Official Journals By StatPerson Publication
|
Table of Content - Volume 4 Issue 1 - October 2017
A study of FEV1 in relation to body mass index among smokers
L K Sudeer Kumar
Associate Professor, Department of Physiology, Mount Zion Medical College, Chayalode, Adoor, Kerala, INDIA. Email: pramoddr2012@gmail.com
Abstract Background: FEV1 is the most specific and dependable measure of airway obstruction. Because of the reliability and simplicity of equipment needed to measure FEVI this parameter is used most frequently to measure bronchial hyper-responsiveness. Reduction in FEVI reflect the total effects of reduction in TLC, obstruction of airway, loss of lung recoil and relatively uncommon gross weakness of respiratory muscles. Methodology: First, case history is taken with special emphasis on personal habits. Then secondly the physical examination including the measurement of height and weight. All the tests are done at the same time of the day to avoid possible diurnal variation. Subject is allowed to sit comfortably on the stool. Instructions are given about the tests. A very enthusiastic demonstration by the operator is required. So that a maximum effort is made by the subject when carrying out the forced expiratory test. Subjects who has not previously examined on spirometry should have two or more practice attempts until it appears that maximum effort is being obtained. Results: In smokers, the smokers with normal weight the mean are 54.85 and the standard deviation is 26.42. In smokers with overweight the mean is 51.94 and the standard deviation is 22.47. When this values are tested using chi-square test, it is found that there is significant difference, according to the chi-square test the P value is less than 0.05 Conclusion: The effect of smoking on FEV1 is more affected in overweight group of subjects than the normal weight group of subjects. Key Words: FEV1, Smoking, BMI.
(FEV1) Is the volume of air exhaled in the specified time during the performance of FVC maneuver, for example FEV1 is the volume of air exhaled during the 1st second of FVC. It can be expressed either as an absolute volume i.e. as FEVI or as a percentage of the FVC i.e. as FEV1/FVC%. FEV1 is the most specific and dependable measure of airway obstruction. Because of the reliability and simplicity of equipment needed to measure FEVI this parameter is used most frequently to measure bronchial hyper-responsiveness. Reduction in FEVI reflect the total effects of reduction in TLC, obstruction of airway, loss of lung recoil and relatively uncommon gross weakness of respiratory muscles. FEVI is mainly used to asses intrathoracic airway obstruction, either in clinical practice or in epidemiological surveys in COPD (Chronic Obstructive Pulmonary Diseases), the level of FEV1 is linked better to prognosis than any other single test of lung function. The normal value of FEVI /FVC % is more than 80, although this value does fall somewhat with advancing age. A study by Gilbert R et al revealed that FEV1/FVC% has a sensitivity of 0.82 and a specificity of 0.98 for diagnosis of airway obstruction. As the specificity is so high less precise clinical information is required.1,2 Assessment of pulmonary function while air was flowing into, or out of the lung began only in 1933 when Hermannsen first proposed the test now known as the maximum voluntary ventilation (MW). But this did not gain wide spread use until Cournand and Richards developed regression equations to predict normal values. In 1955 Leuallen arid Fowler introduced measurement of the average rate of air flow during the middle half of a Forced expiratory vital capacity. The earliest systematic attempt to use the peak flow rate as a physiological index was that of Hadorn who measured the flow rate on expiration by means of an anaeroid manometer connected across a simple orifice. Wyss. Fused the same type of orifice as Hardorn, but recorded the pressures photographically. This gave a permanent record and a higher frequency response. Determination of these indices of dynamic lung function is now generally part of the battery of tests-static and dynamic included under the designation Spirometry. In the first half of this century, progress in developing, methods for pulmonary function testing was slow. In the 1950's pulmonary physiologists quickly turned to take advantage of the opportunities afforded by the rapidly increasing field of electronics and the widespread application of transducers and computers, and the methods have become more complex and sophisticated. The respiratory system