Official Journals By StatPerson Publication
|
Table of Content Volume 12 Issue 1 - October 2019
B S Abhishakth Gerhardt1, Bhuvaneshwari2*, Sravani Marpaka3
1Post Graduate ,2Associate Professor, Department of Pharmacology, Osmania Medical College, Telangana, INDIA. 3Patient Safety Pharmacovigilance Associate, PvPI, AMC-Osmania Medical College, Telangana, INDIA. Email:bhuvana2005@gmail.com
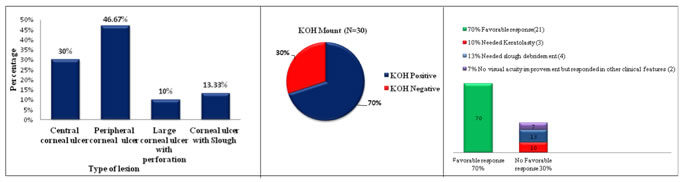
Abstract Background: Fungal corneal ulcer is a suppurative and ulcerative infection of cornea which can lead to loss of vision if left untreated. Though it has an insidious onset, it can elicit severe inflammatory response which may result in corneal perforation and thus affects vision adversely. Foreign body and traumatic injury by vegetable matter in agricultural fields are the potential risk factors in developing countries like India. This study is aimed to evaluate the effectiveness of topical 5% Natamycin in the treatment of fungal corneal ulcer. Methods: 30 randomly selected patients with clinically diagnosed fungal corneal ulcer were included in the study. KOH mount is used for early detection of fungal elements. 5% Natamycin, the test drug was prescribed to all 30 patients. The baseline factors evaluated to assess the response to treatment were best spectacle-corrected visual acuity (BSCVA) at 3 months as primary outcome and clinical progression and safety of medication as secondary outcomes. Results: Out of 30 patients 14 had peripheral corneal ulcer, 9 had central corneal ulcer, 4 had corneal ulcer with slough and 3 had large corneal ulcer with perforation. 70% (21 out of 30) of patients responded favorably to treatment with Natamycin and visual acuity improved with a statistical significance of p=0.0021. In 77% (23 out of 30) of patients ulcer margin receded, size of hypopyon reduced and satellite lesions reduced. None of the patients developed adverse drug reactions. Conclusion: With an early medical intervention using topical 5% Natamycin, ocular morbidity and blindness can be effectively prevented especially in early and less severe stages. Keywords: fungal corneal ulcer, keratitis, KOH mount, keratoplasty, Natamycin
INTRODUCTION Fungal corneal ulcer is a suppurative and ulcerative infection of cornea which can lead to loss of vision if left untreated1. It is one of the leading causes of blindness in corneal diseases which is relatively more common in tropical and developing countries. Fungal corneal ulcer though has an insidious onset, it can elicit severe inflammatory response which may result in corneal perforation and thus affects vision adversely2. Course of fungal keratitis can be more virulent and damaging than bacterial keratitis3. In developed countries like United States, wearing contact lens is the presumed risk factor, where as in developing countries like India and Thailand it is mainly attributed to ocular trauma. In these developing countries 40% of microbial keratitis accounts for fungal keratitis3. Fillamentous fungi like Fusarium and Aspergillus species are common causative fungi in tropical and subtropical countries, while in temperate countries it is mainly by Candida species4.Fungal corneal ulcer is still a diagnostic challenge and a difficult therapeutic problem because it frequently results in corneal melting, visual impairment and serious ocular damage if it is not diagnosed early and treated effectively. The first line treatment of fungal corneal ulcer is topical application of antifungal agents. Natamycin an antifungal agent, is available as 5% topical ophthalmic preparation 5. It is regarded as the most important agent in the treatment of fungal corneal ulcer. Chemically, it is a tetraene polyene 6.As it is effective against filamentous fungi it is usually considered as the first choice of drug against it 7. As fungal corneal ulcer is common in Indian sub-continent and as it has enormous ocular complications, here comes the importance of study on treatment for fungal corneal ulcer in a tertiary care hospital in the state of Telangana. This study is aimed to evaluate the effectiveness of topical 5% Natamycin in the treatment of fungal corneal ulcer.
