|
Table of Content - Volume 13 Issue 2 - February 2020
Pattern of sleep quality and depression, stress and anxiety in medical students: A cross-sectional comparison study over spans of medical years
Jayna Devalia1*, Dipika Baria2, Jatin Chhaya3, Tosha Thakor4, Harsh Thesia5, Shailly Tiwari6, Viral Patel7, Krushang Jadav8, Alok Shah9
{1,2Assistant Professor, Department of Physiology} {3Assistant Professor, Department of Community Medicine,} 4,5,6,7,8,9,Medical Students, Smt. B. K. Shah Medical Institute and Research Centre, Sumandeep Vidyapeeth. Email: dipsy984@gmail.com
Abstract Background: Medical course consider among the toughest course, which demand hard work, dedication, strong efforts, devotion and passion from the enrolled students. Many times, inability to cope stressful situation during the course affects the mental dimension of complete health and results in negative emotions of mental health – depression, anxiety and stress. Poor sleep quality is believed to deteriorate psychosocial comfort. Methods: This observational study was conducted as a part of “EviGenCHiP program” of private medical college and tertiary care hospital of Vadodara. The tool utilized in this study was Depression, Anxiety, and Stress Scale (DASS-21) and the Pittsburgh Sleep Quality Index (PSQI) used to know the subjective quality of sleep. Results: Overall, 8 % of the students suffered from moderate to extremely severe depression, 10% of the students suffered from moderate to extremely severe anxiety, and 12% students had moderate to extremely severe stress. Poor sleep quality was found more in female students as compared to counter male part. Conclusion: Though the less compared to other study but, depression, anxiety, stress and poor sleep quality among medical students is the emerging public health problem. Appropriate actions to reduce depress, anxiety and stress and improve sleep quality, include mentorship program, students support program, students engage in extracurricular activities to revitalize them and to include students friendly education and evaluation process. Key Word: sleep quality, stress, anxiety.
INTRODUCTION Despondency, feeling nervous, having a non-interest in all the routine activities - these are symptoms familiar to all of us. But, if they continue and affect our life significantly, it may be depression.1 It along with anxiety and stress are the leading cause of ill health and disability worldwide. More than 22% of total population are living with depression worldwide; as per World Health Organization (WHO).2 This kind of mental illness found to be more common amongst the medical students without preponderance between males and females. It can be due to various reasons, as instance, long and tough syllabus, hardest exam, and long hours of classes all that need attentive mind-set.3,4 Exceedingly difficult question paper of Medical Colleges sorts it one of the toughest examinations to clear in India.5 Inability to cope kind of expected situation, sometimes medical students succumb to poor quality of sleep and depression, anxiety and Stress. They may yell all of the time, avoid classes, or isolate themselves without recognizing they are depressed or stressed and are often accompanying with poor academic performance and poor quality of life as well. Preceding studies stated that depression in university students is noted worldwide and the prevalence looks to be increasing.6,7 Natural phenomena, magnitude of mental health condition and associated factors of decrease sleep quality, depression, stress and anxiety is essential to report for effective public health planning and interventions towards medical students. However, scarcity of research was found in concern to depression, anxiety and stress and their contributing factors of poor sleep quality among medical students, particularly in low and middle-income countries including India. Therefore, current study aimed to document the prevalence of depression, anxiety and stress among medical students; along with association of contributing factors for poor sleep quality.
OBJECTIVE
METHODOLOGY Study design: this was a Cross-sectional study. Study participants, Sample Size and Study Period: This study included Medical students of Second to Third Final years of Medical course of Smt. B. K. Shah Medical Institute and Research Centre, Sumandeep Vidyapeeth (Dist: Vadodara, State: Gujarat). The entire study was conducted between the months of July 2019 to October 2019. The Medical course is spread over a span of five and half years which include pre-clinical, para-clinical and internship of 1 year. We exclude first year students from the study as it is period that serves as buffer to orient new undergraduates to the course. Ethical Approval: This study was approved by Sumandeep Vidyapeeth Institutional Ethical Committee (SVIEC) of Sumandeep Vidyapeeth. The permission to conduct study was also taken from the Dean of Smt. B. K. Shah Medical Institute and Research Centre, Sumandeep Vidyapeeth Study Inclusion and Exclusion Criteria:
Study tool: The self-report questionnaire utilized which took approximately 30 minutes to answer and collected data on:
Study Procedure: Data collection took place after a didactic lecture sessions. The investigator introduces and explained the significance of the study, and asked the students to fill out complete questionnaire along with signed the attached consent form. Students also assured about confidentiality of information provided by them. Students were asked to fill related details in the validated questionnaire, of past 10 days. Those students, who remained absent on the day of data collection, also approached on next day to fill the questionnaire reduce left outs. Statistical analysis: The data were entered in the Microsoft Excel and analysed with the help of the software named “Statistical Package for the Social Sciences (SPSS)” version 17.0. Socio-demographic details, DASS score to identify percentage of student having depression, anxiety and stress and PSQI score for good and poor quality of sleep were described in frequency. The study participants were compared for gender, age, current living place and year of study using Chi-squared tests for quality of sleeping. A value of p<0.05 at confidence level of 95% was consider statistically significant for analyses.