includes the lungs, the regulatory center in brain, the chest wall and the pulmonary circulation.3 The 4 major components that support the function of respiration are ventilation, diffusion, perfusion and control of breathing. Any disorder may affect one or more of these functional components. Although, a carefully elicited history, proper physical examination and chest radiography can often establish a diagnosis in an individual patient, testing of lung function has become a standard practice in the evaluation and care of patients with various cardio respiratory disorders. Pulmonary function tests (PFT) are done to, entity and quantify the disturbances in respiratory functions. Analytical And Non Analytical Factors Influencing PFT Certain, analytical factors as well as the non-analytical factors must be taken into account to accomplish the true goal. Non-analytical factors include anxiety on the part of the patients. The performance of these test require co-operation and understanding. Worry and uncertainty can exert impact on the performance of the subject. Use of explanatory sheaths or descriptive brochures can reduce this apprehension. A patient who is fatigued or in pain should be alleviated of these symptoms, if possible, before the beginning of the test. Medication taken by the patient before PFT can significantly affect the outcome e.g; bronchodilators should be discontinued before testing. A major non-analytical cause for misinterpreting results is the in appropriate use of data obtained else where from a different patient population, as "control" values. Analytical factors include chances of error with the equipment, techniques and calculations. To help in achieving accuracy, reproducibility and comparability, attempts at standardization have been initiated on a global scale. Guidelines have been developed for valid determination of the Forced Vital Capacity (FVC), the number of attempts required, acceptable, variability efforts and criteria for judging reliable data. The major objective of a Pulmonary Function Lab should be provide accurate and timely results of lung function tests.4,5 For the sake of quantification and comparison, the total volume of gas in the lungs is conventionally subdivided into compartments (volumes) and combinations of two or more volumes (capacities). Tidal volume (TV), Inspiratory reserve volume (IRV), Expiratory Reserve volume (ERV) and Residual volume (RV) are the 4 static volumes. Inspiratory Capacity (IC), Vital Capacity (VC), Functional Residual Capacity (FRC) and Total Lung Capacity (TLC) are the capacities. VITAL CAPACITY VC is the largest amount of air that can be expired after a maximal inspiratory effort. Expressed in liters (BTPS). VC can be measured as: 1. The volume expired from TLC to Residual Volume (RV) during a forced expiration (FVC) or a slow maneuver (relaxed maneuver) 2. As the volume inspired from RV to TLC. 3. As the sum of inspiratory capacity (Volume inspired from FRC to TLC) and the expiratory reserve volume. In healthy subjects, all these methods give similar results; but the value of VC is much more dependent on the technique used when there is airway obstruction. In general, inspiratory vital capacity gives the largest values. Usually 'Vital Capacity' refers to the expiratory VC unless otherwise specified. It is usually measured slowly from a position of maximum inspiration to full expiration (Slow Vital Capacity — SVC). VC gives useful information about the strength of the respiratory muscles and other aspects of pulmonary functions. Decrease in VC can be caused by loss of lung tissue, example; - lobotomy, space-occupying lesions (tumors), fibrosis. VC is often reduced in obstructive lung diseases. Other causes of a decreased VC are, depression of the respiratory centers or neuromuscular diseases, reduction of available thoracic space (pneumothorax, cardiac enlargement) and limitations of thoracic (kyphoscoliosis) or diaphragmatic (pregnancy, ascites) movements. Normal values: -4-5 L in Males, 3-4 L in Females VC was one of the earliest lung volumes to be measured Since then, various studies on VC have been conducted relating the volume to various physical parameters like body, surface area, calculated thoracic volume, sitting height standing height body weight.6 At first a thorough physical examination was carried out and also make sure that patient had not taken cigarette or heavy meals at least an hour prior to the test. Selection of Tests: When choosing tests for lung function a number of criteria should he taken into account.
