A drug utilization study of oral hypoglycemic drugs and insulin in diabetic patients: Face to face with reality
Suyog S Chopade1, Rahul P Bhavsar2*, Devendra R Chaudhari3, Bapurao M Bite4
1,2Associate Professor, 3Professor, 4Assistant Professor, Department of Pharmacology, Dr. Ulhas Patil Medical College and Hospital, Jalgaon, Maharashtra, INDIA.
Abstract Background: Diabetes mellitus (DM) is defined as chronic diseases characterized by derangements in metabolism of carbohydrates, protein and fat. As per WHO, drug utilization (DU) is defined as marketing, distribution, prescription, and use of drugs in society, with special emphasis on emerging medical, social and economic consequences. Aims and objectives: To analyze the drug utilization pattern of oral hypoglycemic drugs in rural area of Jalgaon district, India using WHO drug utilization indicators, and to analyze drugs prescribed per prescription. Materials and Methods: The present study was case control, record based, observational study carried out at Medical Record Section, Dr. Ulhas Patil Medical College and Godavari hospital, Jalgaon, Maharashtra, India. Results: Out of 250 patients data analyzed, majority of the patients were in the age group 51-60 (60 patients). Maximum number of patients had DM since 5 to 10 years (75 patients). Monotherapy with OHD was given in 8 patients (3.2%), dual OHDs therapy in 150 (60%) patients, triple therapy in 31 patients (12.4%), quadruple OHDs in 4 patients (1.6%) and insulin + OHD/s therapy in 57 patients (22.8%). DDD/1000 inhabitants/day was more than DDD in case of metformin, glimepiride, sitagliptin, voglibose, and insulin. DDD/1000 inhabitants/day was less than DDD in case of glipizide, glibenclamide, pioglitazone. Conclusion: There is need to increase awareness about the use of generic drugs on a mass scale in pursuit of making optimal diabetes care available at comparatively low cost, without affecting their efficacy.
Key Words: Diabetes mellitus, WHO, drug utilization.
INTRODUCTION
Diabetes mellitus (DM) is defined as chronic diseases characterized by derangements in metabolism of carbohydrates, protein and fat. The basic pathology behind DM is either lack of insulin secretion (type 1 DM/T1DM) or inability of insulin to act on tissues (type 2 DM/T2DM).1 Globally, DM has already reached epidemic levels, which scales to nearly 382 million cases, and is projected to rise to nearly 600 million, by the year 2035.1 T2DM is the most prevalent type (90-95%) followed by T1DM (5-10%).2 It is associated with numerous complications, which are broadly categorized into macrovascular and microvascular complications. Macrovascular complications include coronary artery diseases, cerebrovascular disease, peripheral arterial disease, etc. Microvascular complications include nephropathy, neuropathy and retinopathy.3 According to report by World Health Organization (WHO) the prevalence of DM will be more than doubled from 32 million cases to 80 million cases by the year 2030.1 This can be attributed to urbanization, sedentary lifestyle, increased consumption of junk food, obesity, etc.4Conventionally, DM is managed by insulin and oral hypoglycemic drugs (OHDs), which include sulphonylureas like gliclazide, glimepiride, biguanides like metformin, alpha glucosidase inhibitors like acarbose, thiazolidinediones like pioglitazone, sodium glucose transporter-2 (SGLT-2) inhibitor) like canagliflozin, DPP-4 inhibitors like teneligliptin, sitagliptin, etc.5 As per WHO, drug utilization (DU) is defined as marketing, distribution, prescription, and use of drugs in society, with special emphasis on emerging medical, social and economic consequences.6 The main aim of DU studies is to tap the pattern of rational use of that particular drug class within the given geographical area.7 The findings of such studies help to provide ground reality to enable chalking out of effective, optimal and feasible health care strategies in pursuit of harmonizing society, health, and medicine.8In the past 2 decades, numerous OHDs and their combinations have been approved for the management of T2DM.9 Patients with DM suffer from co-morbidities like hypertension, dyslipidemia, or complications of DM like coronary artery disease, cerebrovascular disease, etc.10 This warrants prescription of numerous medications to combat the main disease and its complications/comorbidities. Thus, it will not be surprising to a sound mind that irrational combinations are common finding in such studies.9 This leads to dual attack on quality of life of diabetic patients-firstly, due to adverse effects arising due to use of multiple drugs and irrational combinations and secondly, due to increased cost burden of therapy.11Keeping these things in mind, the present study was planned to analyze the drug utilization pattern of antidiabetic drugs in rural areas of Jalgaon district, India.
