Official Journals By StatPerson Publication
|
Table of Content Volume 11 Issue 1 - July 2019
Perspective observational study of antibiotics in pediatric intensive care unit
R Sreedhar1*, R Aruna2
1Associate Professor, Department of Pharmacology, Kamineni Institute of Medical Sciences Narketpally – Nalganda (dist).Telangana, Andhra Pradesh, INDIA. 2Associate Professor, Department of Pathology, Chelmeda Anand Rao Institute of Medical Sciences, Karimnagar – Telangana-505001, INDIA. Email: drsreedharnr@gmail.com
Abstract Background: prescription of antibiotic to pediatric age group is a major concerns because infections are the most frequent cause of childhood disease due to less immunity as compare to adults. Method: The patients with severe illness could not be treated at OPD were admitted at PICU. The blood examination were done to confirm the diagnose and X-ray USG were also done if necessary. Antibiosis were prescribed as per the guide lines of WHOs Results- In the study of clinical manifestations 48(26.6%) had Respiratory diseases, 42(23.3%) GIT, 32(17.7%) CNS, 58(32.2%) miscellaneous diseases 5.4%. The average no. of drug per prescription was 2.6%, antibiotics per prescription, 8% were generic drugs prescription 70% fixed drug combination, 42% of injectables per prescription. Ceftriaxime was highest used antibiotics (102) while neutral machine was least used antibiotics7. Conclusion- This pragmatic observation disease in pediatric and various antiboitics essential to prevent morbidity and mortality. Key Word: PICU- pediatric Intensive care unit, antibiotics, GIT, CNS Miscellaneous, Prescription.
INTRODUCTION Pediatrics represent a higher populations worldwide. They are the most vulnerable to get infected due to less immunity. The use of antibiotics are used commonly for the treatment of pediatric illness.1 Infectious diseases are prevalent in developing countries and antibiotics prescribed for this illness. An irrational use of antibiotics may lead to an infections which are worse than the original infections.2 Hence paediatrician face number of challenges in prescribing antibiotics due to shortage of appropriate drugs. Apart from this, the development of bacterial resistance has promoted the use of antibiotics judiciously in pediatric age groups. Many studies have found that, antibiotics prescribed in viral infections and respiratory tract infections are un-necessary3 Drug utilization is defined as marketing, distribution, prescription and use of drugs in the society with emphasis on medical social and economic consequences. Proper guidelines should be implemented for use of antibiotics in pediatrics. WHO has model formulary for children but knowledge of prescribing pattern will help to formulate these types of guidelines, therefore such perspective observational prescription study will be quite useful to treat the children with various types of infections.
MATERIAL AND METHODS 180 children at different age group from 1 month to 12 years admitted at pediatric ward Kamineni Medical College Hospital Narket pally–Nalgonda (district) Telangana Inclusion criteria: The patients with different clinical manifestation like RTI, GIT, CNS, miscellaneous like scorpion bite, electric burns, snakebite, head injury. Dengue fever, malaria fever, not responding to OPD treatment were admitted at pediatric intensive care unit Exclusion criteria: patients with immune compromised, severe malnutritious, malignancies were excluded from study
METHODS The pediatric patients cannot be treated due to severity of disease were admitted at ICU. The RBE, and concerned blood test and radiological study was done to confirm the diagnose. The suitable antibiotic drugs were prescribed as per WHO guidelines
This research paper was approved by ethical committee of Kamineni medical college Narkat pally- Nalgonda (Dist) Telangana
Statistical analysis: Most of the common diagnosed were classified with percentage. Various prescribing indicators, common antibiotic received by patients were also classified with percentage. The ratio of male and females were 2:1.
OBSERVATION AND RESULTS Table-1 clinical manifestation of pediatric patients admitted at PICU – 48 (26.6%) patients with respiratory distress LRTI with Richet’s 19 Emphyma, 13-RDS with severe dehydration, 16 pneumonia 4-Respiratiory distress with cerebral palsy.