So the tests were selected with a view for pointing information on different aspects of function. Procedure: First, case history is taken with special emphasis on personal habits. Then secondly the physical examination including the measurement of height and weight. All the tests are done at the same time of the day to avoid possible diurnal variation. Subject is allowed to sit comfortably on the stool. Instructions are given about the tests. A very enthusiastic demonstration by the operator is required. So that a maximum effort is made by the subject when carrying out the forced expiratory test. Subjects who has not previously examined on spirometry should have two or more practice attempts until it appears that maximum effort is being obtained. A disposable mouthpiece should be used in each subject. The mouthpiece was positioned so that the subject's chin was slightly elevated and neck extended. After the insertion of mouth piece a careful check was made to ensure that there was no air leak present. The subject was asked to make maxima! effort for each test and was closely watched to ensure that he maintained an airtight seal between the lips and the mouthpiece of the instrument. First the subject data was entered as name, age, sex, height, weight, address, occupation, addiction etc. Then the required measurement was called up from menu. Forced Vital Capacity (FVC) The subject is made comfortable and the nose clip kept in place to close the nostril to prevent air entry through the nose. Then the mouthpiece is placed in the mouth and which is connected to pneumotach. Then the subject is asked to breach via, the mouthpiece. After a brief period of quiet normal breathing subject is asked to breathe in and completely as possible then suddenly breathe out forcefully, rapidly and completely as much as possible. The performance of the maneuver was evaluated by inspecting the graphic output of flow volume curve and the subject was reinstructed if necessary. Repeat it for 2 to 3 times. Measurement was taken from the best of the three tests. RESULTS
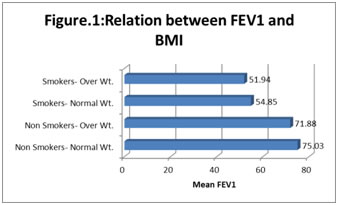
Table 1: Relation between FEV1 and BMI
Figure 1:
As per the table non-smokers with normal weight is having meanFEV1 of 75.03 with a standard deviation of 20.89 and non-smokers with overweight the mean is 71.88 and standard deviation is 18.13. These values are tested using chi-square test and it is found that the difference actually observed does not have significance since the p value is more than 0.05. In smokers, the smokers with normal weight the mean are 54.85 and the standard deviation is 26.42. In smokers with overweight the mean is 51.94 and the standard deviation is 22.47. When this values are tested using chi-square test, it is found that there is significant difference, according to the chi-square test the P value is less than 0.05 and it shows that the effect of smoking on FEV1 is more affected in overweight group of subjects than the normal weight group of subjects. DISCUSSION The pulmonary function tests were conducted in 200 people in the Respiratory Medicine Laboratory, and the values were analyzed statistically using software package. The PFT values analyzed are FVC, FEV1, FEF, FEV1/FVC and FEF 25- 75%. The present study has confirmed the result of earlier researchers who observed impairment of lung function in obese individuals when compared to normal v:eight subjects. The present study has also undoubtedly revealed a significant reduction in pulmonary functions among over weight individuals when compared to normal weight individuals in the smoking group and in the nonsmoking group. Obesity has an adverse effect on pulmonary function and it is associated with a number of pulmonary abnormalities. It has been proved that obesity is not directly related to respiratory disease. Obesity reduces pulmonary compliance, increases airway resistance, and reduces the small airway caliber, which in turn increases the risk of respiratory disease in smokers.7 Thus this study has proved that the obesity is an independent parameter, which can impair lung function in smokers as well as nonsmokers. The study also show that smoking and obesity when present concurrently greatly reduces the lung function. The observations of the present study implicate the need to normalize body weight in patients with compromised respiratory function and to stop smoking if they are smokers. A global long-term prospective study of the effect of obesity on lung functions, involving various races, measurement of compliance, work of breathing and measurement of airway resistance is a need of this era, because obesity is a global health problem affecting developed as well as developing nations. We hope the present study will be a small step, which would inspire the giant leap in the near future. Statistical analysis of the observation between smokers with normal weight and smokers with overweight show that there is significant reduction of spirometric measures such as FVC, FEV1, FEF, FEV1/FVC and FEF 25-75% in overweight smokers compared to normal weight smokers. This reduction could be due to the physiological changes in the respiratory system due to the obesity and sedentary life style of the overweight subjects in addition to smoking. Statistical analysis of the observation of the present study showed that there is significant reduction of FVC, FEV1, FEF, FEV1/FVC and FEF25-75% in over weight nonsmokers when compared to normal weight nonsmokers. Thus, among smokers as well as nonsmokers over weight subjects showed a statistically significant association with impairment of respiratory function as evidenced by spirometric study. The obese subjects are categorized under people who are doing physiological changes in sedentary works. This may leads to various the respiratory system like reduced pulmonary compliance, rise airway resistance and reduces small subjects.8
CONCLUSION The results of present study showed that there was a significant reduction of FEV1 in over weight smokers when compared to normal weight smokers. The reduction of FEV1 in over weight smoker is also statistically significant.
REFERENCES
|
|
 Home
Home