MATERIALS AND METHODS
The present study was case control, record based, observational study carried out at Medical Record Section, Dr. Ulhas Patil Medical College and Godavari hospital, Jalgaon, Maharashtra, India. The present study was carried out for 6 months from January 208 to June 2018. After screening 278 patient records, 250 were finally included for analysis. Records of patients diagnosed with T2DM, irrespective of age and sex were included in the study. All the required information like socio-demographic details, medications according to drug class, average number of drugs per prescription, number of drugs prescribed as generics, etc. was captured into predesigned information sheet. Each drug was classified into ATC (anatomical and therapeutic classification) codes, as laid down by WHO wherein the drugs are classified according to their chemical, pharmacological and therapeutic properties. DDD (defined daily dose) per 1000 inhabitants per day is usually employed to obtain a fair projection of prevalence of drug use in a particular set of population or prevalence of chronic disease where drug is being used for a specific indication [15]. It was calculated by the formula:12
RESULTS
DDD/1000 inhabitants/day = Units prescribed x dosage unit x 1000 DDD
DDD x duration of study x total sample size
The present study was initiated after obtaining Institutional Ethics Committee (IEC) approval. The data was analyzed using Microsoft Excel 2013. Flow of the study is shown in figure 1.
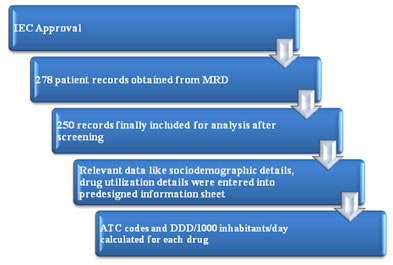
Figure 1: showing methodology of the present study.
52 (21%) patients in >60 years age group, 48 (19.2%) patients in age group 41-50 and least in age group <20 years. The present study comprised of 131 (52.4%) males and 119 (47.6%) females. Average number of drugs per prescription was 2.32, average cost per prescription was 131.23/-, while 78 (31.2%) OHDs were prescribed as generics. [table 1]
Table 1 :General details of the patients |
|
Sr. No. |
Item/s |
|
n (%) |
1 |
Age |
<20 |
16(6.4%) |
21-30 |
35(14) |
31-40 |
39(15.6) |
41-50 |
48(19.2) |
51-60 |
60(24) |
>60 |
52(21) |
2 |
Sex |
Male |
131(52.4) |
Female |
119(47.6) |
3 |
Average no. of drug/prescription |
|
2.32 |
4 |
Average cost/prescription |
|
131.23 /- |
5 |
% of drugs prescribed as generics |
|
78(31.2%) |
Table 1: showing general details of patients.
On analyzing number of patients and duration of DM, it was found that maximum number of patients had DM since 5 to 10 years (75 patients), followed by 55 patients in 11-15 years duration, 51 patients in <5 years duration, and 28 patients with DM for >20 years [figure 2].
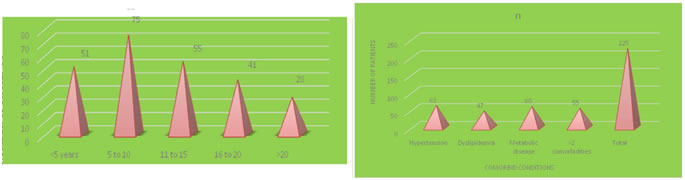
Figure 2: showing number of diabetic patients and duration of DM Figure 3: showing comorbidities in the present study
On analyzing the co-morbid conditions, it was found that 225 patients (90%) were having comorbidities. Out of which, hypertension was most common (63 patients) followed by metabolic disorders (60 patients), >2 comorbidities in 55 patients and dyslipidemia in 47 patients. [figure 3]
Monotherapy with OHD was given in 8 patients (3.2%), dual OHDs therapy in 150 (60%) patients, triple therapy in 31 patients (12.4%), quadruple OHDs in 4 patients (1.6%) and insulin + OHD/s therapy in 57 patients (22.8%) [table 2].
Table 2:Combination therapy in present study |
Sr. No. |
Therapy |
n(%) |
1 |
Monotherapy |
8(3.2%) |
2 |
Dual |
150 (60) |
3 |
Triple |
31 (12.4) |
4 |
Quadruple |
4 (1.6) |
5 |
Insulin + OHD |
57 (22.8) |
Table 2: showing drug regimens used for treatment of DM.
Biguanides were most commonly prescribed class of OHD in 103 patients, followed by thiazolidinedione in 94 patients, sulphonylureas in 89 patients, DPP-4 inhibitors in 39 patients, insulin in 21 patients and SLGT-2 inhibitors in 10 patients [table 3].