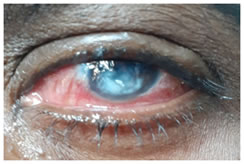
MATERIAL AND METHODS The study was conducted in outpatient department of Ophthalmology in Sarojini Devi Eye hospital, Hyderabad for a duration of 6 months from December 2018 to May 2019.It is a hospital based prospective study (quasi experimental design). After obtaining informed written consent, 30 patients (18 males and 12 females) with clinically diagnosed fungal corneal ulcer were included in the study. Patients presented with symptoms like pain which was gradual in onset, blurring of vision, gritty sensation, photophobia and watery or mucopurulent discharge. On examination corneal opacity and discharge from eye were noted as represented in figure-1. The patients with mixed infections of bacteria and fungi were excluded from the study. After obtaining a proper history regarding the events leading to ulcer, a complete ocular examination was done. This included slitlamp examination, fluorescein staining of cornea and syringing to check for the patency of nasolacrimal duct.
Table 1: Distribution of patients according to their sex (N=30)
Table 2: Distribution of patients according to their age (N=30)
The visual acuity was recorded in all cases and fundus evaluation done wherever possible. Under topical 4% lignocaine anaesthesia, scrapings of corneal ulcer were collected by direct visualization using slitlamp. Multiple scrapings were processed for Potassium hydroxide (KOH) mount preparation.21 out of 30 were potassium hydroxide (KOH) mount smear positive and remaining 9 patients were clinically diagnosed cases. All the study patients were prescribed topical 5% Natamycin eye drops. The drops were administered hourly and examination of the eye was done for every two days till the ulcer started to improve. Then the dosage was reduced to once in three hourly and continued for 2 weeks after healing of ulcer8.The baseline factors evaluated to assess the response to treatment were best spectacle-corrected visual acuity (BSCVA) at 3 months as primary outcome and clinical progression and safety of medication as secondary outcomes. Patients were examined daily in the first week and then weekly thereafter for 12 weeks.
OBSERVATIONS AND RESULTS After clinical evaluation the corneal lesions observed was as follows. Out of 30 patients 14 had peripheral corneal ulcer, 9 had central corneal ulcer, 4 had corneal ulcer with slough and 3 had large corneal ulcer with perforation as shown in Graph-1. From the investigational diagnosis 70% of cases showed positive results for KOH mount as represented in Graph-2. Test drug topical 5% Natamycin results on visual acuity are as follows. Graph 1 Graph 2 Graph 3 Graph 1: Distribution of study participants according to type of lesions (N=30) Graph 2: Distribution of study participants according to their KOH mount result (N=30) Graph 3: Visual acuity response to topical 5% Natamycin Table 3: Comparison between pre and post treatment with 5% Natamycin mean visual acuity
The graph-3 and table-4 depicts that 21 patients (70%) out of 30 responded favorably to Natamycin as primary treatment in terms of visual acuity. On statistical analysis p value is found to be 0.0021 which is significant. Out of 9 patients with central corneal ulcer, for 3 patients visual acuity has improved from 3 meters to 6/60 and in 4 patients it is improved from 5 meters to 6/36 .Remaining 2 patients did not respond in terms of visual acuity but they responded in other clinical features. 14 with peripheral corneal ulcer responded favorably to topical Natamycin and visual acuity has improved from 6/60 to 6/24 in 7 patients, 6/36 to 6/18 in 4 patients and 6/60 to 6/18 in 3 patients. 3 patients who had large corneal ulcer with perforation and melting did not respond to Natamycin, were taken for keratoplasty. In 4 patients debridement for slough was done and then they were started with 5% Natamycin. They had a favorable response. In 23 out of 30 patients ulcer margin receded, size of hypopyon reduced and satellite lesions reduced. There were no adverse drug reactions observed and reported by patients during the indexed period of the study.