RESULTS Of the total 415 students enrolled for second to third year of medical graduation at the medical course, 69.63% (n=289) answered the complete questionnaire, comprising 100 (34.72%) of second year, 91 (31.60%) of third year part 1, and 97(33.68%) of third year part 2 medical students. From the Socio-demographic profile, all the students were in the age group of 18 to 25 years of age, with predominance of 20 to 21 year of age group (44.29%). Females were fairly higher compared to males (52.43% vs 47.92%). Of the total 289 students, majority (81.31%) were currently living in the hostel. Among 289 medical students, 76 (26.30%) reported poor sleep quality. Table 1: Socio-demographic characteristics of study participants
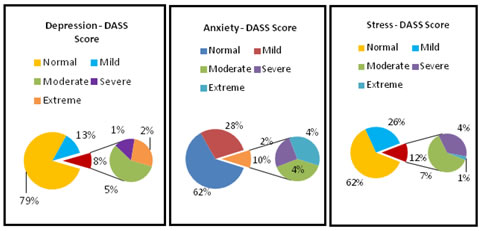
Figure 1: Prevalence of Depression, Anxiety and Stress among study participants according to DASS Score With concern to the prevalence of depression, anxiety, and stress, as weighed by the DASS-21 score, 21% had depressive symptomatology (3% severe or extremely severe), 30% had anxiety symptoms (6% severe or extremely severe), and 33% had stress symptoms (5% severe or extremely severe).
Table 2: Association between various socio-demographic profile and quality of sleep
The Non-parametric chi square test revealed that females had higher chance of having poor quality of sleep (28.48%) compared to counter study part; but the result was not statistically significant(p>0.05). Apart from this, other study variables, as instance, second year MBBS students (35.00%), students who were living in rental house (30.00%), students who require more than 30 minutes of time to fall asleep (50.00%), students whose usual time to go to bed is more than 2:00am (52.38%) and who spend less time in bed were more prone to have poor quality of sleep(52.78%) associated with poor sleep quality and the result was also statistically significant (<0.05).
DISCUSSION Core findings of current study: Sufficient sleep has a crucial role in augmenting cognitive skills especially memory preservation. Poor night time sleep quality and the consequent daytime sleepiness affect physical and cognitive health of students and their academic performance. Looking this concern, PSQI score of < 5, were found in 26.30% of the study participants, which indicate one in four medical students had significant poor sleep quality. From validate DASS score questionnaire, study result revealed that one in thirteen, ten and eight medical students suffering from moderate to extreme severe range of depression, anxiety and stress respectively. Study comparison with past literature: The magnitude of depression among medical students in the current study (21%), which was lower than the found in study conducted in Ethiopia(51%). 6 Even though Found Prevalence is low in compare to the study done in other part of India, in which prevalence of depression of 51%10 and 49.1%11. However, the current study result is in line with the study conducted in Addis Ababa University (Ethiopia) which were 27.7%.12 The study revealed that the prevalence of anxiety was (38%). Regarding the prevalence, the current study’s finding was similar to other studies carried out in Ethopia (30.1%)6 and with other study conducted in Brazil (33.7%)13. Contrarily the occurrence of anxiety in the recent study was higher than found in the studies conducted in India (9.8%)14, and Nepal (5%)15. The magnitude of stress among medical students in the current study was 38%. Even though it was high, few studies reported even higher percentage (74% and 90%) of stress among medical students.16,17 Low prevalence of mental health problems is a good signs of our institute and can be attributed due to various students supportive programs (mentorship program, extracurricular activity etc.) of the institutes. The global PSQI score shows a 26% of study participants was having disturbance of sleep; in the line with the study conducted at Saifai, Etawah(27%)18. Other studies also support this findings19,20. In this study better sleep quality is found in the same proportionate of male and female members which is contrary to finding of study conducted in Loni, Maharashtra where females have better sleep quality than the males.21 Sleep duration of less than 7 hours was observed in (72/289) 24.91% of medical students in the current study; which is lower than the finding observed in the study conducted in Saifai, Etawah (60%)18. Nearly 15.91% of medical students spend more than 30 minutes of time in the bed to sleep; which was less than the found in the study conducted in Saudi Arabia (51.5%)22. In the current study, associated factors for having poor quality of sleep were female gender(28.48%), second year of MBBS(35.00%), rental place of stay(30.00%), >30 minutes of time spend in a bed to sleep(50.00%), students who get in the bed after 2 am midnight(52.38%), and who spend less than 7 hours in the bed (52.78%). Unfortunately, researcher of current study was unable to find comparable data for above associated parameters. So, this can be serving as first of its kind data for future references.
LIMITATIONS Underreporting of the Depression, Anxiety and Stress condition and Poor sleep problem cannot be ignored in the current study; as students hide their condition and may give socially anticipated answers. This study belongs to the students of private medical college only; we cannot replicate our results to the students who are in government medical colleges.
CONCLUSION Though the less compared to other study but, depression, anxiety, stress and poor sleep quality among medical students is the emerging public health problem. The common anticipated reasons for this situation are family’s expectation, exam pressure, extensive long course, fear of pacing into the real world of medicine, and dissatisfaction with the administration etc. This profession is highly demanding and requires utmost focus and expertise. There is a desperate requirement to take measures to enhance the mental health of medical students who will be the future rescuers of health. Appropriate actions to reduce depress, anxiety and stress and improve sleep quality, include mentorship program, students support program, students engage in extracurricular activities to revitalize them and to include students friendly education and evaluation process.
ACKNOWLEDGEMENT The study was conducted as a part of Evidence Generating Community Health Projects (EviGenChiP) program of Sumandeep Vidyapeeth. We like to thank the Dean, SBKS MIRC and EviGenChiP program coordinators for providing opportunity and platform to conduct a research.
REFERENCES
Policy for Articles with Open Access |
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
 Home
Home