Table 3: showing medications prescribed according to drug class.
Sr. No. |
Class of drugs |
n |
1 |
SU |
89 |
2 |
Biguanide |
103 |
3 |
Thiazolidinedione |
94 |
4 |
DPP-4 inhibitor |
39 |
5 |
SGLT-2 inhibitor |
10 |
6 |
Insulin |
21 |
Table 3: showing medications prescribed according to drug class.
The ATC codes and DDD/1000 inhabitants/day is shown in table 4. DDD/1000 inhabitants/day was more than DDD in case of metformin, glimepiride, sitagliptin, voglibose, and insulin. DDD/1000 inhabitants/day was less than DDD in case of glipizide, glibenclamide, pioglitazone.
Table 4: showing ATC/DDD of OHDs and insulin in the present study.
Sr. No. |
Drug |
ATC code |
DDD (in mg) |
DDD/1000 inhabitants/day |
1 |
Metformin |
A10BA02 |
2000 |
18.9 |
2 |
Glimepiride |
A10BB12 |
2 |
8.2 |
3 |
Glipizide |
A10BB07 |
10 |
5.4 |
4 |
Glibenclamide |
A10BB01 |
10 |
8.64 |
5 |
Pioglitazone |
A10BG03 |
30 |
5.23 |
6 |
Teneligliptin |
NA |
NA |
NA |
7 |
Sitagliptin |
A10BH01 |
0.1 |
3.4 |
8 |
Voglibose |
A10BF03 |
0.6 |
4.72 |
9 |
Insulin |
A10AB01 |
40 |
52.1 |
Table 4: showing ATC/DDD of OHDs and insulin in the present study.
DISCUSSION
The present study showed slight male predilection towards the disease. This is in conjunction with findings of other such studies.3,13 However, Agrawal et al reported male: female ratio of 3:1 which is way higher.12 Most probable reason for male preponderance might be the fact that women’s health is still neglected in most parts of the country and therefore, it is less likely that a women will visit healthcare facility under such circumstances. The average number of drugs per prescription in the present study was less than that found in other studies, wherein average number of drugs per prescription was reported around 4.14 This is a welcome sign, since it is known that major issue with optimal outcomes in diabetic patients is poor patient adherence to these drugs. It has been found in one study that adherence of patients to antidiabetic drugs was as less as 60%.11 Reasons for such low adherence were reported as multiple medications/ prescription, increased cost of therapy, adverse effects arising due to these multiple medications.11 31% of total OHDs were prescribed as generic drugs in the present study, which is far higher than that of other studies, which reported only 4.5% and 22% OHDs reported as generics.3,15 Generic drugs are bioequivalent to innovator drug, plus they have added advantage of having less price. Hence, it is quite logical that more the use of generic drugs, better healthcare can be made available to mass population in an economically constrained country like India.16 Hypertension and metabolic disease were the most common co-morbidities in the present study. This is in corroboration with findings of other studies conducted in other parts of the country.17,18 Dual therapy was most commonly used in the present study. Similar findings were observed in one clinical study.19 Mostly, dual therapy involves a combination of insulin secretogogue and insulin sensitizer, and metformin + sulphonlyurea is most commonly used dual therapy combination in diabetic patients.20 These studies report the use of such combination in as much as 60% of the patients, which is in conjunction with the findings of the present study. Metformin helps to prevent weight gain and has shown to attenuate effect of cardiovascular risk factors, and hence metformin is used as first line drug in the treatment of T2DM in majority of the cases, unless contraindicated.21 In the present study, metformin was most commonly prescribed OHD and the above cited facts might have played a crucial role for such finding. Drug consumption in the present study was analyzed in the present study by DDD (defined daily dose) concept to permeate the shortcomings of traditional techniques.22 DDD provides a fair projection of average drug consumption for its use in main indication in adults.22 Highest DDD/1000 inhabitants/ day was found in regular insulin and amongst the OHDs, metformin was having maximum DDD/1000 inhabitants/day. This indicates that metformin was most commonly prescribed OHD, and glimepiride along with glibenclamide were most commonly prescribed sulphonylureas. These findings are in corroboration with that of other studies.7,23
CONCLUSION
Metformin was most commonly used drug in OHDs. Dual therapy was most commonly prescribed, which indicates attempts to achieve stringent glycemic control. There is need to increase awareness about the use of generic drugs on a mass scale in pursuit of making optimal diabetes care available at comparatively low cost, without affecting their efficacy.
REFERENCES
- IDF Diabetes Atlas. 6th ed. International Diabetes Federation, 2013. Available from: http://www.idf.org. Accessed on 10 May 2018.