Table 1: Clinical manifestation of pediatric patients admitted (No of patients180)
-2 GIT were – 42(23.3%) 36- Acute Gastro enteritis, 6- post operative appendicitis tenderness -3 CNS 32 (17.7%),14 – Bacterial meningitis, 8-Tubercular meningitis, 6- Generalized tonic- clonic seizures, 4-sulphite oxdase deficiency with epilepsy -4 Miscellaneous 58 (32.2%) -8 scorpion bite, 9-snake bite 12- electric burns, 14 head injury 8-dengue fever 5-PUO (pyrexia of un- known origin)2-septicemia
Table-2 study of various prescription indicators 8% No of prescription with generic drugs, 2.6% No of antibiotic per prescription, 5.4% total number of drugs, 70% No of fixed drug combination, 42% no of injectables per prescription, 62% drugs from essential drug list (WHO 2018)
Table 2: Various prescribing Indicators
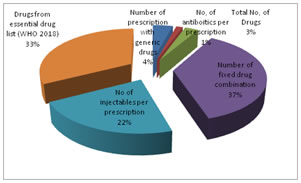
Table-3 list of antibiotics commonly used 102 ceftriaxone, 82- Amikacin, 80- Metronidiazole + oflaxacin, 60- Norfloxacin + Tinidiazole, 10-polymyxin – 9 Gentamicin, 7 Netilmicin
Table 3: List of commonly used antiboitics
DISCUSSION In the present study of perspective observation of antibiotics in pediatrics admitted at PICU. The clinical manifestation were – 48(26.6%) had Respiratory distress – 6 LRTI with rickets 9- Emphyma, 13-RDS with severe dehydration, 16-pnemonia 4- Respiratory distress with cerebral palsy (2) GIT – 42, (23.3%) – 36- acute Gastroenteritis, 6-post operative appendicitis tenderness (3) – CNS – 32(17.7%)–14 – Bacterial meningitis, 8- Tubercular meningitis, 6-Generalised tonic- clinic seizers, 4-sulphite oxidize deficiency with epilepsy. (4) – miscellaneous- 58 (32.3%) – 8 scorpion bite, 9- snake bite, 12 electric burn, 14-head injury 8-dengue fever 5-PUO.2-septicemia (Table-1) In the study of various prescribing indicators – 8% of No of prescriptions with generic drugs 2.6% No of antibiotics per prescription, 5.4% total No of drugs 70% No of fixed drug combination, 42% No of injectables per prescription. 62% drugs from essential list (WHO 2018 ) (Table-2). The list of commonly used antiboitics 102- ceftriaxame, 82- Amikacin, 80- metronidiazole + oflaxacin, 60 – Norfloxacin, Tinidiazole, 10- Polymyxine 9- Gentamicin, 7- Netrilmicin. (Table-3) These findings were more or less in agreement with previous studies.4,5,6,7 Prescribing and diagnosis in the several cases additionally, prescribing tendency of drugs reflects the clinical judgment of the clinicians. The difference in the tendency of prescribing practice may occur due to different in prevalence of disease. Larger value of antibiotics in the present study might occur due to the high for amount of infectious disease s such as upper respiratory tract infection pneumonia and empirical treatment based on sign and symptoms which itself differs between practitioner.8 It was also reported that drugs were prescribed without any information regarding the frequency of drug administration.9. This might be because of inexperience and /or professional negligence which lead to significant number of drugs prescribing without specifying the frequency ultimately cause drug resistance by bacilli. In the present study injectable route was 42% WHO recommends lesser use of injections as it is helpful in reducing the cost of treatment.10 but to tackle the severity injectable route was unavoidable. In mild or moderate infections children are comfortable with the dosage form like syrup and drops compared to the tablets and capsule. It increases compliance and helps in completing the treatment regimen. Increasing the prescription generic names drugs would promote rationale drug use and reduce the cost of drug. Moreover limited information available on drug use pattern throughout the world, indicated that drugs are not optimally used, where inappropriate use has serious health and economic consequences for individuals, and society as a whole 11
SUMMARY AND CONCLUSION In the present study of antibiotic prescription to the pediatric was not rational rather it was poly pharmacy. Overuse and inappropriate use of antibiotics without prior culture sensitivity testing demands further introspection for justification of prescription. As culture and sensitivity is a time consuming process and no patients with severe infections wait for the report of culture and sensitivity. This study warrants further microbiological, pathological, immunological study because most of the pathogenesis of infections is still un-clear
REFERENCES
|
|
 Home
Home