DISCUSSION In our study male predominance (60%) is observed. Majority of patients are from rural areas. By occupation most of them are farmers and few are house wives. Majority had history of trauma or foreign body like vegetable matter that was encountered at work place. Patients presented with history of insidious onset of symptoms which were gradual in progression. A complete ocular examination and clinical evaluation was done for clinical diagnosis. A simpler and rapid diagnostic test, KOH mount was used as a screening test for fungal elements detection. KOH mount showed positive result in 70% of study population. Though culture results may play a vital role to initiate medical therapy in infectious diseases, fungi grow slower than other pathogens9. Here comes the need for proper history, clinical examination, screening tests like KOH smear and confocalmicroscopy which shows fungal elements at a faster rate10. Based on the above observations we started the anti-fungal treatment as it will be too late if we wait for the culture results. There are three main classes of antifungal agents that are used for treatment of fungal corneal ulcer which are polyenes, triazoles and echinocandins. Our study drug Natamycin, an antifungal agent is chemically a tetraene polyene. Its mechanism of action is by blocking fungal growth by binding specifically to ergosterol which is an essential component in fungal cell wall11.As it has low ocular retention, frequent administration of is advised12. On topical application Natamycin enters only into corneal stroma but not into ocular fluid13. Hence it is primarily useful in patients with superficial ocular infection. Conventional route of administration of antifungal agents in fungal corneal ulcer is in the form of eye drops. Systematic use of the agents possesses serious side effects. Other routes include oral, intravenous, ointment, subconjunctival and corneal stromal injection. With Natamycin intravenous and subconjunctival injections it’s difficult to achieve therapeutic levels and it poorly penetrates into the aqueous6. Natamycin has broad antifungal spectrum against filamentous fungi especially Fusarium species12. In our study we considered visual acuity as the primary outcome in respect to effectiveness of Natamycin. The data was statistically evaluated with IBM SPSS statistics for Windows, Version 22.0. When we compare mean visual acuity before and after Natamycin treatment it is observed that Natamycin showed favorable response in 70% (21 out of 30) of patients with an improved visual acuity with a p=0.0021, which implies it’s statistically significant. In peripheral corneal ulcer patients Natamycin showed favorable response with p= <0.001 and in central corneal ulcer patients showed favorable response with p= 0.001 which also implies its statistical significance. Due to the means of the visual acuity and the direction of t-value, we can conclude that there was a statistically14 significant improvement in visual acuity following the drug. Another study by Sharma et.al. also stated significant improvement in visual acuity (p=0.005) with Natamycin in patients with Fusarium keratitis and 89.2% patients showed ulcer healing15. We consider the progression of ulcer and drug safety as secondary outcome. In 77% (23 out of 30) of patients ulcer margin receded, size of hypopyon reduced and satellite lesions reduced. None of the patients developed adverse drug reactions during the indexed period. From the above analysis we can conclude that pharmacotherapy with topical 5% Natamycin is effective both clinically and statistically. Consider central and peripheral corneal ulcers as non severe keratitis (23 out of 30) and large corneal ulcer with perforation and ulcer with slough as severe keratitis(7 out of 30). Among non-severe keratitis 91% (21 among 23) showed improvement in vision with best spectacle-corrected visual acuity. This tells high the efficacy of Natamycin in early and less severe cases. A study done by Kalavathy et.al. also stated 72% (36 of 50) patients showed a favorable response to primary Natamycin therapy among them 28 out of 37 are non severe keratitis, 8 out of 13 are with severe keratitis16. There are also comparative studies of Natamycin with voriconazole. In a study by Venkatesh Pragna et al states significantly better clinical and microbiological outcomes with Natamycin than voriconazole treatment for smear-positive filamentous fungal keratitis17.The efficacy of Natamycin is attributed to its broad spectrum of antifungal activity and safety profile. The primary effect of 5% Natamycin in the management of fungal corneal ulcer is prevention of disease progression that may lead to vision loss or blindness and morbidity of eye. The vision improvement attained as Best spectacular corrected visual acuity may be achieved around 3 months post treatment. Generally side effects of Natamycin are rare, but there may be allergic reactions like ocular irritation 13.This study brings out the requirement of the patient to seek medical attention as early as possible .We are also emphasizing the importance of creating awareness among the general population regarding need for taking precautionary measures for avoiding foreign body or trauma to the eye.
CONCLUSION An early medical intervention with topical 5% Natamycin can prevent ocular morbidity and blindness to a great extent. Clinical findings and rapid diagnostic tests like KOH smear are helpful in early detection for timely management of disease. 5% topical Natamycin is a preferable choice as a primary first line management in superficial fungal ocular infection. More rapid, sensitive and specific diagnostic tests for the detection of fungal corneal ulcer, study of more topical ophthalmic antifungal agents and comparative studies are always helpful for better management.
ACKNOWLEDGMENT We are thankful to Dr.M.Padma , Associate Professor, Sarojini Devi Eye Hospital, for helping us to conduct the study in this institution. We also thank the patients of Sarojini Devi Eye Hospital, for their cooperation.
REFERENCES
|
|
 Home
Home