof MA, van Rijswijk MH, van de Putte LB. Prognostic factors for radiographic damage and physical disability in early rheumatoid arthritis. A prospective follow-up study of 147 patients. Br J Rheumatol. 1992; 31: 519–2.
-
Prevoo ML, van ’t Hof MA, Kuper HH, van Leeuwen MA, van de Putte LB, van Riel PL. Modified disease activity scores that include twenty-eight-joint counts. Development and validation in a prospective longitudinal study of patients with rheumatoid arthritis. Arthritis Rheum. 1995;38:44–8
-
McCarey DW, McInnes IB, Madhok R, Hampson R, Scherbakov O, Ford I, et al. Trial of atorvastatin in Rheumatoid Arthritis (TARA): Double-blind, randomised placebo-controlled trial. Lancet. 2004;363:2015–21
-
Chan AW, Bhatt DL, Chew DP, Reginelli J, Schneider JP, Topol EJ, et al. Relation of inflammation and benefit of statins after percutaneous coronary interventions. Circulation. 2003; 107: 1750–6.
-
Romano M, Diomede L, Sironi M, Massimiliano L, Sottocorno M, Polentarutti N, et al. Inhibition of monocyte chemotactic protein-1 synthesis by statins. Lab Invest. 2000; 80: 1095–100.
-
Shiomi M, Ito T. Effect of cerivastatin sodium, a new inhibitor of HMG-CoA reductase, on plasma lipid levels, progression of atherosclerosis, and the lesional composition in the plaques of WHHL rabbits. Br J Pharmacol. 1999;126:961–8
-
Guijarro C, Blanco-Colio LM, Ortego M, Alonso C, Ortiz A, Plaza JJ, et al. 3-Hydroxy-3-methylglutaryl coenzyme a reductase and isoprenylation inhibitors induce apoptosis of vascular smooth muscle cells in culture. Circ Res. 1998;83:490–500
-
Rousseau JC, Zhu Y, Miossec P, Vignon E, Sandell LJ, Garnero P, et al. Serum levels of type IIA procollagen amino terminal propeptide (PIIANP) are decreased in patients with knee osteoarthritis and rheumatoid arthritis. Osteoarthritis Cartilage. 2004; 12: 440–7.
-
Inoue I, Goto S, Mizotani K, Awata T, Mastunaga T, Kawai S, et al. Lipophilic HMG-CoA reductase inhibitor has an anti-inflammatory effect: Reduction of MRNA levels for interleukin-1beta, interleukin-6, cyclooxygenase-2, and p22phox by regulation of peroxisome proliferator-activated receptor alpha (PPARalpha) in primary endothelial cells. Life Sci. 2000;67:863–76
-
Steimle V, Siegrist CA, Mottet A, Lisowska-Grospierre B, Mach B. Regulation of MHC class II expression by interferon-gamma mediated by the transactivator gene CIITA. Science. 1994;265:106–9
-
Musial J, Undas A, Gajewski P, Jankowski M, Sydor W, Szczeklik A. Anti-inflammatory effects of simvastatin in subjects with hypercholesterolemia. Int J Cardiol. 2001;77:247–53.
|
|