Official Journals By StatPerson Publication
|
Table of Content - Volume 4 Issue 1 - October 2017
FEV1/FVC among smokers and non smokers: A comparative study
L K Sudeer Kumar
Associate Professor, Department of Physiology, Mount Zion Medical College, Chayalode, Adoor, Kerala, INDIA. Email: pramoddr2012@gmail.com
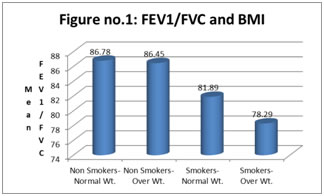
Abstract Background: Respiratory Physiological changes in obesity are decreased overall compliance, increased airway resistance and shallow breathing pattern. These changes are due to increased intra abdominal pressure, decreased chest wall expansion, reduced small airway caliber and adaptation to the increased load. Methodology: The study was conducted at department of TB and chest diseases, medical college. Tests were carried out in the laboratory and these tests were done in chronic smokers who attend in the smoker's clinic at morning hours. Here pulmonary function test are done using spirometry. Results: In smokers, the smokers with normal weight the mean is 81.89 and the standard deviation is 23.10. In smokers with overweight the mean is 78.29 and the standard deviation is 21.61. When these values are chi-square test, it is found that there is significant difference, according to the chi-square test the P value is less than 0.05 Conclusion: The effect of smoking on FEV1/FVC is more affected in overweight group of subjects than the normal weight group of subjects. Key Words: FEV1/FVC, Overweight, Spirometry.
Obesity is measured using "BODY MASS INDEX" (BMI). There was a study of pulmonary functions tests in relation to body mass index (2001) from the Arizona Respiratory Center, University of Arizona, Tucson. They found that except emphysema all other respiratory diseases are more in obese/overweight people. Ray et al also found that obesity affects pulmonary function by lowering many spirometric measures. The risk of pulmonary diseases are two times more in obese person who smoke than in smokers with normal weight. The effects of smoking in obesity on respiratory system are reduced pulmonary compliance, increased work of breathing, increased minute volume, decreased total lung capacity and decreased functional residual volume. Based on these observations, an attempt has been made to study the pulmonary function tests in smokers in relation to body mass index and comparing these results with non-smokers in relation to body mass index.1 Obesity may be defined as an abnormal growth of the adipose tissue or increase in the fat cell number or combination of the both. Overweight mean weight in excess of the average for a given sex, height and age. Obesity is the one of the most significant contributors to ill health. It is the key risk factor for chronic and non-communicable diseases. It has been estimated to affect 30-40 percent of adults and 10-20% of children in developed countries.2 The etiology of obesity are: - Age, Sex, Genetic factor, physical inactivity, Socio economic status, eating habit, familial tendency and endocrine factors. Assessment of Obesity Obesity can be assessed by Body Mass Index (BMI). It is the measurement of body fat. It is a simple index of weight for height; it is commonly used to classify overweight and obesity in adult. BMI is calculated as the weight in kilograms divided by the square of the height in meters. For example, an adult who is 80 kg in weight and 1.7 meters in height BMI=80Kg/i.7m2 =NW- c21. 7 Normal range is 18.5-2IP Below 18.5 is underweight and above 25 is overweight This BMI is widely accepted. Other methods used are skin fold thickness and waist circumference and waist: hip ratio Hazards of Obesity is a positive risk factor of diabetes, hypertension and coronary artery disease, moderate risk factor for osteoarthritis, gallstones and other several diseases. Numerous studies also suggested that, it directly affects respiratory system and by lowering some of the spirometric measures. Respiratory Physiological changes in obesity are decreased overall compliance, increased airway resistance and shallow breathing pattern. These changes are due to increased intra abdominal pressure, decreased chest wall expansion, reduced small airway caliber and adaptation to the increased load. Respiratory Effects of obesity are dysponea and exercise intolerance, bronchial asthma, rapid shallow breathing. Sin D.D. et al., suggested that obesity also associated with obstructive sleep apnea, obesity hypoventilation syndrome, hypoxaemia and pulmonary hypertension. PFT in Obesity Recently studies suggested, many measures of PFT declines in obesity. Especially measures such as FEV1, FVC, FEV1/FVC, MW, ERV and FRC are reduced. VC and TLC are preserved. The pulmonary function values in obesity found lower values such as FEV1, FVC, FEV1/FVC and FEF. Obesity showed low PFT values such as FVC, FEV1, FEV1/FVC, MW, FRC and FVC. It suggested that even in the absence of obstructive or restrictive lung diseases, obesity affects the respiratory system.3,4 Effect of Smoking and Obesity in Respiratory System Ewing M.S. et al., 1997 done PFT in obese smokers and he found that the PFT measures such as FVC, FEV1, ERV, FRC and FEF 25-75% were significantly reduced. In 2002, A.M.Li et al. found reduced ERV, FVC, FEV1, FEF25-75% and MW of PFT values in obese smokers. In 1997, A.M.J. Respir 1997 found that there was significant reduction in the PFT values such as FVC, FEV1, FEF 25-75%, FEF, FEV1/FVC and MW in obese smokers.