- Bope E, Kellerman R. Conn’s Current Therapy 2014. Saunders-Elsevier, Philadelphia, United States of America; 2014;701-704.
- Naidu C, Vardhan A, Bankar M, et al. A drug utilization study of antihyperglycaemic agents in a rural tertiary care hospital. Int J Med and Dent Sci 2017;6(1):1357-1361.
- Wild S, Bchir M, Roglic G. Global Prevalence of Diabetes estimates for the year 2000 and projections for 2030. DIABETES CARE 2004;27(5):1-11.
- Matthaei S, Bierwirth R, Fritsche A, et al. Medical Antihyperglycaemic Treatment of Type 2 Diabetes Mellitus: Update of the evidence-based guideline of the German Diabetes Association. Exp Clin Endocrinol Diabetes 2009; 117: 522 – 557.
- Lee D, Bergman U. Studies of drug utilization. In: Strom BL, editor. Pharmacoepidemiology. 4 ed. New York: John Wiley and Sons; 2005.p. 401.
- Adibe M, Aguwa C, Ukwe C, et al. Outpatient Utilization of anti-diabetic drugs in the South Eastern Nigeria; Int J.Drug Dev. and Res. 2009; 1(1):27-32.
- Bakssas I, Lunde P. National drug policies: the need for drug utilization studies. Trends Pharmacol Soc 1986; 7:331.
- Das B, Sethi A, Rauniar G, et al. Antimicrobial utilization pattern in outpatient services of ENT department of tertiary care hospital of Eastern Nepal. Kathmandu Univ Med J 2005;3(12):370-5.
- Triplitt C, Reasner C, Isley L; Diabetes mellitus.; In: Dipiro J, Talbert R, Yee G, Matzke G, et al, editors. Pharmacotherapy: a pathological approach. 6thed. New York: McGraw-Hill Inc 2005:1333.
- Perwitasari D, Urbayatun S. Treatment adherence and quality of life in diabetes mellitus patients in Indonesia. Sage Open 2016:1-7.
- Agrawal R, Rath B, Saha K, Mohapatra S. Drug utilization pattern of antidiabetic agents in a tertiary care hospital of western Odisha, India. Int J Basic Clin Pharmacol 2016;5:2222-6.
- Vengurlekar S, Shukhla P, Patidar P, et al. Prescribing pattern of anti-diabetic drugs in Indore city hospital. Indian J Pharm Sci 2008;70:637-40.
- Nuthakki S, Pendyala S, Vallabhu C, et al. An Assessment of Anti-hyperglycemic Drug Utilization Patterns and Adherence to AACE/ACE 2015 Guidelines in South Indian Tertiary Care Teaching Hospital. Indian Journal of Pharmacy Practice 2016;9(4):226-230.
- Abidi A, Rizvi D, Ahmad A. Pharmacoeconomic and drug utilization study of antidiabetic therapy in a tertiary care teaching hospital of northern India. Asian J Pharm Clin Res 2016; 9(3):371-375.
- Bera A, Mukherjee A. The importance of generic drugs in India. IJPCBS 2012; 2(4):575-587.
- Alti A, Latha S, Nagarjun G, et al. A Study on Drug Utilization Pattern and Effectiveness of Oral Hypoglycemic Agents in Diabetes Mellitus. PharmaTutor 2015; 3(7); 31-37.
- Ramachandran G, Rohith V, Isabella T. Evaluation of prescribing pattern of anti-diabetic drugs using WHO prescribing indicators in a tertiary care hospital in Puducherry: A cross-sectional study. The Pharma Innovation Journal 2015; 4(5): 76-80.
- Kannan A, Kumar S. A study on drug utilization of oral hypoglycemic agents in type-2 diabetic patients. Asian J Pharm Clin Res, Vol 4, Issue 4, 2011, 60-64.
- Hermann L, Schersten B, Bitzen P, et al. Therapeutics comparison of metformin and sulphonylurea alone and in combinations. A double blind controlled study. Diabetes Care 1994;17:1100-9.
- Krentz A, Bailey C. Oral antidiabetic agents: current role in type 2 diabetes mellitus. Drugs 2005;65(3):385–411.
- WHO collaborating centre for drug statistics methodology. ATC index with DDDs. Oslo: WHO Collaborating Centre for Drug Statistics Methodology; 2002.
- Petel B, Oza B, Patel K, et al. Pattern Of Anti Diabetic Drug Use In Type 2 Diabetic Patients In A Medicine Outpatient Clinic Of A Tertiary Care Teaching Hospital. Int Journal of Basic and Clinical Pharmacology; 2013;2(4); 485-491.