MATERIAL AND METHODS The study was conducted at department of TB and chest diseases, medical college. Tests were carried out in the laboratory and these tests were done in chronic smokers who attend in the smoker's clinic at morning hours. Here pulmonary function test are done using spirometry. The tests done are FVC, FEV1, FEF, FEV1/FVC and FEF25-75%. These studies were done to find out the effects of smoking on lung function tests by comparing smokers with non-smokers in relation to body mass index. The tests are done by selecting chronic smokers of different age group from 30-70 years from outpatient, and impatient from the department of TB and chest diseases, medical college. Control groups are selected from patient who does not smoke. The instrument used was a portable small-computerized. Here mouthpiece is attached to resistant pneumatochograph, which contains parallel rows of resistant wire. Airflow through these procedures a pressure gradient across the resistant element, which is converted to electrical, signal and measured by the computer system. Results were displayed on the screen. This can be printed on an electro sensitive paper for a permanent record. The test was done in 100 subjects and another100 as control. The subjects were chronic smokers and then they are divided into two groups as
The control arenon smokers and also they were divided into two groups:-
RESULTS
Table 1: Statistical analysis of FEV1/FVC
Figure 1:
As per the table non-smokers with normal weight is havingmean FEV1/FVC of 86.78 with a standard deviation of 17.89 and non-smokers with overweight the mean is 86.45 and standard deviation is 16.37. This values are tested using chi-square test and it is found that the difference actually observed does not have significance since the p value is more than 0.05. In smokers, the smokers with normal weight the mean is 81.89 and the standard deviation is 23.10. In smokers with overweight the mean is 78.29 and the standard deviation is 21.61. When this values are chi-square test, it is found that there is significant difference, according to the chi-square test the P value is less than 0.05 and it shows that the effect of smoking on FEV1/FVC is more affected in overweight group of subjects than the normal weight group of subjects.
DISCUSSION Comparison of PFT between smokers and nonsmokers, in relation to BMI Statistical analysis of the observations of the present study showed that there is significant reduction of spirometric parameters such as FVC, FEV1, FEF, FEV1/FVC and FEF25-75% in overweight subjects (smokers and nonsmokers). The reduction observed in all parameters were more significant in overweight smokers compared to normal weight smokers than the reduction observed in overweight nonsmokers as compared to normal weight nonsmokers. This is because of the addictive effects of smoking as well as overweight on the respiratory system in this group of subjects. Obesity is not directly related to respiratory diseases but increases the risk of respiratory diseases in smokers. The sedentary habit of overweight individuals may contribute to the impairment of pulmonary function.5 The obese subjects are categorized under people who are doing sedentary works. The sedentary life style and obesity causes many physiological changes on respiratory system by reducing respiratory compliance, increase airway resistance and reduces small airway caliber. This in turn leads to various types of respiratory diseases. This study reveals that moderate type of respiratory exercise needed for proper maintenance of respiratory compliance, This can be achieved by decreasing the body weight and by doing regular physical exercise or by decreasing the body weight and by doing simple respiratory exercise (example Yoga). In the present study it was observed that the reduction in FVC, FEV1, FEF, FEV1/FVC and FEF25-75% in obese smokers as compared with non-obese smokers were statistically significant than the reduction in these parameters in obese nonsmokers as compared with normal weight nonsmokers. This indicates there is a synergistic harmful effect of obesity in the presence of smoking. There are many previous studies on PFT in smokers in relation to obesity. They also proved that smoking with obesity reduces pulmonary function two times more than that of non-smokers with obesity. Biring M.S et.al, 1997 proved that PFT measures such as FVC, FEV1, FEE 25-75%, ERV and FRC were significantly reduced in obese smokers. In another study it was found that there was significant reduction in the PFT values such as FVC, FEV1, FEF 25-75%, FEF, FEV1/FVC and MW in obese smokers. A.M.Li et.al, in 2002 found reduced ERV, FVC, FEV1, FEF 25-75% and MW of PFT values in obese smokers. Sterfano Gueriaet. al, on 2002 found that obesity and smoking increases the risk of asthma.6 The present study also substantiates the views of the above workers. All the pulmonary function parameters analyzed in the present study were found to be significantly reduced in obese smokers compared to nonobese smokers.
CONCLUSION The statistical analysis of the present study showed that there was significant reduction of FEV1/FVC in over weight smokers when compared to normal weight smokers. The reduction of FEV1/FVC observed in over weight smokers is statistically significant. FEF 25-75%: The results of present study showed that there was a significant reduction of FEF 25-75% in over weight smokers when compared to normal weight smokers. The reduction of FEF 25-75% in over weight smoker is statistically significant.
REFERENCES
|
|
 Home
Home